Current advances of endobronchial ultrasonography in the diagnosis and staging of lung cancer
Introduction
Lung cancer is the leading cause of cancer related death (1). The prognosis for lung cancer is extremely poor and a five year survival rate remains less than 15% (2). Two-thirds of patients had advanced disease when they were diagnosed (1,3). The factors that affect prognosis in patients with lung cancer are stage, histology, performance status, comorbidity, age and sex (4). Before the introduction of novel cytotoxic chemotherapy (pemetrexed) and biologic agents (bevacizumab), the main diagnostic modalities and focus on tissue acquisition were obtaining small samples for simple histopathological characterization: small cell lung cancer (SCLC) vs. non-small cell lung cancer (NSCLC) (5,6). Markers to differentiate between adenocarcinoma and squamous cell carcinoma are now necessary and are defined by the 2011 International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) lung adenocarcinoma classification (7). Adenocarcinoma can also be classified according to the driver oncogene mutation that is present, which is usually mutually exclusive in the different subtypes (8). The current guidelines suggest molecular testing for EGFR and ALK after adenocarcinoma has been confirmed. Therefore, sufficient and high quality tissue for diagnosis, and molecular testing for treatment selection become important.
In the treatment of lung cancer, staging is a prognostic factor not only for determining whether there is surgically resectable disease but also for the treatment planning (9). How to improve techniques for tissue acquisition in diagnosis and staging becomes important for improving the prognosis.
Endobroncial ultrasound radial probe (EBUS RP)
EBUS has become an important tool in daily practice for diagnosis and staging of lung cancer in the last decade (10). There are two types of probes used in EBUS: the RP and the convex probe (CP), which have technical differences and distinct diagnostic abilities. EBUS RB as a guidance technique for peripheral pulmonary lesions (PPL) and for the evaluation of tumor involvement of the tracheobronchial wall is now used for the diagnosis of PPL (11). Before the EBUS RB as one of the tissue biopsy tools for PPL, transthoracic needle aspiration (TTNA), flexible bronchoscopy with traditional transbronchial biopsy (TBB) or even direct surgical excision were recommended (12). TTNA is currently preferred because it has a diagnostic yield of 90% but high pneumothorax rate (25%), of which at least 5% requires chest tube insertion (12,13). The sensitivity of flexible bronchoscopy biopsy ranges from 14% to 63%, depending on size and location (13,14). EBUS RP offers guidance during bronchoscopy to help reach the lesion. The diagnostic yield varied from 46% to 86.2% and pooled sensitivity was 73% for all lesions and even better in the diagnosis of lung cancer (15,16). There is no direct comparison between EBUS RB and fluoroscopy in lung cancer diagnosis (17), but combined these two modality increased the diagnostic yield (18). Guide sheath (GS) is designed to increase the reliability of collection from PPL. EBUS-GS can decrease the total procedure time and decreased the bleeding rate (19). However, a meta-analysis showed sensitivity increased 2% when compared with EBUS RP without GS (16). Efforts to increase the diagnostic accuracy of EBUS RP are still ongoing. The position of the probe (within or adjacent to the PPL) independently predicts the diagnostic yield, and all efforts to reach the small bronchus within the lesions should be done (19). Beyond the conventional diagnostic procedures (CDPs) including TBB, bronchial washing and brushing, there are several approaches to improve performance. EBUS RP with CDPs and combined with transbronchial needle aspiration (TBNA) can increase the diagnostic yield without additional risk (20). The diagnostic benefit of EBUS-GS for PPLs was minimal when the probe was adjacent to the lesion (19). TBNA (passing a needle through the bronchial wall) can be the better solution if the EBUS probe was adjacent to the lesions (20,21). Suction catheter–biopsy is one technique for obtaining tissue sample from PPLs. This approach is efficient, safe and is complementary to TTB (22). Another approach to increase the diagnostic yield is EBUS RP guided cryobiopsy, with which the diagnosis can be 61% by forceps and 74% by cryoprobe (23,24). The guidelines of the american college of chest physicians suggest the use of EBUS is recommended in patients with PPLs when tissue diagnosis is required due to uncertainty of diagnosis or poor surgical candidacy (25).
