Stenting or bypass surgery for unprotected left main coronary artery disease—still a long rally to go
Coronary artery disease (CAD) is still major cause of mortality and morbidity in western country (1,2). With the advancement of percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG) is not the only choice of revascularization for CAD (1,2). The left main coronary artery (LMCA) arises from aortic sinus and supplies the around 70% myocardium in patients with right dominant type and 100% in patients with left dominant type (3). Therefore, severe LMCA stenosis will reduce coronary perfusion to large portion of the myocardium and may cause terrible consequences. The definition of LMCA stenosis is the reduction by more than 50% in the luminal diameter of LMCA (4). Patients with LMCA stenosis are associated with higher mortality, and LMCA stenosis is a strong independent predictor of mortality and morbidity in patients with CAD (1,2,5-7). The average diameter of LMCA is usually more than 3 mm (8), implying LMCA is theoretically considered suitable for coronary stenting. However, the complex anatomy of LMCA may associate with periprocedural complications and restenosis of PCI (9,10). Furthermore, most LMCA lesions are at distal site presenting as bifurcation or trifurcation lesions, which is challenging for PCI. Given that patients with isolated LMCA stenosis are rare, and most patients with LMCA stenosis are associated with severe double or triple vessel disease, complete revascularization by CABG is still the golden standard for treating unprotected LMCA stenosis (1,2) although intravascular ultrasound-guided PCI is considered a reasonable alternative nowadays (11).
With improvement of the design in PCI devices such as drug eluting stent (DES) and pharmacological treatment, more and more evidences shows that PCI is a safe and effective revascularization strategy for patients with unprotected LMCA stenosis and multivessel CAD in short term period. Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) study is the first large-scale randomized trial comparing the long-term outcomes after LMCA stenting with first generation DES to CABG in patients with unprotected LMCA stenosis (12). There was no significant different between PCI and CABG in mortality and major advanced cardiac and cerebral events (MACCE) in patients with unprotected LMCA stenosis in low/intermediate SYNTAX score (<33) although target lesion revascularization (TLR) rate is higher in PCI group than CABG group. However, CABG provided better long-term outcome including survival rate in patients with high SYNTAX score (≥33). Interestingly, among patient cohort of multi-vessel CAD but no critical LMCA stenosis, CABG was superior to PCI in cardiac death, TLR, and MACCE. This finding suggests that stenting at LMCA may secure the upstream coronary artery flow and provide adequate perfusion to the large territory of left coronary artery system. Importantly, the results of Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease (PRECOMBAT) (13) and Xience Everolimus-Eluting Stent Versus Coronary Artery Bypass Surgery for Effectiveness of Left-Main Revascularization (EXCEL) (14) are consistent with the results of LMCA stenosis cohort in SYNTAX study. Table 1 lists the randomized clinical trials comparing PCI and CABG in patients with unprotected LMCA stenosis.
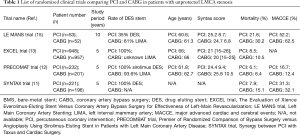
Full table
The LE MANS (Left Main Coronary Artery Stenting) trial was the first prospective randomized study to compare left main stenting (n=52) to CABG (n=53) in patients with unprotected LMCA stenosis. There was no significant different of short-term survival rate between PCI and CABG group in patients with LMCA stenosis in low to intermediate SYNTAX score (<33). However, the repeat revascularization rate was higher in PCI group than CABG group during the 28±9.9 months of follow-up (relative risk: 1.27; 95% confidence interval: 1.05–1.54; P<0.01). Notably, PCI provided better improvement of left ventricular ejection fraction (LVEF) than CABG group (P=0.04) (15). Recently, Dr. Buszman and his colleagues published the 10-year outcomes of LE MANS study in Journal of the American College of Cardiology Cardiovascular Interventions (16). The major findings are that PCI with stenting demonstrated equivalent outcomes in the very long-term as compared to CABG in patients with unprotected LMCA obstruction and low to intermediate SYNTAX score (<33). In addition, there was no significant between PCI and CABG groups in myocardial infarction (8.7% vs. 10.4%; P=0.62), stroke (4.3% vs. 6.3%; P=0.68) and repeat revascularization (26.1% vs. 31.3%; P=0.64). LE MANS study is the first randomized study to prove that PCI also provide similar very long-term outcomes in patients with unprotected LMCA stenosis and low to intermediate SYNTAX score (<33). Although their findings are interesting with clinical meaning, and provide us a new evidence and concept to manage the patients with unprotected LMCA stenosis, there are some issues that should be discussed.
