
Double-bar technique for the correction of asymmetric pectus excavatum
Highlight box
Key findings
• Patients who underwent the double-bar technique had a significant benefit in asymmetric degree without compromising improvement in the Haller index.
What is known and what is new?
• Minimally invasive repair of pectus excavatum (PE) is the most commonly performed procedure for correcting chest wall deformities. Parallel and crossbar techniques have demonstrated similar effectiveness.
• This study evaluates the double-bar technique and its benefits in improving asymmetry.
What is the implication, and what should change now?
• The double-bar technique may be a promising option for correcting asymmetric PE, and further studies are needed.
Introduction
Background
With the introduction of minimally invasive repair of pectus excavatum (MIRPE), pectus excavatum (PE) surgery has improved substantially. Thoracic surgeons have recognized the feasibility and safety of this procedure, and MIRPE has become the most commonly performed procedure for correcting chest wall deformities.
Multiple-bar insertion is currently used to correct chest deformities at multiple rib levels. Our previous study compared parallel and crossbar techniques, both of which demonstrated similar effectiveness (1). Hyun et al. also reported the benefits of the crossbar technique for the correction of more rigid and complex PE (2). While they did address the correction of asymmetry, only a limited number of studies have specifically focused on patients with this condition.
Rationale and knowledge gap
Asymmetry in patients with PE remains as an important postoperative issue. Although an improvement in the Haller index (HI) has been achieved, a considerable number of patients complain of persistent asymmetry (3). Several procedures have been employed to improve asymmetry after MIRPE, such as the morphology-tailored bar-shaping technique (3,4), proximal insertion of the introducer (5), and Wang’s procedure, which pulls and fixes the depressed portion using inserted bars at subcutaneous or muscular levels (6). However, these techniques have not yet been universally accepted, and there are still areas that need improvement.
In 2018, Song et al. suggested a double compression and complete fixation bar system as a new approach for correcting PE (7). It has several advantages in terms of operative time and incidence of hospital complications. The system has also been applied to patients with complex PE and carinatum, demonstrating promising results (8).
Therefore, we investigated this technique, described as the double-bar technique, to evaluate its benefit in improving asymmetry. Additionally, we introduced several radiological parameters that are easily measurable and reproducible in different hospitals.
Objective
This study aimed to investigate the double-bar technique and its chest wall asymmetry-improving benefits in patients with PE. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1650/rc).
Methods
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional board of Gangnam Severance Hospital, Yonsei University College of Medicine (No. 3-2023-0164, approval date 07/03/2023), and the need for individual consent for this retrospective analysis was waived.
Participants
This retrospective study included patients who underwent PE surgical correction between January 2017 and December 2021. Of the 190 patients, we only included those with available pre-and postoperative computed tomography (CT) images (n=79).
Radiologic indices and evaluation
Axial CT was used to assess the severity and asymmetry of the patients with PE (Figure 1). HI was defined as the ratio of the transverse and vertical diameters at the most depressed point of the chest wall. Asymmetric degree (AD) was calculated as the percentage of the difference between the bilateral apicoposterior diameters divided by the larger apicoposterior diameter. An AD >5% was considered to indicate an asymmetric chest wall shape. Sternal rotation angle (SRA) was measured as the angle between the horizontal line and the line parallel to the sternal surface at the closest point of the maximally depressed lesion. A SRA >10° was considered to indicate severe rotations.
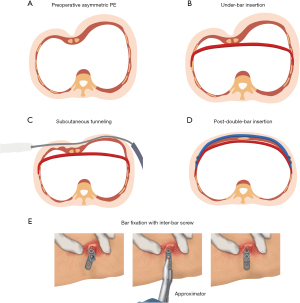
Surgical procedure: double-bar technique
Surgery was performed under general anesthesia with single-lumen endotracheal tube intubation. Surgical draping was performed with the patient in the supine position and both arms outstretched. After marking the deepest point and planning the number of bars to be inserted, the sternum was sutured with a wire and elevated using the crane technique. Starting in 2021, we introduced cryoanalgesia of intercostal nerves using Argon gas (−80 ℃). Cryoanalgesia was performed at the bar insertion level, including one or two upper and lower levels, via the VATS approach with 12- and 5-mm trocars. After cryoablation, a passer was inserted from the left side under right-sided thoracoscopic inspection. Figure 2 shows each step of the double-bar insertion procedure. A bar under the chest wall was inserted along the path through a passer inserted using chest tubes, which was then rotated into place. A second bar was inserted subcutaneously above the chest wall and a second passer was used to track the second bar. These two bars were fixed with a screw, and an approximator was used to prevent bar rotation. If an additional bar was inserted at the upper level, it was fixed using bridge plates. A hemovac was inserted, and the wound was closed. Figure 3 shows the postoperative chest X-ray after the double-bar insertion.