In the last decade, new techniques other than EBUS RP have emerged and helped to guide and biopsy PPLs through the tracheobronchial tree during bronchoscopy. Electromagnetic navigation bronchoscopy (ENB) and virtual bronchoscopy (VB) can create a virtual image for biopsy. ENB provides real-time directions for approach. The diagnostic yield is similar when ENB or VB is used for biopsy compared with EBUS RP guidance biopsy (16). But when combining two methods such as EBUS RP + ENB, or EBUS RP + VB, the diagnostic yield increases significantly (16,18,26-28). Ultrathin bronchoscopy is another tool to increase diagnostic accuracy. It has a diameter of 3.0 mm, incorporating a working channel with a different inner diameter, and can reach fourth-generation bronchi (29). The novel ultrathin bronchoscopy has a 1.7 mm working channel, which allows the use of a RP EBUS and 1.5 mm biopsy forceps (29). Combining ultrathin bronchoscopy with EBUS RP sans GS improved the diagnostic yield compared with thin bronchoscopy with EBUS GS (29).
Imaging from EBUS RP correlates well with the histopathologic findings of benign and malignant lesions (30,31), but final diagnosis needs to be made via tissue biopsy. During EBUS RP guidance PPL biopsy, rapid on site evaluation (ROSE) improved diagnosed yield (32). If ROSE is not available, at least 4–5 biopsies per lesion are necessary to get adequate sensitivity of diagnosis (33,34). The most frequent complications of EBUS RP guidance biopsy are bleeding and pneumothorax. But these complications are self-limited and seldom required intervention (15,35).
EBUS CP
Accurate staging is one of the important factors affecting patient management. Before the development of direct real-time EBUS-guided TBNA using a CP (36), mediastinoscopy remained the “gold standard” for mediastinal staging in lung cancer (37). Mediastinoscopy is invasive, requires general anesthesia and cannot be performed repeatedly. Therefore, several minimally invasive methods have been used for tissue sampling including conventional bronchoscopy with TBNA guided by fluoroscopy or EBUS RP, but the yield varied widely (38-40). After one large randomized control trial compared surgical staging or combined EBUS-TBNA and transesophageal ultrasound fine needle aspiration (EUS-FNA) followed by surgical staging (41), EBUS CP guided TBNA (EBUS-TBNA) is now the first choice for mediastinal LN staging (9,42). Another single arm study also supports that EBUS TBNA is better than mediastinoscopy (43). EBUS TBNA is not only a minimally invasive procedure that can be performed repeatedly, but also has higher sensitivity and specificity in specific lymph node stations (9,44). Mediastinoscopy had lower diagnostic yield in lymph node station 7, which was easily approached by EBUS-TBNA with very high sensitivity (45).
In the previous guideline, lymph node staging by tissue sampling is usually suggested in lymph nodes with short-axis diameter >1 cm on CT scan (46) or PET positive lymph nodes (47). But more than 10% of patients who had no lymph node metastasis by image criteria had lymph node metastasis confirmed by thoracotomy (48-50). Because EBUS TBNA can be performed in an outpatient setting, current guidelines suggest that with patients with clinical N1 disease (51), central tumor and tumor >3 cm, and mainly adenocarcinoma with high fluorodeoxyglucose (FDG)uptake (52,53) all lymph nodes >0.5 cm found in echosonography (9,42) should be sampled, precisely because all of these conditions are associated with a high probability of mediastinal lymph node metastases.
Efforts to improve the diagnostic yield are still ongoing, including large size needle (22 vs. 21 gauge needle) (54) and transbronchial needle forceps (55). None of the new techniques improved the diagnostic yield because EBUS TBNA with 22 gauge needle and ROSE had nearly 90% sensitivity and 100% specificity (9,44). However, the accuracy of EBUS-TBNA is quite dependent on experience (56). High-volume hospitals were associated with high diagnostic yields (56,57). How to acquire mastery during training is important in interventional bronchology (57).
