
Assessment of needle-based confocal laser endomicroscopy (nCLE) as a tool for real-time diagnosis of non-small cell lung cancer
Highlight box
Key findings
• The diagnostic value of needle-based confocal laser endomicroscopy (nCLE) is poorly understood, particularly in the case of suspicious pulmonary nodules.
What is known and what is new?
• The nCLE technology has been well documented in a study by Wijmans et al. Notably, this approach was based on its association with endoscopic ultrasound and focused mainly on lymph node involvement.
• This study is the first to describe the association between nCLE technology and electromagnetic navigational bronchoscopy for lung nodule assessment.
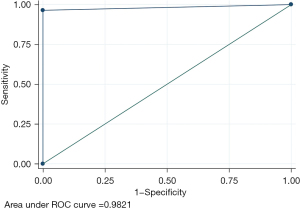
• A comparison of malignant and benign aspects with nCLE technology and pathology report revealed a sensitivity of 96.43% and a specificity of 100%. The area under the receiver operating characteristic curve was 0.98 (95% confidence interval: 0.83–0.99).
What is the implication, and what should change now?
• We believe that this technology may be utilized in the future for endobronchial analysis of suspected pulmonary lesions in the context of lung cancer screening programs, and for the injection of cytotoxic agents into the lesions.
Introduction
Lung cancer remains the leading cause of cancer-related deaths worldwide. However, a series of recent advances have led to a considerable improvement in overall survival. Considering the 3-year survival rate, the difference is significant, rising from 21% in 2004 to 31% in 2018 (1). This can be partly explained by the discovery of oncogenic drivers and, above and beyond that, the widespread use of targeted therapies targeting epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) (2-4). Approximately 10 years ago, the first cases of cancer immunotherapy represented a paradigm shift in the fight against cancer (5,6). Similarly, the combination of chemotherapy and immunotherapy will likely become the gold standard in the treatment of locally advanced lung cancer in the aftermath of the Checkmate816, Keynote671 or AEGEAN trials (7-9).
The other main change in cancer treatment is not related to therapeutic drugs but rather to public health development and the advent of organized lung cancer screening. Following the NLST trial in North America and the NELSON trial in Europe, many screening programs have been established worldwide (10,11). To date, there are no fewer than 9 lung cancer screening programs or trials currently underway in different populations, but only in France. The widespread deployment of these screening programs, which are based on low-dose chest computed tomography (CT) scans for specific populations, has increased the number of suspected pulmonary nodules diagnosed.
As a result, thoracic surgeons and pulmonologists are increasingly being called upon to carry out histological diagnosis using advanced fiberoptic techniques.
In the Department of Thoracic Surgery of Nancy Regional University Hospital, we routinely use electromagnetic navigational bronchoscopy (ENB) to obtain biopsies of pulmonary nodules or to identify nodules to be surgically resected by video-assisted thoracoscopic surgery (VATS) using indocyanine green (ICG) coupled to near-infrared fluorescence imaging. More recently, we have added confocal laser endomicroscopy (CLE) to ENB in order to help guide these procedures, particularly for small lesions. CLE is a laser-based technique in which fluorescein is intravenously injected to allow real-time visualization of cell shapes, mimicking a real-time microscope (12-14). Through recent advancements, imaging probes have become small enough to be advanced through a biopsy needle in a procedure known as needle-based CLE (nCLE) (15).
The technology in question has been well documented in a study by Wijmans et al. Notably, this approach was based on its association with endoscopic ultrasound (EUS) and focused mainly on lymph node involvement in the staging of 21 patients with or suspected of having NSCLC (16). At present, there is a lack of data on its use in treating pulmonary nodules.
The aim of our study was to retrospectively evaluate the concordance between CLE images and the pathological diagnosis of pulmonary nodules.
The results of our study indicate that nCLE technology has the potential to differentiate between benign and malignant lesions with a sensitivity of 96.43% and a specificity of 100%. The area under the receiver operating characteristic (ROC) curve was 0.98 [95% confidence interval (95% CI): 0.83–0.99]. However, it is important to note that distinguishing between these two categories of lesions can be challenging, and our study included only three benign lesions. These findings should be further validated in a prospective evaluation. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-546/rc).
Methods
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the French Society of Thoracic and Cardiovascular Surgery (approval No. CERC-SFCTCV-2023-10-03) and informed consent was obtained from all individual participants.
