
Preoperative localization of pulmonary nodules by electromagnetic navigation bronchoscopy combined with methylene blue injection
Highlight box
Key findings
• Electromagnetic navigation bronchoscopy (ENB)-guided methylene blue marking is an effective method of localizing pulmonary nodules.
• Only one complication was observed in our study cohort of 61 patients (1.64%), which was a patient who sustained pulmonary hemorrhage during ENB bronchoscopy.
• The univariate and multivariate logistic regression analyses showed that the node location and location mode had significant effects on the navigation time.
What is known, and what is new?
• The ENB-guided location of pulmonary nodules has been shown to be an effective, safe, and minimally invasive technology. However, the factors affecting the navigation time in pulmonary nodule localization using ENB-guided methylene blue injection remain unclear.
• This study evaluated the clinical efficacy and safety of methylene blue marking localization under the guidance of ENB, and further investigated the factors affecting navigation time.
What is the implication, and what should change now?
• Methylene blue injection guided by ENB is a promising option for the preoperative localization of pulmonary nodules. Greater experience at setting the target and selecting the location mode is necessary to enhance the accuracy of ENB-guided dye localization and to standardize the procedure. The shorter navigation time will be achieved at the later phase of the learning process of ENB localization.
Introduction
Based on GLOBOCAN 2022 estimates, lung cancer was the most frequently diagnosed cancer and the leading cause of cancer-related death globally (1). The early diagnosis of lung cancer contributes to improving patient prognosis and survival (2). Based on a large-scale real-world Chinese sample of 26,226 cases, the 5-year survival rates of stages I, II, III, and IV lung cancer were 84.20%, 56.41%, 34.39%, and 18.41%, respectively (3). Therefore, early detection and treatment of lung cancer are crucial to survival (4). Pure ground-glass nodules and sub-solid nodules are difficult to detect during surgery. Due to the deviation in terms of location of lesions before and after the collapse of the lungs, preoperative CT scan images was difficult to locate the pulmonary nodules accurately (5).
Electromagnetic navigation bronchoscopy (ENB) is a transbronchial location tool that can assist in the minimally invasive resection of peripheral pulmonary nodules, and is recommended for use in the biopsy of peripheral pulmonary nodule lesions for definitive diagnosis (5,6). It combines three-dimensional (3D) reconstruction technology and magnetic navigation with bronchoscopy to reach deep into grade 12 to 14 bronchi and realize the real-time navigation and accurate localization of lung lesions (7). ENB has gained increasing popularity, as it has advanced the preoperative marking of small pulmonary nodules, is highly effective, and is low risk (8,9). The prospective, multicenter Navigate study (10) showed that ENB-aided diagnosis can be obtained concomitantly in approximately 75% of patients undergoing ENB-guided biopsy and has a low procedural complication rate.
In this study, we sought to evaluate the clinical efficiency and safety of using ENB combined with methylene blue marking for the preoperative localization of pulmonary nodules, and to further investigate the factors affecting navigation time. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1358/rc).
Methods
Patients
From October 2021 to February 2022, patients who had been diagnosed with pulmonary nodules, and underwent ENB-guided preoperative localization followed by surgery, were enrolled for the study. The inclusion criteria were: (I) small pulmonary lesions (diameter ≤8 mm) were presumed to be undetectable and unpalpable based on the surgeon’s experience and the presence of two or more pulmonary nodules; (II) pulmonary lesions (diameter >8 mm) located >10 mm deep from the pleural surface. Patients allergic to methylene blue were excluded. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Shanghai General Hospital (No. 2021KY175). Informed consent was obtained from all the participants.
ENB location and surgery
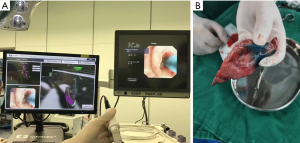
All the ENB procedures used the superDimensionTM navigation system (version 7.0) in accordance with the manufacturer’s instructions (and as described previously) (11,12). General anesthesia with intubation in a supine position was performed first before surgery. A chest computed tomography scan was performed to generate a 3D channel before the ENB operation. Based on the already established route to access the pulmonary, every nodule was successfully located with the help of a navigation console system, locatable electromagnetic catheter, and extended injection catheter. And then, the electromagnetic guide catheter was removed, and the extended injection catheter was left (11-13). 0.2–0.8 mL of methylene blue and the appropriate amount of air was then injected. The operating process is shown in Figure 1. The pulmonary nodules were resected according to the staining markers. All patients were scheduled to undergo VATS surgical procedures including wedge resection, segmentectomy, and lobectomy after localization.