There are several sonographic characteristics of malignant lymph nodes found by EBUS CP. These factors include large size, round shape, distinct margin, absent central hilum sign and distinct vascular pattern (58,59). A hard lymph node demonstrated by elastography of new CP is also a predictor of malignancy (60). But none of these factors had high sensitivity or specificity compared with direct sampling.
It is now suggested to assay all lymph nodes with size more than 0.5 cm, and at least 3–4 lymph node stations if possible (42). At least one tissue core is needed per lymph node to get adequate diagnosis. If tissue core is not available, three aspirations are advised (61). ROSE should always be considered because it can decrease the frequency of aspiration and total time of procedure. Higher N stage LNs should always be sampled first: N3 > N2 > N1, because the final stage only includes high N stages. Another reason is that if we use one needle for one patient, sampling lower N stage LNs before the high N stage may upgrade N stage through contamination. If possible, lymph node stations 4R, 4L and 7 should be evaluated in all patients who receive EBUS CP study (42). Because EBUS TBNA is the first choice for LN staging with high sensitivity and specificity, several studies suggest EBUS TBNA for lung cancer diagnosis and staging at the same time because it reduces the time to treatment decision compared with conventional diagnosis and staging techniques (62,63). The Complication rate for EBUS TBNA is low. In a national survey of complications associated with EBUS-TBNA by the Japan Society for Respiratory Endoscopy, the most frequent complications were hemorrhage and infection with only one mortality due to ischemic stroke after withdrawal of antiplatelet drugs (replaced by heparin) (64).
Conclusions
EBUS is a powerful tool for lung cancer diagnosis and staging (Table 1). EBUS CP guided TBNA (EBUS TBNA) is now the first choice for staging mediastinal LNs. Because of the high sensitivity (>90%) and specificity (almost 100%), little improvement could be made by new techniques. However, the sensitivity is mainly dependent on the operator. How to improve the diagnostic yield through training is still an issue. EBUS RP guided TBB has lower sensitivity compared with TTNA in tissue sampling. But the complication rate of EBUS TBB is significantly lower than that of TTNA. There are many new techniques that can be combined with EBUS TBB to increase the diagnostic yield. EBUS also helps these techniques in sampling of PPL and vice versa. It is suggested that for peripheral lesions, we could perform bronchoscopy for airway evaluation and EBUS TBB for tissue sampling at the same time before moving to more the invasive TTNA for diagnosis.
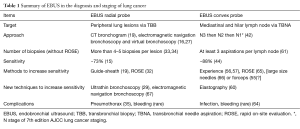
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: CC Ho has received grants from AstraZeneca (#ISSIRES0105). The other authors have no conflicts of interest to declare.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Spira A, Ettinger DS. Multidisciplinary management of lung cancer. N Engl J Med 2004;350:379-92.
- Wang BY, Huang JY, Cheng CY, et al. Lung cancer and prognosis in taiwan: a population-based cancer registry. J Thorac Oncol 2013;8:1128-35. [Crossref] [PubMed]
- Salomaa ER, Sällinen S, Hiekkanen H, et al. Delays in the diagnosis and treatment of lung cancer. Chest 2005;128:2282-8. [Crossref] [PubMed]
- Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 2006;355:2542-50. [Crossref] [PubMed]
- Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol 2008;26:3543-51. [Crossref] [PubMed]
- Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244-85. [Crossref] [PubMed]
- Pao W, Girard N. New driver mutations in non-small-cell lung cancer. Lancet Oncol 2011;12:175-80. [Crossref] [PubMed]
- Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e211S-50S.
- Gompelmann D, Herth FJ. Role of endobronchial and endoscopic ultrasound in pulmonary medicine. Respiration 2014;87:3-8. [Crossref] [PubMed]
- Kurimoto N, Murayama M, Yoshioka S, et al. Assessment of usefulness of endobronchial ultrasonography in determination of depth of tracheobronchial tumor invasion. Chest 1999;115:1500-6. [Crossref] [PubMed]
- Gould MK, Fletcher J, Iannettoni MD, et al. Evaluation of patients with pulmonary nodules: when is it lung cancer? ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:108s-30s.