Procedure
ENB was performed as previously described (17,18). In summary, during an endobronchial navigational bronchoscopy (ENB) procedure, for dye injection or endoscopic biopsy, we used the Cellvizio system together with the AQ-Flex 19 probe (Mauna Kea Technologies, Paris, France) to optimize and guide the positioning of the probe at the time of biopsy or injection. The nCLE system was used together with ENB, without requiring radial endobronchial ultrasound (rEBUS) or 3D-imaging system [e.g., cone beam computed tomography (CT)].
As briefly described previously, all patients benefited from a preoperative injection of fluorescein ranging from 2.5 to 4.5 mL according to the quality of cell visualization (16).
Once navigation to the peripheral nodule was achieved, the ENB navigation probe was removed from the catheter, and the AQ-Flex 19 probe was advanced on an 18F Broncus Flex needle (Broncus Medical, San Jose, USA). At this juncture, the nodule is evaluated with the AQ-Flex 19 in order to ascertain the most pathological area. Once this area has been identified, the biopsy or ICG injection is performed.
Retrospectively, we extracted the videos captured by the probe and compared them with the final pathology report (obtained after surgical resection or via needle biopsy).
Patient selection
All patients included required an ENB for biopsy or lesion marking prior to VATS surgical resection and nCLE was used to optimize and guide the positioning of the probe. There was no restriction on nodule size, and nodules could be peripheral or centrally located. For technical reasons, we advanced the AQ-Flex 19 probe on the ENB catheter without using the 18F Broncus Flex needle for the last 10 patients in our cohort. For those last patients, we included only patients with bronchus signs to increase the likelihood of reaching the nodule.
Statistical analysis
We conducted a single-center retrospective analysis of adults who underwent ENB procedures at Nancy University Hospital, Nancy, France. The statistical analysis was performed using Stata software (Statacorp, Texas, USA).
Descriptive characteristics, including the mean ± standard deviation, median [interquartile range (IQR)], and 95% confidence intervals (CIs) of the means for continuous parameters and frequency distributions (number and proportion) for categorical parameters, were calculated for all patient demographics and baseline characteristics.
Study design
This was a retrospective, observational, single-center trial performed in the Thoracic Surgery Department of the Regional University Hospital of Nancy (France).
We collected data from patients who underwent major lung resection (i.e., lobectomy or segmentectomy) with lung nodule dye marking or lung nodule biopsy after ENB for suspected NSCLC or proven NSCLC cT1a-T3N0 between June and October 2023. All the data were extracted though the medical charts.
Preoperative staging included chest and abdominal CT scans as well as a position emission tomography (PET) scan. Brain imaging was performed via magnetic resonance imaging (MRI) or CT depending on the availability of the exam. Pulmonary function tests (PFTs) were routinely performed for patients scheduled for lung resection.
Patients underwent either open thoracotomy or VATS according to the surgeon’s preference. Radical lymph node dissection was routinely performed as recommended (19).
Study endpoints
The primary endpoint of this study was the concordance between the observation of nCLE pulmonary nodules suggesting malignant or benign pathology and the pathological diagnosis.
The secondary endpoints were the feasibility of nCLE guidance during an endobronchial navigation procedure (number of patients with high-quality images/number of patients included) and the occurrence of major complications/minors during the procedure.
Results
Cohort characteristics
Overall, 30 patients were retrospectively included in the study. The median size of the suspicious lesions was 16 mm (IQR, 13 mm). The characteristics of the patients included are summarized in Table 1.
Table 1
| Variable | Values (n=30) |
|---|---|
| Age (years) | 63.5 [14] |
| Gender | |
| Male | 15 (50.0) |
| Female | 15 (50.0) |
| Body mass index (kg/m2) | 28 [9] |
| Lung nodule size (mm) | 16 [13] |
| Preoperative (n=24) | |
| FEV1 (%) | 88 [22] |
| DLCO (%) | 89 [28] |
| nCLE aspects | |
| Dark enlarged pleomorphic cells | 22 (73.3) |
| Dark clusters | 5 (16.7) |
| Mix (clusters/pleomorphic cells) | 1 (3.3) |
| Granuloma | 2 (6.7) |
| Type of surgery (n=24) | |
| Lobectomy | 11 (45.8) |
| Segmentectomy | 8 (26.7) |
| Wedge | 5 (16.7) |
| Histology | |
| ADK | 19 (63.3) |
| SCC | 5 (16.7) |
| Carcinoid | 1 (3.3) |
| NOS | 1 (3.3) |
| SCLC | 1 (3.3) |
| Benign | 3 (10.0) |
| Complications | |
| Minor | 1 (3.3) |
| Major | 0 (0.0) |
| Bronchus sign (n=20) | 10 (50.0) |
Data are presented as n (%) or median [IQR]. FEV1, forced expiratory volume in one second; DLCO, diffusing capacity for carbon monoxide; nCLE, needle-based confocal laser endomicroscopy; ADK, adenocarcinoma; SCC, squamous cell carcinoma; NOS, not otherwise specified; SCLC, small-cell lung cancer; IQR, interquartile range.