Terminology for pectus surgery
Following terminology were used to describe different techniques of MIRPE.
- Double-bar technique: insertion of presternal bar parallelly above the retrosternal bar fixing each other;
- Sandwich technique: insertion of presternal bar obliquely between two retrosternal bars, which were inserted in parallel manner;
- Cross-bar technique: insertion of two retrosternal bars which were crossed each other;
- Parallel-bar technique: insertion of two retrosternal bars parallelly.
Follow-up protocols
Patients were followed up within 2 weeks of discharge. The patients visited the outpatient clinic at 3, 6, and 12 months post-surgery. Follow-up CT evaluation was usually performed 6 months after surgery. The bars were removed between 24 and 36 months after surgery.
Statistical analyses
For continuous variables, data are presented as medians and interquartile ranges due to their non-normality, and the Mann-Whitney U test was performed for the analysis. The Fisher’s exact test was used to analyze categorical variables. Differences in the parameters before and after surgery were compared according to the type of bar technique used. For the subgroup analysis of patients with preoperative asymmetric PE, propensity score matching was applied to minimize the impact of confounding variables on the severity of asymmetry. The propensity score for each participant was calculated using a logistic model that included age, sex, and AD. Statistical analyses were performed using R version 4.0.4 (R Core Team, R Foundation for Statistical Computing, Vienna, Austria). Differences were considered statistically significant at a two-tailed P value <0.05.
Results
Clinical and procedural characteristics according to bar insertion techniques
The demographic and procedure-related parameters between the double-bar and the non-double-bar groups are presented in Table 1. Patients in the double-bar group were younger than those in the non-double bar group (P=0.001), representing a recent trend of early surgical intervention for patients with PE. Surgical outcomes such as hospital stay and postoperative pain score were superior in the double-bar group, which may have been related to the introduction of cryoanalgesia for the intercostal nerves. In the non-double-bar group, either the cross (28/56, 50.0%) or parallel bar (25/56, 44.6%) technique was used. There were no differences in the development of postoperative complications, such as wound infection (n=2), pneumothorax (n=2), or pleural effusion (n=1). No patient experienced bar rotation or mortality.
Table 1
| Variables | Double (n=23) | Non-double (n=56) | P value |
|---|---|---|---|
| Sex | 0.12 | ||
| Female | 7 (30.4) | 8 (14.3) | |
| Male | 16 (69.6) | 48 (85.7) | |
| Age (years) | 13.1 [8.1, 14.9] | 16.2 [13.5, 20.0] | 0.001 |
| BMI (kg/m2) | 17.0 [15.0, 18.0] | 18.0 [16.0, 20.0] | 0.04 |
| Comorbidity† | 7 (30.4) | 8 (14.3) | 0.12 |
| Operative procedures | |||
| Regional pain control | <0.001 | ||
| Cryoablation | 16 (69.6) | 0 (0.0) | |
| Epidural PCA | 0 (0.0) | 5 (8.9) | |
| ON-Q‡ + IV-PCA | 1 (4.3) | 12 (21.4) | |
| IV-PCA | 6 (26.1) | 39 (69.6) | |