- Rivera MP, Mehta AC. Initial diagnosis of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:131s-48s.
- Baaklini WA, Reinoso MA, Gorin AB, et al. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest 2000;117:1049-54. [Crossref] [PubMed]
- Steinfort DP, Khor YH, Manser RL, et al. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: systematic review and meta-analysis. Eur Respir J 2011;37:902-10. [Crossref] [PubMed]
- Wang Memoli JS, Nietert PJ, Silvestri GA. Meta-analysis of guided bronchoscopy for the evaluation of the pulmonary nodule. Chest 2012;142:385-93. [Crossref] [PubMed]
- Triller N, Dimitrijevic J, Rozman A. A comparative study on endobronchial ultrasound-guided and fluoroscopic-guided transbronchial lung biopsy of peripheral pulmonary lesions. Respir Med 2011;105 Suppl 1:S74-7. [Crossref] [PubMed]
- Sánchez-Font A, Giralt L, Vollmer I, et al. Endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions. A controlled study with fluoroscopy. Arch Bronconeumol 2014;50:166-71. [Crossref] [PubMed]
- Kurimoto N, Miyazawa T, Okimasa S, et al. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest 2004;126:959-65. [Crossref] [PubMed]
- Chao TY, Chien MT, Lie CH, et al. Endobronchial ultrasonography-guided transbronchial needle aspiration increases the diagnostic yield of peripheral pulmonary lesions: a randomized trial. Chest 2009;136:229-36. [Crossref] [PubMed]
- Hayama M, Izumo T, Chavez C, et al. Additional transbronchial needle aspiration through a guide sheath (GS-TBNA) for peripheral pulmonary lesions that cannot be detected by radial EBUS. Clin Respir J 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Zaric B, Stojsic V, Carapic V, et al. Radial Endobronchial Ultrasound (EBUS) Guided Suction Catheter-Biopsy in Histological Diagnosis of Peripheral Pulmonary Lesions. J Cancer 2016;7:7-13. [Crossref] [PubMed]
- Schuhmann M, Bostanci K, Bugalho A, et al. Endobronchial ultrasound-guided cryobiopsies in peripheral pulmonary lesions: a feasibility study. Eur Respir J 2014;43:233-9. [Crossref] [PubMed]
- Franke KJ, Nilius G, Ruehle KH, et al. The cryo-needle: a new tool for histological biopsies. A feasibility study. Lung 2013;191:611-7. [Crossref] [PubMed]
- Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e142S-65S.
- Asahina H, Yamazaki K, Onodera Y, et al. Transbronchial biopsy using endobronchial ultrasonography with a guide sheath and virtual bronchoscopic navigation. Chest 2005;128:1761-5. [Crossref] [PubMed]
- Asano F, Eberhardt R, Herth FJ. Virtual bronchoscopic navigation for peripheral pulmonary lesions. Respiration 2014;88:430-40. [PubMed]
- Eberhardt R, Anantham D, Ernst A, et al. Multimodality bronchoscopic diagnosis of peripheral lung lesions: a randomized controlled trial. Am J Respir Crit Care Med 2007;176:36-41. [Crossref] [PubMed]
- Oki M, Saka H, Ando M, et al. Ultrathin Bronchoscopy with Multimodal Devices for Peripheral Pulmonary Lesions. A Randomized Trial. Am J Respir Crit Care Med 2015;192:468-76. [Crossref] [PubMed]
- Kuo CH, Lin SM, Chen HC, et al. Diagnosis of peripheral lung cancer with three echoic features via endobronchial ultrasound. Chest 2007;132:922-9. [Crossref] [PubMed]
- Lie CH, Chao TY, Chung YH, et al. New image characteristics in endobronchial ultrasonography for differentiating peripheral pulmonary lesions. Ultrasound Med Biol 2009;35:376-81. [Crossref] [PubMed]
- Chen CH, Cheng WC, Wu BR, et al. Improved diagnostic yield of bronchoscopy in peripheral pulmonary lesions: combination of radial probe endobronchial ultrasound and rapid on-site evaluation. J Thorac Dis 2015;7:S418-25. [PubMed]