Instead of DES, 65% of patients in PCI group in LE MANS study received bare metal stent (BMS) during PCI, which is not recommended by established guidelines. This finding is different to previous studies (17-19). Surprisingly, mortality (21.6% vs. 30.2%), repeat revascularization (26.1% vs. 31.3%), and MACCE (51.1% vs. 64.4%) were similar between two groups. These findings were different from previous studies, which found CABG group is with less TVR revascularization rate (12-14). On the other hand, there was only 72% of patients received left internal mammary artery (LIMA) graft to left anterior descending artery in CABG group in this study, which is apparently lower than those in other studies (>95%) (12,13). The LIMA graft provides long-term patent rate than saphenous vein graft in patients undergoing CABG and leads to better clinical outcomes (20). This difference may explain why CABG group in LE MANS study did not could not reduce repeat vascularization rate in LE MANS study. Furthermore, LVEF is one of secondary endpoint in the LE MANS study, and PCI group provided better LVEF preserved function than CABG group in the first year and maintain the LVEF function after 10 years. Nevertheless, 35% patients did not echocardiography in this study which initially enrolled only 105 patients. It may be not adequately powered to exam this primary endpoint. Finally, the penetration and adherence rate with anti-platelet therapy, beta-blocker, angiotensin inhibition, and statin therapy was high in both groups in the LE MANS trial. Optimal risk factor modification is crucial to reduce mortality and morbidity in patients with stable CAD (21), suggesting optimization of medical therapy together with selection of appropriate revascularization therapy is mandatory to order to achieve better long-term clinical outcomes in this specific patient group.
Similar to SYNTAX study, the LE MANS trial showed that PCI with optimal medical therapy is not inferior to CABG among patients with unprotected LMCA stenosis and low to intermediate SYNTAX score (<33) in 10 years after index procedure. Given that graft failure rate may as high as 50% at 10 years after CABG (22), PCI is promising to catch up with CABG in this long rally! However, answers for several questions remains unclear: (I) the comparison between PCI with 2nd generation DES and CABG in long-term outcomes; (II) PCI vs. CABG in non-bifurcation LMCA stenosis; (III) whether chronic total occlusion may have an impact in procedural success and clinical outcomes this patient population? (IV) why PCI has different outcomes in the patient cohorts with and without LMCA stenosis in SYNTAX study? (V) optimal duration of dual anti-platelet therapy in the era of 2nd generation DES and bioabsorbable vascular scaffold. Further large scale, long-term clinical trials or registries are warranted to investigate these important issues.