| Bar insertion techniques | <0.001 | ||
| Cross | 0 (0.0) | 28 (50.0) | |
| Double (± parallel) | 23 (100.0) | 0 (0.0) | |
| Parallel | 0 (0.0) | 25 (44.6) | |
| Single | 0 (0.0) | 3 (5.4) | |
| Pain score (VAS) after surgery | |||
| 3 hours after surgery | 4.5 [4.0, 5.8] | 7.0 [4.0, 8.0] | 0.056 |
| 12 hours after surgery | 3.5 [2.0, 5.0] | 5.0 [4.0, 6.0] | 0.03 |
| 48 hours after surgery | 2.0 [1.0, 3.0] | 3.0 [2.5, 4.0] | 0.04 |
| MME during hospitalization (mg) | 8.5 [0.0, 22.5] | 32.3 [22.2, 71.9] | 0.002 |
| Hospital stay (days) | 4.0 [4.0, 5.0] | 6.0 [5.0, 6.3] | <0.001 |
| Complication§ | 2 (8.7) | 3 (5.4) | 0.63 |
Data are presented as n (%) or median [interquartile range]. †, includes cardiovascular, genetic (Marfan syndrome), or respiratory diseases. ‡, ON-Q pump (ON-Q PainBuster®, ref. PS6505; I-Flow Corp., Lake Forest, CA, USA) is designed to deliver local anesthetics to surgical sites for non-narcotic pain relief. §, two wound infections in the double bar group; one pleural effusion and two pneumothorax development in the non-double bar group. BMI, body mass index; PCA, patient-controlled analgesia; IV, intravenous; VAS, visual-analogue scale; MME, morphine milligram equivalent.
Changes in radiologic parameters according to bar insertion techniques
The three preoperative radiologic indices (HI, AD, and SRA) were not significantly different between the two groups. However, there were remarkable changes in several factors after the surgery (Table 2). Although the change in HI was not statistically significant (P=0.06), the non-double-bar group tended to have an overcorrection of PE (double bar, −1.17; non-double bar, −1.41). Importantly, the change in AD was significantly greater in the double-bar group than in the non-double-bar group (double, −1.50%; non-double-bar, −0.49%, P=0.009) (Figure 4). Furthermore, more patients with a symmetric chest wall shape were observed in the double-bar group after surgery (P=0.057).
Table 2
| Variables | Double (n=23) | Non-double (n=56) | P value |
|---|---|---|---|
| Preoperative radiologic parameters | |||
| HI | 3.87 [3.38, 4.33] | 4.06 [3.57, 4.66] | 0.41 |
| AD (%) | 4.27 [0.93, 12.15] | 3.87 [1.74, 7.28] | 0.50 |
| AD | 0.33 | ||
| Asymmetric† | 11 (47.8) | 20 (35.7) | |
| Symmetric | 12 (52.2) | 36 (64.3) | |
| SRA (°) | 11.2 [4.9, 15.1] | 8.6 [0.0, 14.6] | 0.46 |
| Postoperative radiologic parameters | |||
| HI | 2.65 [2.40, 3.14] | 2.49 [2.34, 2.87] | 0.26 |
| AD (%) | 2.29 [0.88, 3.97] | 3.32 [1.92, 5.81] | 0.12 |
| AD | 0.057 | ||
| Asymmetric† | 3 (13.0) | 20 (35.7) | |
| Symmetric | 20 (87.0) | 36 (64.3) | |
| SRA (°) | 2.0 [0.0, 7.6] | 0.0 [0.0, 7.3] | 0.68 |
| Change of HI | −1.17 [−1.46, −0.77] | −1.41 [−1.92, −1.01] | 0.06 |
| Change of AD (%) | −1.50 [−9.51, −0.27] | −0.49 [−3.79, 1.56] | 0.009 |
| Change of sternum-rotation angle | −5.3 [−10.1, −2.2] | −4.8 [−9.0, 0.0] | 0.56 |
| Follow up duration (days) | 489 [118, 720] | 497 [44, 837] | >0.99 |
Data are presented as n (%) or median [interquartile range]. †, asymmetricity was defined as AD 5 or above. PE, pectus excavatum; HI, Haller index; AD, asymmetric degree; SRA, sternal rotation angle.