- Yamada N, Yamazaki K, Kurimoto N, et al. Factors related to diagnostic yield of transbronchial biopsy using endobronchial ultrasonography with a guide sheath in small peripheral pulmonary lesions. Chest 2007;132:603-8. [Crossref] [PubMed]
- Huang CT, Tsai YJ, Liao WY, et al. Endobronchial ultrasound-guided transbronchial biopsy of peripheral pulmonary lesions: how many specimens are necessary? Respiration 2012;84:128-34. [Crossref] [PubMed]
- Huang CT, Ruan SY, Liao WY, et al. Risk factors of pneumothorax after endobronchial ultrasound-guided transbronchial biopsy for peripheral lung lesions. PloS one 2012;7:e49125. [Crossref] [PubMed]
- Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest 2004;126:122-8. [Crossref] [PubMed]
- Lloyd C, Silvestri GA. Mediastinal staging of non-small-cell lung cancer. Cancer Control 2001;8:311-7. [PubMed]
- Harrow EM, Abi-Saleh W, Blum J, et al. The utility of transbronchial needle aspiration in the staging of bronchogenic carcinoma. Am J Respir Crit Care Med 2000;161:601-7. [Crossref] [PubMed]
- Garpestad E, Goldberg S, Herth F, et al. CT fluoroscopy guidance for transbronchial needle aspiration: an experience in 35 patients. Chest 2001;119:329-32. [Crossref] [PubMed]
- Herth F, Becker HD, Ernst A. Conventional vs endobronchial ultrasound-guided transbronchial needle aspiration: a randomized trial. Chest 2004;125:322-5. [Crossref] [PubMed]
- Annema JT, van Meerbeeck JP, Rintoul RC, et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: a randomized trial. JAMA 2010;304:2245-52. [Crossref] [PubMed]
- De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
- Um SW, Kim HK, Jung SH, et al. Endobronchial ultrasound versus mediastinoscopy for mediastinal nodal staging of non-small-cell lung cancer. J Thorac Oncol 2015;10:331-7. [Crossref] [PubMed]
- Adams K, Shah PL, Edmonds L, et al. Test performance of endobronchial ultrasound and transbronchial needle aspiration biopsy for mediastinal staging in patients with lung cancer: systematic review and meta-analysis. Thorax 2009;64:757-62. [Crossref] [PubMed]
- Ernst A, Anantham D, Eberhardt R, et al. Diagnosis of mediastinal adenopathy-real-time endobronchial ultrasound guided needle aspiration versus mediastinoscopy. J Thorac Oncol 2008;3:577-82. [Crossref] [PubMed]
- Pretreatment evaluation of non-small-cell lung cancer. The American Thoracic Society and The European Respiratory Society. Am J Respir Crit Care Med 1997;156:320-32. [Crossref] [PubMed]
- Pieterman RM, van Putten JW, Meuzelaar JJ, et al. Preoperative staging of non-small-cell lung cancer with positron-emission tomography. N Engl J Med 2000;343:254-61. [Crossref] [PubMed]
- Herth FJ, Eberhardt R, Krasnik M, et al. Endobronchial ultrasound-guided transbronchial needle aspiration of lymph nodes in the radiologically and positron emission tomography-normal mediastinum in patients with lung cancer. Chest 2008;133:887-91. [Crossref] [PubMed]
- Kuo CH, Chen HC, Chung FT, et al. Diagnostic value of EBUS-TBNA for lung cancer with non-enlarged lymph nodes: a study in a tuberculosis-endemic country. PloS one 2011;6:e16877. [Crossref] [PubMed]
- Ong P, Grosu H, Eapen GA, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for systematic nodal staging of lung cancer in patients with N0 disease by computed tomography and integrated positron emission tomography-computed tomography. Ann Am Thorac Soc 2015;12:415-9. [Crossref] [PubMed]
- Hishida T, Yoshida J, Nishimura M, et al. Problems in the current diagnostic standards of clinical N1 non-small cell lung cancer. Thorax 2008;63:526-31. [Crossref] [PubMed]