In 22/30 patients, dark enlarged pleomorphic cells were visualized, and for one patient, a mix of dark clusters and dark enlarged pleomorphic cells was visualized, leading to a diagnosis of cancer in 22/23 (95.6%). In 5 other patients, dark clusters were visualized, resulting in a diagnosis of cancer in 100% of patients. For 2 patients, we found granuloma leading to a diagnosis of benign disease (100%). The association between the aspect of nCLE images and the final pathology was statistically significant (P=0.004) (Table 2).
Table 2
| nCLE images | Malignant | Benign |
|---|---|---|
| Dark pleomorphic cells | 21 | 1 |
| Dark clusters | 5 | 0 |
| Mix | 1 | 0 |
| Granuloma | 0 | 2 |
nCLE, needle-based confocal laser endomicroscopy.
A comparison of malignant and benign aspects with nCLE technology and pathology report revealed a sensitivity of 96.43% and a specificity of 100%. The area under the curve of the ROC curve was 0.98 (95% CI: 0.83–0.99) (Figure 1).
Pathology report
Pathology was performed for 6/30 patients (20%) by endobronchial biopsy and for 24 patients by surgical resection of the suspicious lesion (80%) (including wedge/segmentectomy or lobectomy).
Table 3 shows the different pathological images encountered: dark clusters, dark enlarged pleomorphic cells or normal alveolar tissue.
Table 3
| nCLE images | Adenocarcinoma | Not otherwise specified | Carcinoid | Squamous cell carcinoma | Small-cell lung cancer | Benign disease |
|---|---|---|---|---|---|---|
| Dark pleomorphic cells |  |
 |
 |
 |
 |
– |
| Dark clusters |  |
– | – | – | – | – |
| Granuloma | – | – | – | – | – |  |
nCLE, needle-based confocal laser endomicroscopy.
There were 27 malignant lesions in the 30 patients included (90%): 18 adenocarcinomas (ADK), 6 squamous cell carcinomas (SCCs), 1 carcinoid tumor, 1 not otherwise specified (NOS) tumor, 1 small-cell lung cancer (SCLC) and 3 benign lesions (diagnosis was proven with endobronchial biopsy for one patient who would benefit from a short-term follow-up; the other 2 patients had a wedge resection with frozen section confirming benign disease).
Among the four biopsies positive for non-small cell lung cancer (NSCLC), programmed death-ligand 1 (PD-L1) expression was assessed in all patients, ALK and ROS-1 were detected by IHC in two patients, and a molecular analysis was performed for EGFR in one patient.
Navigation
The median time the nCLE system was in contact with the lesion was 5 minutes (IQR, 5 minutes). The median navigation time to the nodule was 8.5 minutes (IQR, 5 minutes). Navigation to the lung nodule was possible in all patients, and quality images were obtained and recorded during every procedure (100%). Except for the last ten patients (selected on the basis of nodule accessibility according to the preoperative CT scan), a bronchus sign was present in 10/20 patients (50%).
Regarding complications, only one minor complication was reported in the cohort (3.3%). This was minor bleeding from the bronchus of the biopsied lesion, which was easily controlled by endobronchial injection of ice-cold serum. No major complications were described.
Discussion
The diagnostic value of nCLE is poorly understood, particularly in the case of suspicious pulmonary nodules.
This situation is particularly common in daily clinical practice, and we have been able to demonstrate that the detection of dark clusters or dark enlarged pleomorphic cells allows us to confirm the tumor nature of the lesion in more than 95% of patients in a relatively short examination time (median time 5 minutes). Furthermore, the median navigation time to the target in an expert center was similarly short (8 minutes). This minimally invasive procedure is performed through natural orifices, resulting in very low morbidity (1 case of minor bleeding controlled endoscopically).