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Yue Liu (Associate professor, Department of Cardiology, The First Affiliated Hospital of Harbin Medical University, Harbin, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011;124:2610-42. [Crossref] [PubMed]
- Authors/Task Force members, Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541-619. [Crossref] [PubMed]
- Kalbfleisch H, Hort W. Quantitative study on the size of coronary artery supplying areas postmortem. Am Heart J 1977;94:183-8. [Crossref] [PubMed]
- Taylor HA, Deumite NJ, Chaitman BR, et al. Asymptomatic left main coronary artery disease in the Coronary Artery Surgery Study (CASS) registry. Circulation 1989;79:1171-9. [Crossref] [PubMed]
- Athappan G, Patvardhan E, Tuzcu ME, et al. Left main coronary artery stenosis: a meta-analysis of drug-eluting stents versus coronary artery bypass grafting. JACC Cardiovasc Interv 2013;6:1219-30. [Crossref] [PubMed]
- Brennan JM, Dai D, Patel MR, et al. Characteristics and long-term outcomes of percutaneous revascularization of unprotected left main coronary artery stenosis in the United States: a report from the National Cardiovascular Data Registry, 2004 to 2008. J Am Coll Cardiol 2012;59:648-54. [Crossref] [PubMed]
- Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation 1999;100:1464-80. [Crossref] [PubMed]
- von Birgelen C, Airiian SG, Mintz GS, et al. Variations of remodeling in response to left main atherosclerosis assessed with intravascular ultrasound in vivo. Am J Cardiol 1997;80:1408-13. [Crossref] [PubMed]
- Ragosta M, Dee S, Sarembock IJ, et al. Prevalence of unfavorable angiographic characteristics for percutaneous intervention in patients with unprotected left main coronary artery disease. Catheter Cardiovasc Interv 2006;68:357-62. [Crossref] [PubMed]
- Capodanno D, Capranzano P, Di Salvo ME, et al. Usefulness of SYNTAX score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. JACC Cardiovasc Interv 2009;2:731-8. [Crossref] [PubMed]
- de la Torre Hernandez JM, Baz Alonso JA. Clinical impact of intravascular ultrasound guidance in drug-eluting stent implantation for unprotected left main coronary disease: pooled analysis at the patient-level of 4 registries. JACC Cardiovasc Interv 2014;7:244-54. [Crossref] [PubMed]
- Morice MC, Serruys PW, Kappetein AP, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation 2014;129:2388-94. [Crossref] [PubMed]
- Ahn JM, Roh JH, Kim YH, et al. Randomized Trial of Stents Versus Bypass Surgery for Left Main Coronary Artery Disease: 5-Year Outcomes of the PRECOMBAT Study. J Am Coll Cardiol 2015;65:2198-206. [Crossref] [PubMed]
- Campos CM, van Klaveren D, Farooq V, et al. Long-term forecasting and comparison of mortality in the Evaluation of the Xience Everolimus Eluting Stent vs. Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL) trial: prospective validation of the SYNTAX Score II. Eur Heart J 2015;36:1231-41. [Crossref] [PubMed]
- Buszman PE, Buszman PP, Kiesz RS, et al. Early and long-term results of unprotected left main coronary artery stenting: the LE MANS (Left Main Coronary Artery Stenting) registry. J Am Coll Cardiol 2009;54:1500-11. [Crossref] [PubMed]
- Buszman PE, Buszman PP, Banasiewicz-Szkróbka I, et al. Left Main Stenting in Comparison With Surgical Revascularization: 10-Year Outcomes of the (Left Main Coronary Artery Stenting) LE MANS Trial. JACC Cardiovasc Interv 2016;9:318-27. [Crossref] [PubMed]
- Seung KB, Park DW, Kim YH, et al. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N Engl J Med 2008;358:1781-92. [Crossref] [PubMed]
- Park DW, Kim YH, Yun SC, et al. Long-term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 10-year results of bare-metal stents and 5-year results of drug-eluting stents from the ASAN-MAIN (ASAN Medical Center-Left MAIN Revascularization) Registry. J Am Coll Cardiol 2010;56:1366-75. [Crossref] [PubMed]
- Cheng CI, Lee FY, Chang JP, et al. Long-term outcomes of intervention for unprotected left main coronary artery stenosis: coronary stenting vs coronary artery bypass grafting. Circ J 2009;73:705-12. [Crossref] [PubMed]
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1-6. [Crossref] [PubMed]
- Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16. [Crossref] [PubMed]
- Fitzgibbon GM, Kafka HP, Leach AJ, et al. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol 1996;28:616-26. [Crossref] [PubMed]


