Uniportal video-assisted thoracoscopic right upper sleeve lobectomy and tracheoplasty in a 10-year-old patient
Introduction
Carcinoid tumors are neuroendocrine lung tumors that occur in 1–2% of all lung cancers, and is even less frequent in the pediatric population. This oncologic disease has a good prognosis when complete surgical excision of the tumor is performed (1).
Given its endoluminal location they are characterized by causing non-specific respiratory symptoms such as cough, hemoptysis and often generate or simulate recurrent respiratory infections with partial improvement delaying the oncological diagnosis (2,3).
Sir Clement Price Thomas proposed implementing bronchial resections since 1947 when he first performed a lobectomy with a bronchial sleeve to resect an adenoma of the right main bronchus. Later in 1955 the surgeons Paulson and Shaw, added the technique known as “bronchoplasty” in bronchial resections (4-7).
During the last decade, different techniques of minimally invasive surgery for bronchial resections have been introduced, among these, the single port (uniportal) video-assisted thoracoscopic surgery (VATS), this being the less morbid and less invasive technique with excellent results in expert hands (8).
In this article a successful sleeve lobectomy in a pediatric patient by uniportal VATS with excellent postoperative results is reported.
Case presentation
A 10-year-old female patient with a 1-year history of clinical symptoms characterized by episodic cough and mild fever was diagnosed of pneumonia so an empiric antibiotic treatment was initially prescribed. The patient showed partial improvement with persistence of cough with a later onset of hemoptysis, with serial smears reported as negative for bacilli identification.
According to the demographic and epidemiological profile of the patient, oral antibiotic management with anti-tuberculosis treatment was prescribed (isoniazid—pyrazinamide—ethambutol—Rifampicin) for 6 months without improvement. She underwent a diagnostic bronchoscopy with biopsy, where a polypoid tumor was seen blocking the entrance of the right upper bronchus (Figure 1A). The result of the biopsy reported a low-grade neuroendocrine carcinoid tumor.
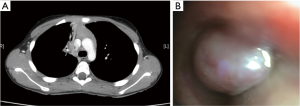
A CT Scan confirmed the presence of endobronchial lesion and secondary atelectasis of the right upper lobe (RUL), without the presence of mediastinal enlarged lymph nodes (Figure 1B).
The patient was proposed for a uniportal VATS right upper sleeve lobectomy.
Surgical technique (Figure 2)
Under general anesthesia and double lumen intubation the patient was placed in a left lateral decubitus position with abduction and flexion of the right upper limb.
A uniportal VATS approach through a 3-cm incision was performed at the 4th intercostal space, anterior axillary line. A 30-degree high definition thoracoscope was inserted through the incision and a panoramic view of the right chest cavity was obtained showing a chronic atelectasis of RUL (Figure 3).
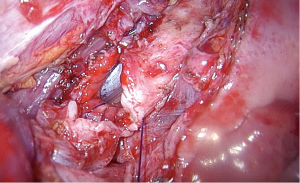
A right upper sleeve lobectomy was performed leaving the bronchial division for the end. The main and intermediate bronchus was cut by means of a bronchoplastic resection. An intra-operative frozen section was positive for malignancy from the proximal segment so a wider proximal resection margin towards the carina and distal trachea was performed until a disease-free histopathology report was confirmed.
The dissection of the right lower lung ligament was carried out to allow the mobilization of the remaining lobes and to avoid tension on the anastomosis.
The mediastinal lymphadenectomy was performed prior doing the anastomosis, to release trachea and bronchus and avoid tension on the suture. The posterior part of the trachea was initially reconstructed by using single PDS 3/0 sutures. The anastomosis of the bronchus intermedius and the edge of the carina was performed in two steps: first a continuous PDS 3/0 suture from back to front for the posterolateral wall of carina and another continuous suture for the anterolateral wall (lateral side of trachea and bronchus intermedius), tying both sutures at the anterior corner of the anastomosis (Figure 4).
After the hemostasis was checked, a single chest tube (20F) was inserted and the wound was closed. The patient was successfully extubated and transferred to the intensive care unit.
Evolution
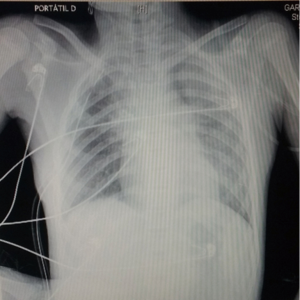
The patient was discharged from the intensive care unit to the ward 24 hours after the surgical procedure. She referred a 3/10 score on the visual analog pain scale without respiratory symptoms. A postoperative chest X-ray showed a normal expansion of the right middle and lower lobes.