Statistical analysis
The data are expressed as the total number with the percentage for the categorical variables, and as the median [interquartile range (IQR)] for the continuous variables. After the single-factor analysis, the relevant factors affecting the navigation time were screened, and a multi-factor analysis was conducted. Data analysis was performed using SAS 9.4 version. All P values <0.05 were considered statistically significant.
Results
Characteristics of the patients
In total, 61 patients were included in the study from October 2021 to February 2022. The median age of the patients was 60 (IQR, 18) years, and 36 (59.02%) were women. The median body mass index of the patients was 24 (IQR, 3.6) kg/m2. Of the 61 patients, the majority of patients (70.69%) had two or more nodules. Nine patients had emphysema, and two patients had pulmonary bulla (Table 1).
Table 1
| Parameters | Patient data (n=61) |
|---|---|
| Age (years) | 60 [18] |
| ≥60 | 33 (54.10) |
| <60 | 28 (45.90) |
| Gender | |
| Male | 25 (40.98) |
| Female | 36 (59.02) |
| Active smoking | 21 (34.40) |
| Male | 18 (72.0) |
| Female | 3 (8.33) |
| Body mass index (kg/m2) | 24 [3.6] |
| Pulmonary function | |
| FEV1 (L) | 2.34 [0.89] |
| FVC (L) | 2.88 [1.28] |
| Missing | 16 |
| Nodules per patient | |
| 1 | 17 (29.31) |
| ≥2 | 41 (70.69) |
| Missing | 3 |
| Emphysema | 9 (14.75) |
| Pulmonary bulla | 2 (3.28) |
Data are presented as median [interquartile range], n (%) or n. FVC, forced vital capacity; FEV1, forced expiratory volume in 1 second.
Characteristics of pulmonary nodules
ENB localization was performed on 170 nodules in 61 patients. The characteristics of the pulmonary nodules are summarized in Table 2. The pulmonary nodules were most commonly located in the right upper lobe (38.92%), followed by the left lower lobe (19.76%), left upper lobe (17.96%), right lower lobe (14.97%), right middle lobe (6.59%), and left middle lobe (1.80%). A large proportion of nodules were pure ground-glass opacity nodules (14, 25.00%) and mixed ground-glass opacity nodules (27, 48.21%).
Table 2
| Parameters | Nodule data (n=170) |
|---|---|
| Nodule size (mm) | 58 [3] |
| <5 | 58 (34.12) |
| 5−8 | 45 (26.47) |
| >8 | 67 (39.41) |
| Maximum diameter (mm) | 10 [8] |
| Unilateral/bilateral lung nodules | |
| Unilateral | 25 (43.10) |
| Bilateral | 33 (56.90) |
| Missing | 3 |
| Location of lung nodules | |
| Right upper lobe | 65 (38.92) |
| Right middle lobe | 11 (6.59) |
| Right lower lobe | 25 (14.97) |
| Left upper lobe | 30 (17.96) |
| Left middle lobe | 3 (1.80) |
| Left lower lobe | 33 (19.76) |
| Missing | 3 |
| Characteristics | |
| Mixed ground-glass nodule | 27 (48.21) |
| Pure ground-glass nodule | 14 (25.00) |
| Solid nodule | 10 (17.86) |
| Other | 5 (8.93) |
| Missing | 5 |
Data are presented as median [interquartile range], n (%) or n.
Localization and operative results
Patients were injected with 0.5 (IQR, 0.1) mL of methylene blue dye. The median ENB navigation time was 10.5 (IQR, 6) min. The median distance from the target nodule was 0.9 (IQR, 0.6) cm. Pulmonary hemorrhage occurred in one patient (1.64%), and no other complication directly related to ENB-guided localization was observed in this study. Postoperative pathology was performed on each resected nodule. The pathological results are shown in Table 3. There were 27 cases of minimally invasive adenocarcinoma, 16 cases of invasive adenocarcinoma, and 14 cases of benign lesion.