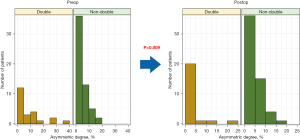
Subgroup analysis: patients with asymmetric PE
To focus on assessing patients with asymmetric PE, a subgroup analysis was performed among those with preoperative AD >5%. Eleven patients in the double-bar and 20 patients in the non-double-bar group were recruited (Table 3). Preoperative demographic variables did not differ between the groups; however, AD was much higher among patients in the double-bar group (P=0.048).
Table 3
| Variables | Double (n=11) | Non-double (n=20) | P value |
|---|---|---|---|
| Sex | >0.99 | ||
| Female | 3 (27.3) | 5 (25.0) | |
| Male | 8 (72.7) | 15 (75.0) | |
| Age at surgery (years) | 13.2 [12.8, 14.7] | 15.6 [13.4, 18.9] | 0.09 |
| BMI (kg/m2) | 17.0 [16.0, 19.0] | 17.0 [15.0, 19.3] | 0.90 |
| Preoperative radiologic findings | |||
| HI | 4.02 [3.83, 4.58] | 4.05 [3.62, 4.64] | 0.97 |
| AD | 13.3 [9.8, 20.6] | 9.3 [7.1, 13.2] | 0.048 |
| Severe rotation (SRA >10°) | 11 (100.0) | 12 (60.0) | 0.03 |
| Change of radiologic parameters | |||
| HI | −1.32 [−1.59, −0.69] | −1.34 [−1.75, −1.03] | 0.48 |
| AD (%) | −9.53 [−12.56, −8.25] | −4.21 [−6.02, −2.77] | <0.001 |
| SRA (°) | −7.3 [−10.9, −5.3] | −6.7 [−9.1, −4.8] | 0.42 |
| Postoperative radiologic findings | |||
| Asymmetric (AD ≥5%) | 2 (18.2) | 12 (60.0) | 0.03 |
| Severe rotation (SRA >10°) | 3 (27.3) | 7 (35.0) | >0.99 |
Data are presented as n (%) or median [interquartile range]. PE, pectus excavatum; BMI, body mass index; HI, Haller index; AD, asymmetric degree; SRA, sternal rotation angle.
Although the change in HI was not different between groups, the difference in AD was more prominent in the double-bar group (P<0.001), and the proportion of asymmetric PE at follow-up was also significantly lower in the same group (P=0.03).
In addition, more patients with severe sternal rotation (SRA >10°) were included in the double-bar group than in the non-double-bar group preoperatively (P=0.03). However, this difference in severe sternal rotation diminished after surgery (P>0.99), indicating a better correction of sternal rotation in the double-bar group.
Subgroup analysis: patients with asymmetric PE with propensity score matching
To minimize the effect of preoperative AD, we matched the AD values and demographic data among patients with asymmetric PE. The characteristics of this particular subgroup are presented in Table S1. In this population, both groups had similar ADs of approximately 10% (10.5% vs. 10.5%, P=0.834). A greater reduction in AD was also observed in the double-bar group (P=0.01). Patients with severe sternal rotation also exhibited better correction using the double-bar technique than others.
Discussion
The landscape of surgical techniques for MIRPE has progressed considerably with the introduction of thoracoscopy, multiple bar insertions, and pain management procedures. While earlier studies juxtaposed diverse methodologies, this study elucidated the benefits of the double-bar technique in ameliorating chest wall symmetry. In this context, we propose using AD and SRA as alternative metrics to assess asymmetry. These radiological assessments offer simplicity and reproducibility, rendering them suitable for widespread adoption and a more objective evaluation of the degree of asymmetry. Moreover, the efficacy of the double-bar technique is substantiated by these assessments. Compared with other multiple-bar techniques, the double-bar approach is superior in rectifying asymmetry.
According to Kim et al., the Nuss procedure has a positive effect on the physical development of patients with PE, although it does not influence the angle of the sternal rotation (9). However, our study revealed a clear improvement in sternal rotation with the double-bar technique, showing a more pronounced effect in cases of asymmetric PE. For individuals with PE, while the procedure aims to assist with correcting depression, rectifying sternal rotation is an important component when considering the correction of asymmetry and accounting for future growth or post-correction appearance. Additionally, as observed in this study, there may be a tendency towards overcorrection in the non-double-bar group. This could potentially lead to the induction of reactive pectus carinatum in situations where sternal rotation correction is insufficient. While the precise influence of the double-bar technique on physiological function in comparison with the non-double-bar approach remains unclear, it is believed to offer major advantages in terms of patient confidence and self-esteem, which are factors closely tied to one’s external appearance.