- Wang J, Welch K, Wang L, et al. Negative predictive value of positron emission tomography and computed tomography for stage T1-2N0 non-small-cell lung cancer: a meta-analysis. Clin Lung Cancer 2012;13:81-9. [Crossref] [PubMed]
- Lee PC, Port JL, Korst RJ, et al. Risk factors for occult mediastinal metastases in clinical stage I non-small cell lung cancer. Ann Thorac Surg 2007;84:177-81. [Crossref] [PubMed]
- Yarmus LB, Akulian J, Lechtzin N, et al. Comparison of 21-gauge and 22-gauge aspiration needle in endobronchial ultrasound-guided transbronchial needle aspiration: results of the American College of Chest Physicians Quality Improvement Registry, Education, and Evaluation Registry. Chest 2013;143:1036-43. [Crossref] [PubMed]
- Herth FJ, Schuler H, Gompelmann D, et al. Endobronchial ultrasound-guided lymph node biopsy with transbronchial needle forceps: a pilot study. Eur Respir J 2012;39:373-7. [Crossref] [PubMed]
- Ost DE, Ernst A, Lei X, et al. Diagnostic yield of endobronchial ultrasound-guided transbronchial needle aspiration: results of the AQuIRE Bronchoscopy Registry. Chest 2011;140:1557-66. [Crossref] [PubMed]
- Davoudi M, Colt HG, Osann KE, et al. Endobronchial ultrasound skills and tasks assessment tool: assessing the validity evidence for a test of endobronchial ultrasound-guided transbronchial needle aspiration operator skill. Am J Respir Crit Care Med 2012;186:773-9. [Crossref] [PubMed]
- Fujiwara T, Yasufuku K, Nakajima T, et al. The utility of sonographic features during endobronchial ultrasound-guided transbronchial needle aspiration for lymph node staging in patients with lung cancer: a standard endobronchial ultrasound image classification system. Chest 2010;138:641-7. [Crossref] [PubMed]
- Nakajima T, Anayama T, Shingyoji M, et al. Vascular image patterns of lymph nodes for the prediction of metastatic disease during EBUS-TBNA for mediastinal staging of lung cancer. J Thorac Oncol 2012;7:1009-14. [Crossref] [PubMed]
- Izumo T, Kirita T, Ariji E, et al. General rules for clinical and pathological studies on oral cancer: a synopsis. Jpn J Clin Oncol 2012;42:1099-109. [Crossref] [PubMed]
- Lee HS, Lee GK, Lee HS, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration in mediastinal staging of non-small cell lung cancer: how many aspirations per target lymph node station? Chest 2008;134:368-74. [Crossref] [PubMed]
- Navani N, Nankivell M, Lawrence DR, et al. Lung cancer diagnosis and staging with endobronchial ultrasound-guided transbronchial needle aspiration compared with conventional approaches: an open-label, pragmatic, randomised controlled trial. Lancet Respir Med 2015;3:282-9. [Crossref] [PubMed]
- Yarmus L, Akulian J, Ortiz R, et al. A randomized controlled trial evaluating airway inspection effectiveness during endobronchial ultrasound bronchoscopy. J Thorac Dis 2015;7:1825-32. [PubMed]
- Asano F, Aoe M, Ohsaki Y, et al. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: a nationwide survey by the Japan Society for Respiratory Endoscopy. Respir Res 2013;14:50. [Crossref] [PubMed]
- Micames CG, McCrory DC, Pavey DA, et al. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and metaanalysis. Chest 2007;131:539-48. [Crossref] [PubMed]
- Nakajima T, Yasufuku K, Takahashi R, et al. Comparison of 21-gauge and 22-gauge aspiration needle during endobronchial ultrasound-guided transbronchial needle aspiration. Respirology 2011;16:90-4. [Crossref] [PubMed]
- Yarmus LB, Arias S, Feller-Kopman D, et al. Electromagnetic navigation transthoracic needle aspiration for the diagnosis of pulmonary nodules: a safety and feasibility pilot study. J Thorac Dis 2016;8:186-94. [PubMed]