Table 3
| Parameters | Value |
|---|---|
| Navigation time (min) | 10.5 [6] |
| Dose of methylene blue (mL) | 0.5 [0.1] |
| Location mode | |
| Perinodular | 43 (70.49) |
| Pleura | 16 (26.23) |
| Midnodular | 2 (3.28) |
| Distance from the target nodule (cm) | 0.9 [0.6] |
| Operation mode | |
| Segmentectomy | 11 (18.03) |
| Lobectomy | 10 (16.39) |
| Wedge resection | 40 (65.57) |
| Surgery time (min) | 140 [55] |
| Complications | |
| Hemorrhage | 1 (1.64) |
| Pneumothorax | 0 |
| Pathological diagnosis | |
| MIA | 27 (44.26) |
| IA | 16 (26.23) |
| Benign | 14 (22.95) |
| Highly differentiated adenocarcinoma | 1 (1.64) |
| Bronchial adenocarcinoma | 1 (1.64) |
| Poorly differentiated squamous cell carcinoma | 1 (1.64) |
| Small cell neuroendocrine carcinoma | 1 (1.64) |
| Adenocarcinoma | 2 (3.28) |
| Squamous carcinoma | 1 (1.64) |
| Navigation success | 66 (92.96) |
| Location success | 70 (95.89) |
Data are presented as median [interquartile range] or n (%). MIA, minimally invasive adenocarcinoma; IA, invasive adenocarcinoma.
Relevant factors influencing the navigation time
The factors affecting the navigation time based on the univariate analysis are shown in Table 4. Age, sex, methylene blue dose, node location, node size, distance from pleura, location mode, surgical experience, and breath were included in the univariate analysis. The results showed that the node location, location mode, and surgical experience affected the navigation time. The multivariate logistic regression analysis of the above-mentioned variables showed that the node location (P=0.001) and location mode (P=0.04) significantly affected the navigation time (Table 5).
Table 4
| Parameters | Navigation time, min | R | P value |
|---|---|---|---|
| Age (years) | 59.23 (14.16) | −0.19 | 0.15 |
| Sex | 0.96 | ||
| Male | 12.6 (6.09) | ||
| Female | 12.7 (10.18) | ||
| Dose of methylene blue (mL) | 0.09 | ||
| <0.3 | 15.6 (8.67) | ||
| 0.3−0.5 | 11.34 (5.37) | ||
| >0.5 | 15.22 (8.24) | ||
| Nodule location | <0.001 | ||
| Upper lobe | 10.4 (4.0) | ||
| Middle lobe | 9.67 (1.53) | ||
| Lower lobe | 11.9 (5.68) | ||
| Other | 21.67 (8.49) | ||
| Nodule size (mm) | 0.26 | ||
| <5 | − | ||
| 5−8 | 14.73 (6.07) | ||
| >8 | 12.18 (6.86) | ||
| Distance from pleura (mm) | 2.57 (4.15) | −0.07 | 0.65 |
| Location mode | 0.04 | ||
| Perinodular | 11.4 (6.23) | ||
| Pleura | 16.5 (6.98) | ||
| Midnodular | 12.0 (2.83) | ||
| Surgery experience | 0.02 | ||
| Year 2021 | 16.0 (6.6) | ||
| Year 2022 | 11.49 (6.3) | ||
| Breath | 0.29 | ||
| End-exhalation | 14.29 (7.58) | ||
| End-expiratory | 12.14 (6.31) | ||
Data are presented as mean (standard deviation).
Table 5
| Parameters | Type III sums of squares | Mean square | F value | P value |
|---|---|---|---|---|
| Age | 32.89 | 32.89 | 1.15 | 0.29 |
| Sex | 0.03 | 0.03 | 0.00 | 0.97 |
| Dose of methylene blue | 45.26 | 22.63 | 0.79 | 0.46 |
| Nodule location | 604.20 | 201.40 | 7.05 | 0.001 |
| Nodule size | 47.65 | 47.65 | 1.67 | 0.20 |
| Location mode | 206.47 | 103.23 | 3.61 | 0.04 |
| Distance from pleura | 9.17 | 9.17 | 0.32 | 0.57 |
| Breath | 25.60 | 25.60 | 0.90 | 0.35 |
Discussion
In this study, ENB guidance and methylene blue injection were performed on 170 nodules in 61 patients. Of the patients, 41 (70.69%) had more than two nodules. The median ENB navigation time was 10.5 (IQR, 6) min. The navigation success rate was 92.96%, and the ENB location success rate was 95.89%. During the study, only one case of pulmonary hemorrhage directly related to ENB-guided localization was observed in the participants. The results of this study showed that the ENB-guided methylene blue marking of pulmonary nodules can effectively and safely localize and mark pulmonary nodules. As previously reported, the application of methylene blue injection guided by ENB in the localization of pulmonary nodules is an accurate and safe method for successful minimally-invasive surgery of multiple pulmonary nodules (12,14).