The trans-thoracic needle aspiration (TTNA) technique is frequently compared to ENB, with or without nCLE technology. However, we believe this to be a methodological error, as the targets accessible are theoretically not the same. Although it does not target the same types of lesion due to the location, endobronchial navigation offers the advantage of avoiding irradiation, and being less morbid, particularly in emphysematous patients (commonly accepted rate of pneumothorax of 1.5% for endobronchial navigation compared with 15% for TTNA) (20,21). In addition, in the era of immunotherapy and personalized treatments, this technique has made it possible to assess PD-L1 expression on biopsy in all NSCLC patients, to search for ALK or ROS-1 expression by immunohistochemistry (IHC) in half of the patients and to carry out molecular biology tests in 25% of the patients.
Moreover, in an era when lung cancer screening programs are being developed worldwide, this type of approach seems more than necessary to enable early diagnosis.
On the other hand, this technique also has its own limitations, such as the need for performance under general anesthesia, access to the operating theatre when this procedure is performed there, and the cost of the equipment. Additionally, as in France, it is not currently reimbursed by many healthcare systems.
This study is the first to describe the association between nCLE technology and electromagnetic navigational bronchoscopy. These results are interesting given that, in all cases, ENB enabled the nCLE probe to contact the nodule quickly. Concurrently, a prior study suggested the use of conjunction of nCLE technology with robot-assisted bronchoscopy (Monarch) and radial EBUS to evaluate the value of nCLE for repositioning at the time of biopsy (22). This study demonstrated that in 45% of patients, the use of nCLE indicated the need for probe repositioning. The average examination time in this study was 52 minutes. In contrast, one of the very first investigations of the ENB procedure in 2007 estimated the average duration of the ENB procedure with biopsy to be 26 minutes (23).
In addition, this study comprises the largest cohort of pulmonary nodules to date (n=30), and the images obtained are consistent with the final histological data reported for more than 95% of the patients, without any major complications.
Furthermore, compared to previous study published by the Wijmans team, our study provides external validation of these previous results at a new center (16). This study is also the first based on a strategy of injection (ICG) or biopsy with nCLE guidance followed by surgical resection; more than 80% of the patients in the series underwent surgery at the same time.
Another interesting feature we experienced is the possibility of performing biopsies or injections without the use of fluoroscopy. For technical reasons, we perform most of our biopsies without real-time radiological control; in these cases, the use of nCLE to guide the biopsy procedure seems to be an additional safety factor limiting irradiation to patients and the whole medical team.
The nCLE technology may also be considered a potential alternative to the rapid onsite evaluation (ROSE) system, which enables a pathologist to provide a rapid diagnosis in the immediate aftermath of a biopsy. When considering the financial implications of the ROSE system and the availability of a dedicated pathologist in the operating room, it is challenging to directly assess the comparative value of ROSE and nCLE technology. Nevertheless, for the present time, nCLE remains a technique for assisting and guiding needle placement during biopsy. Furthermore, should future results reinforce the diagnostic efficacy of nCLE, the ROSE system may no longer be necessary in centers with nCLE technology.
The limitations of our study include its single-center and retrospective nature. Furthermore, these results need to be validated in larger studies due to the size of our cohort. The other current limitation of the technique lies in the boundaries that are sometimes blurred between the different patterns, i.e., the difference between benign lesions (granuloma) and some malignant lesions, particularly in the case of dark, enlarged pleomorphic cells. Future studies may also have to investigate the influence of the learning curve on image analysis and the performance of the procedure.
These very interesting results also allow us to foresee the future use of this type of technology for rapid diagnosis. In one of the patients in our cohort who required frozen sectioning, we examined the structure of the nodule on the back table using nCLE after the wedge had been made. These results were consistent with the findings of malignancy (dark enlarged pleomorphic cells) as were those from the frozen section examination. If this type of approach can be validated, the patient could be quickly dispatched to the operating room. Finally, although not evaluated in this study, the possibility of performing mediastinal lymph node staging in real time, as previously described by Wijmans et al. (16), is another major advantage of this system.
Conclusions
The direct, real-time visualization of lung tissue in front of the needle appears to be a significant advantage when performing ENB biopsies, particularly when it highlights images suspicious of malignancy (dark pleomorphic cells and dark clusters).
We believe that this technology may be utilized in the future for endobronchial analysis of suspected pulmonary lesions in the context of lung cancer screening programs, and for the injection of cytotoxic agents into the lesions. However, the diagnostic value of this system needs to be confirmed, particularly for benign lesions.