The chest tube was removed on the fourth postoperative day and the patient was discharged home on the seventh postoperative day with excellent recovery (Figure 5). Before being discharged home, a bronchoscopy was performed confirming a perfect caliber of the anastomosis with no complications.
Discussion
The vast majority of bronchial sleeve resections are performed in patients diagnosed with tumor or polypoid bronchial disease, more frequently occurring in adult patients rather than in the pediatric population. In addition, reported cases refer to open surgical treatment instead of thoracoscopic surgery. To our knowledge and with a thorough review of PubMed, Science Direct, Cochrane and Ovid, there are no reports of uniportal VATS in pediatric patients.
Although technically more demanding, minimally invasive thoracoscopic surgery allows rapid recovery and generates less morbidity compared with open surgery (10). Technical advancements in surgical instruments designed for thoracoscopic surgery, allow surgeons to innovate and to make adaptations to techniques for the treatment of oncological diseases.
Uniportal VATS is an example of the continuing search for methods that aim to provide the patient a surgical cure of the disease with the lowest morbidity (11). In this particular case, the minimization of surgical invasiveness and preservation of the lung parenchyma is of great importance, as it offers better postoperative results and less rate of complications (12).
The application of uniportal VATS requires a highly trained surgical team in thoracoscopic surgery and when executed with dexterity, reduces morbidity and mortality. Despite current evidence being based on retrospective studies and case series, it is hereby shown that sleeve lobectomy by uniportal VATS is safe. It also offers great advantages such as reduction in postoperative complications and speeds up the period of patient recovery (12,13).
The sleeve bronchoplastic resection is usually the surgical method of choice in cases with proximal bronchial tumor obstruction. We must avoid thoracotomy and its associated morbidity and mortality, with particular emphasis on the pediatric population, so susceptible to alterations in their chest and lung development after surgical interventions.
In summary, we believe that the uniportal VATS technique for bronchoplastic procedures is an excellent option for the treatment of endobronchial tumors especially in the pediatric population
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Bagheri R. Tracheobronchopulmonary carcinoid tumors: analysis of 40 patients. Ann Thorac Cardiovasc Surg 2011;17:7-12. [Crossref] [PubMed]
- Gaissert HA, Mathisen DJ, Grillo HC, et al. Tracheobronchial sleeve resection in children and adolescents. J Pediatr Surg 1994;29:192-7; discussion 197-8. [Crossref] [PubMed]
- Erginel B, Ozkan B, Gun Soysal F, et al. Sleeve resection for bronchial carcinoid tumour in two children under six years old. World J Surg Oncol 2016;14:108. [Crossref] [PubMed]
- Tsuchiya R. Bronchoplastic techniques. In: Pearson FG, Cooper JD, Deslauriers J, et al. editors. Thoracic Surgery. New York: Churchill Livingstone, 2002:1005-13.
- Nesbitt J, Wind G. Right upper lobectomy and sleeve resection. In: Nesbitt J, Wind G. editors. Thoracic surgical oncology: Exposures and techniques. New York: Lippincott Williams and Wilkins, 2003:56-64.
- Ashiku S, DeCamp MM Jr. Parenchymal-Sparing Procedures in Lung Cancer: Sleeve Resection of the Lung for Proximal Lesions. Oper Tech Thor Card Surg 2006;11:295-309. [Crossref]
- D'Amico T. Right upper lobe sleeve resection. Oper Tech Thor Card Surg 1998;3:178-82. [Crossref]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-16. [PubMed]
- Gonzalez-Rivas D, Marin JC, Granados JP, et al. Uniportal VATS right upper sleeve tracheobronquial lobectomy. Asvide 2016;3:385. Available online: http://www.asvide.com/articles/1149
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Yang Y, Guerrero WG, Algitmi I, et al. Complex uniportal video-assisted thoracoscopic sleeve lobectomy during live surgery broadcasting. J Thorac Dis 2016;8:1345-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Lyscov A, Obukhova T, Ryabova V, et al. Double-sleeve and carinal resections using the uniportal VATS technique: a single centre experience. J Thorac Dis 2016;8:S235-41. [PubMed]