ENB has a considerable learning curve, and the success rate of ENB localization and localization accuracy increase significantly as experience with ENB technology increases (13). In this study, the shorter navigation time was achieved at the later phase of the learning process of ENB localization. Type of injected dye and the dye dosage also play an important role in ENB-guided location of pulmonary nodules. Indocyanine green is a near infrared fluorescent dye. It is necessary to use a near-infrared fluorescence thoracoscope for observation (4). Methylene blue is water soluble and easy to spread, and a small amount of methylene blue may lead to staining failure or difficulties in distinguishing nodules, while the over-injection of methylene blue may also cause diffuse staining and result in localization failure (15,16). A clinical analysis at a single center (17) recommended that 0.3–0.5 mL of methylene blue be applied in ENB-guided preoperative staining. In lung nodule located more than 5 mm from the pleural surface, an additional injection of no more than 0.5 mL methylene blue was used to mark the pleural surface with a 97.2% success rate, and extravasation of methylene blue into the pleural surface occurred in only two cases (18). Previous ENB-guided methylene blue studies (Table 6) have reported that ENB-guided methylene blue staining localization method is an accurate and safe modality.
Table 6
| First author (reference) | No. of patients | Dose of methylene blue (mL) | Mean navigation time (min) | Postoperative complications, n (%) |
|---|---|---|---|---|
| Wang LL (4) | 25 | 0.2–1.0 | 12.6 | 2 (8.0) |
| Awais O (9) | 29 | 0.5 | 9.7 | 0 |
| Yao YS (13) | 20 | 1.5 | NA | 0 |
| Cheng X (17) | 79 | 0.15 | 10 | 5 (2.7) |
NA, not available; ENB, electromagnetic navigation bronchoscopy.
The location of pulmonary nodules and movement of the lung occurs with respiratory variation during bronchoscopy can affect ENB navigation (19,20). Hyun et al. reported that compared with targets in the middle or lower zones, the navigation time was longer in the upper zone, while the target distance remained relatively constant (19). Respiratory movement is another factor that influences navigation accuracy of ENB. Control of respiratory movements would enhance the accuracy of ENB navigation (20).
In this study, we conducted a univariate analysis to further investigate the factors affecting the navigation time, and found that the node location, location mode, and surgical experience affected the navigation time. The multivariate logistic regression analysis showed that the node location (P=0.001) and location mode (P=0.04) significantly affected the navigation time.
This study had a number of limitations. Notably, it used data from a single center. In the future, we will recruit more patients to further monitor the clinical effects and safety of ENB-guided methylene blue location and analyze any other relevant factors affecting the navigation time. Robotic-assisted bronchoscopy with advantage of an easier learning curve has recently emerged as an alternative to ENB for the evaluation of peripheral pulmonary lesions. The first known cluster randomized pragmatic trial in the interventional pulmonology field (RELIAN) will elucidate whether it has comparable diagnostic utility as ENB in the future (21).
Conclusions
ENB-guided preoperative methylene blue location has a high localization success rate and a low complication rate, which proves that it is a safe and effective method for the accurate identification and successful resection of small pulmonary nodules. Methylene blue injection guided by ENB is a promising option for the preoperative localization of pulmonary nodules. In addition, the node location and location mode had significant effects on the navigation time.