The double-bar technique is thought to have a more profound effect on correcting sternal rotation and asymmetry than the non-double-bar technique because it simultaneously exerts forces that lift the sternum from below and push it downward from above. According to Hyun et al., chest wall remodeling using the crossbar technique has shown successful outcomes for complex PE (2). However, this surgery (XI fashion) requires substantial experience and is relatively challenging in terms of the technique. In contrast, the double-bar technique used in this study is simpler and less challenging and enables easier manipulation. Additionally, although not explicitly mentioned in the study by Hyun et al. (2), the impact of inserting three or more multibars into the thoracic cavity is unclear. Further research is needed to determine whether or how three or more multibar insertions could affect physiology, such as sternum overcorrection, adhesion to surrounding organs, granulation overgrowth, and respiratory movement. This study is a novel investigation focused on evaluating the extent of asymmetry and sternal rotation, which is believed to have important clinical implications.
Our study had some limitations. First, radiological evaluations were conducted at only one or two levels around the deepest point of the PE. Therefore, the configuration of the entire chest wall may not have been accurately represented. Second, the threshold or cut-off level for asymmetry or severe sternal rotation lacked consensus. The threshold or cutoff level was determined solely based on our dataset, emphasizing the need for subsequent validation prior to widespread adoption. Third, the sample size was relatively modest, and the dataset for the double-bar group was relatively limited. Further follow-up data on patients undergoing double-bar insertion are required to confirm the efficacy of this novel technique.
Conclusions
The double-bar technique may be a promising option for correcting asymmetric PE. Simplified radiologic assessments of AD and SRA can be used to evaluate improvements in chest wall configuration. Further studies are necessary to expand the application of the double-bar technique.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1650/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1650/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1650/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1650/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional board of Gangnam Severance Hospital, Yonsei University College of Medicine (No. 3-2023-0164, approval date 07/03/2023), and the need for individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Moon DH, Park CH, Moon MH, et al. The effectiveness of double-bar correction for pectus excavatum: A comparison between the parallel bar and cross-bar techniques. PLoS One 2020;15:e0238539. [Crossref] [PubMed]
- Hyun K, Park HJ. The Cross-Bar Technique for Pectus Excavatum Repair: A Key Element for Remodeling of the Entire Chest Wall. Eur J Pediatr Surg 2023;33:310-8. [Crossref] [PubMed]
- Park HJ, Jeong JY, Jo WM, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg 2010;139:379-86. [Crossref] [PubMed]
- Park HJ, Lee SY, Lee CS, et al. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg 2004;77:289-95. [Crossref] [PubMed]
- Squillaro AI, Melhado C, Ozgediz D, et al. Minimally invasive repair of asymmetric pectus excavatum: An alternative technique to treating asymmetric morphology. J Pediatr Surg 2022;57:1079-82. [Crossref] [PubMed]
- Wang W, Wang W, Long W, et al. Experience of the Wang procedure in treating pectus excavatum in two hundred fifty-six paediatric patients. Int Orthop 2022;46:2307-13. [Crossref] [PubMed]
- Song IH, Lee SJ, Kim SS, et al. Surgical Outcomes of Double Compression and Complete Fixation Bar System in Pectus Excavatum. Ann Thorac Surg 2018;106:1025-31. [Crossref] [PubMed]
- Song IH, Lee SJ, Lee SY. Repair of pectus carinatum, carinatum/excavatum complex patients with doubly double bar technique. Gen Thorac Cardiovasc Surg 2020;68:1354-6. [Crossref] [PubMed]
- Kim HK, Yoon JY, Han KN, et al. Effect of the Nuss Procedure on the Physical Development of Patients with Pectus Excavatum. Ann Thorac Cardiovasc Surg 2016;22:327-32. [Crossref] [PubMed]