Acknowledgments
We would like to thank MaunaKea Technologies for supplying the AQ19 Flex probes and Broncus needles used in this study. This work was supported by MaunaKea Technologies. Our funding source (MaunaKea Technologies) was not involved in the study design, analysis or in decision to submit the article for publication.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-546/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-546/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-546/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-546/coif). All authors report that Mauna Kea Technologies provided the probes and needles used in the study. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the French Society of Thoracic and Cardiovascular Surgery (approval No. CERC-SFCTCV-2023-10-03) and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [Crossref] [PubMed]
- Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 2005;353:123-32. [Crossref] [PubMed]
- Wu YL, Tsuboi M, He J, et al. Osimertinib in Resected EGFR-Mutated Non-Small-Cell Lung Cancer. N Engl J Med 2020;383:1711-23. [Crossref] [PubMed]
- Shaw AT, Yeap BY, Solomon BJ, et al. Effect of crizotinib on overall survival in patients with advanced non-small-cell lung cancer harbouring ALK gene rearrangement: a retrospective analysis. Lancet Oncol 2011;12:1004-12. [Crossref] [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. [Crossref] [PubMed]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Wakelee H, Liberman M, Kato T, et al. Perioperative Pembrolizumab for Early-Stage Non-Small-Cell Lung Cancer. N Engl J Med 2023;389:491-503. [Crossref] [PubMed]
- Heymach JV, Harpole D, Mitsudomi T, et al. Abstract CT005: AEGEAN: a phase 3 trial of neoadjuvant durvalumab + chemotherapy followed by adjuvant durvalumab in patients with resectable NSCLC. Cancer Res 2023;83:CT005. [Crossref]
- Forde PM, Spicer J, Lu S, et al. Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer. N Engl J Med 2022;386:1973-85. [Crossref] [PubMed]
- de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med 2020;382:503-13. [Crossref] [PubMed]
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Giovannini M. Needle-based confocal laser endomicroscopy. Endosc Ultrasound 2015;4:284-8. [Crossref] [PubMed]
- Krishna SG, Brugge WR, Dewitt JM, et al. Needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cystic lesions: an international external interobserver and intraobserver study (with videos). Gastrointest Endosc 2017;86:644-654.e2. [Crossref] [PubMed]
- Benias PC, D'Souza LS, Papafragkakis H, et al. Needle-based confocal endomicroscopy for evaluation of malignant lymph nodes - a feasibility study. Endoscopy 2016;48:923-8. [Crossref] [PubMed]
- Wijmans L, de Bruin DM, Meijer SL, et al. Real-Time Optical Biopsy of Lung Cancer. Am J Respir Crit Care Med 2016;194:e10-1. [Crossref] [PubMed]
- Wijmans L, Yared J, de Bruin DM, et al. Needle-based confocal laser endomicroscopy for real-time diagnosing and staging of lung cancer. Eur Respir J 2019;53:1801520. [Crossref] [PubMed]
- Stasiak F, Seitlinger J, Streit A, et al. Sentinel Lymph Node in Non-Small Cell Lung Cancer: Assessment of Feasibility and Safety by Near-Infrared Fluorescence Imaging and Clinical Consequences. J Pers Med 2022;13:90. [Crossref] [PubMed]
- Seitlinger J, Stasiak F, Piccoli J, et al. What is the appropriate "first lymph node" in the era of segmentectomy for non-small cell lung cancer? Front Oncol 2022;12:1078606. [Crossref] [PubMed]
- Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg 2006;30:787-92. [Crossref] [PubMed]
- Wang Memoli JS, Nietert PJ, Silvestri GA. Meta-analysis of guided bronchoscopy for the evaluation of the pulmonary nodule. Chest 2012;142:385-93. [Crossref] [PubMed]
- Wiener RS, Schwartz LM, Woloshin S, et al. Population-based risk for complications after transthoracic needle lung biopsy of a pulmonary nodule: an analysis of discharge records. Ann Intern Med 2011;155:137-44. [Crossref] [PubMed]
- Manley CJ, Kramer T, Kumar R, et al. Robotic bronchoscopic needle-based confocal laser endomicroscopy to diagnose peripheral lung nodules. Respirology 2023;28:475-83. [Crossref] [PubMed]
- Eberhardt R, Anantham D, Herth F, et al. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest 2007;131:1800-5. [Crossref] [PubMed]