Acknowledgments
The authors would like to thank all the patients for providing their data.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1358/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1358/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1358/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1358/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Shanghai General Hospital (No. 2021KY175) and informed consent was obtained from all the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2024;74:229-63. [Crossref] [PubMed]
- Yang WH, Xu TQ, Zhang Y, et al. Application of Electromagnetic Navigation Bronchoscopy in the early diagnosis and treatment of lung cancer: a narrative review. Transl Cancer Res 2021;10:1583-93. [Crossref] [PubMed]
- Wang C, Shao J, Song L, et al. Persistent increase and improved survival of stage I lung cancer based on a large-scale real-world sample of 26,226 cases. Chin Med J (Engl) 2023;136:1937-48. [Crossref] [PubMed]
- Wang LL, He BF, Cui JH, et al. Electromagnetic navigational bronchoscopy-directed dye marking for locating pulmonary nodules. Postgrad Med J 2020;96:674-9. [Crossref] [PubMed]
- Qian K, Deng Y, Shen C, et al. Combination of electromagnetic navigation bronchoscopy-guided biopsy with a novel staining for peripheral pulmonary lesions. World J Surg Oncol 2019;17:158. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2022;20:497-530. [Crossref] [PubMed]
- Geraci TC, Ferrari-Light D, Kent A, et al. Technique, Outcomes With Navigational Bronchoscopy Using Indocyanine Green for Robotic Segmentectomy. Ann Thorac Surg 2019;108:363-9. [Crossref] [PubMed]
- Mehta AC, Hood KL, Schwarz Y, et al. The Evolutional History of Electromagnetic Navigation Bronchoscopy: State of the Art. Chest 2018;154:935-47. [Crossref] [PubMed]
- Awais O, Reidy MR, Mehta K, et al. Electromagnetic Navigation Bronchoscopy-Guided Dye Marking for Thoracoscopic Resection of Pulmonary Nodules. Ann Thorac Surg 2016;102:223-9. [Crossref] [PubMed]
- Abbas A, Kadakia S, Ambur V, et al. Intraoperative electromagnetic navigational bronchoscopic localization of small, deep, or subsolid pulmonary nodules. J Thorac Cardiovasc Surg 2017;153:1581-90. [Crossref] [PubMed]
- Folch EE, Pritchett MA, Nead MA, et al. Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary Lesions: One-Year Results of the Prospective, Multicenter NAVIGATE Study. J Thorac Oncol 2019;14:445-58. [Crossref] [PubMed]
- Zeng C, Yang G, Wei L, et al. Accurate and non-invasive localization of multi-focal ground-glass opacities via electromagnetic navigation bronchoscopy assisting video-assisted thoracoscopic surgery: a single-center study. Front Oncol 2023;13:1255937. [Crossref] [PubMed]
- Yao YS, Xuan HJ, Chen CJ, et al. Feasibility of electromagnetic navigation bronchoscopy-guided injection of methylene blue in locating the multiple pulmonary nodules: a case series analysis. Indian J Surg 2023; [Crossref]
- Yang Q, Han K, Lv S, et al. Virtual navigation bronchoscopy-guided intraoperative indocyanine green localization in simultaneous surgery for multiple pulmonary nodules. Thorac Cancer 2022;13:2879-89. [Crossref] [PubMed]
- Sun J, Mao X, Xie F, et al. Electromagnetic navigation bronchoscopy guided injection of methylene blue combined with hookwire for preoperative localization of small pulmonary lesions in thoracoscopic surgery. J Thorac Dis 2015;7:E652-6. [Crossref] [PubMed]
- Shi J, He J, He J, et al. Electromagnetic navigation-guided preoperative localization: the learning curve analysis. J Thorac Dis 2021;13:4339-48. [Crossref] [PubMed]
- Cheng X, Zhang YJ, Han DP, et al. Electromagnetic navigation bronchoscopy-guided preoperative localization of pulmonary nodules in 183 patients: a clinical analysis in a single center. Chinese Journal of Clinical Thoracic and Cardiovascular Surgery 2023;30:1539-44.
- Marino KA, Sullivan JL, Weksler B. Electromagnetic Navigation Bronchoscopy for Identifying Lung Nodules for Thoracoscopic Resection. Ann Thorac Surg 2016;102:454-7. [Crossref] [PubMed]
- Hyun K, Park IK, Song JW, et al. Electromagnetic navigation bronchoscopic dye marking for localization of small subsolid nodules: Retrospective observational study. Medicine (Baltimore) 2019;98:e14831. [Crossref] [PubMed]
- Chen A, Pastis N, Furukawa B, et al. The effect of respiratory motion on pulmonary nodule location during electromagnetic navigation bronchoscopy. Chest 2015;147:1275-81. [Crossref] [PubMed]
- Paez R, Lentz RJ, Salmon C, et al. Robotic versus Electromagnetic bronchoscopy for pulmonary LesIon AssessmeNT: the RELIANT pragmatic randomized trial. Trials 2024;25:66. [Crossref] [PubMed]


