Thick lung wedge resection for acute life-threatening massive hemoptysis due to aortobronchial fistula
Introduction
Aortobronchial fistula due to thoracic aortic aneurysm or dissection is extremely rare but potentially life-threatening condition. Early diagnosis and emergency surgery are the predictive factors for good outcomes. To rapidly control hemoptysis and secure airway, dividing the lung from the aortic dissection is important, but the adhering lung is also the last structure that prevents bleeding to free the thoracic cavity. Surgery has few difficulties due to ongoing bleeding, pulmonary hematoma, the hemodynamic instability, and complicated surgical approach due to severe adhesions from the adjacent tissue. Dissection of the adhesion has a high risk for massive bleeding. In addition, systemic lung resection, such as lobectomy and segmentectomy, is difficult during life-threatening situations.
Recent endostaplers have many cartridge sizes. We could use these to cut the thick part of lung parenchyma. We report a patient whose acute life-threatening massive hemoptysis due to aortobronchial fistula was successfully controlled by undergoing a simple and rapid thick wedge resection by using the black cartilage stapler before aortic replacement.
Case presentation
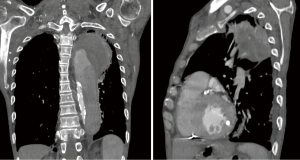
A 65-year-old man was admitted to our hospital for massive hemoptysis. The patient underwent ascending aorta replacement for chronic dissecting aneurysm two years previously and had hemodialysis for chronic renal failure. We performed tracheal intubation to secure the airway. The chest computed tomography revealed a ruptured aortic dissection from the distal arch to the descending aorta and hematoma in the apical-posterior segment of the left upper lobe and the superior segment of the lower lobe (S6) (Figure 1). We diagnosed rupture of the aortic dissection into the lung, and the patient underwent an emergency surgery on the same day.
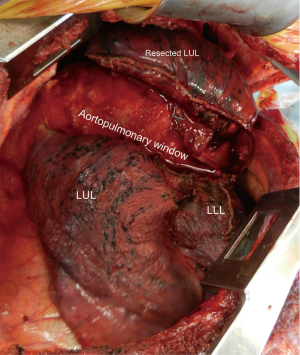
We performed posterolateral thoracotomy in the fourth intercostal space. A dissecting aorta approximately 80 mm in diameter with tight adhesion of the left upper lobe and S6 was found. The lung parenchyma expanded because of the hematoma. The rupture point could not be identified. We attempted dissecting the adhesions, but we discontinued because bleeding from the adhesion area increased. Subsequently, we performed wedge resection of the lung hematoma to divide the lung and aorta. We created a tunnel through the aortopulmonary window from the anterior side of the pulmonary hilum to the posterior side of the mediastinal pleural layer (Figure 2). We stapled the upper lobe and S6 along the aortopulmonary window by using the stapler for thick tissues (Endo GIA Black Reload, Covidien, Tokyo, Japan). The aortic dissection and left lung were isolated by the staplings; massive hemoptysis disappeared, and the complete aortic dissection appeared. The aortic dissection with adherent lung was excised, and graft replacement was performed. Stapling line had adequate strength to tolerate the bleeding pressure.
Although the surgery was successful, the condition of the patient deteriorated due to the metabolic disorder caused by chronic renal failure. He died 5 days postoperatively.
Discussion
Aortobronchial fistula is an anomalous communication between the aorta and lung. The major causes are thoracic aortic aneurysm with lung infection, pressure necrosis, atherosclerosis, trauma, and previous vascular surgery (1).
Aortobronchial fistula is a life-threatening condition. Major factors of the poor prognosis are the patient’s unstable condition, emergency of the repair, and presence of aortic wall infection (2). Various diagnostic tools, such as computed tomography, echocardiography, bronchoscopy, and aortography, are useful in diagnosing the aortobronchial fistula; the differential diagnosis established only 44–56% of all cases (3).
Surgery is a traditional method. Traditional procedures include opening the aneurysm, leaving the portion attached to the lung, and performing surgical repair of the aneurysm. Air leakage through the aortobronchial fistula was stopped by repairing from inside the aneurysm wall (4). Previous report suggested that the dissecting lung tissue adhering tightly to the aneurysm should be minimized to limit bleeding, air leakage, and pulmonary infection in the absence of obvious preoperative infection (4). Direct suturing of the lung is generally performed, but wedge resection, lobectomy, or pneumonectomy is needed in 25–50% of cases (1,5). Overall survival rate of the surgical cases ranged from 18–24% (6). Surgery of aortobronchial fistula has few difficulties due to the hemodynamic instability of patients, pulmonary hematoma, ongoing bleeding, and complicated surgical approach due to severe adhesions from the adjacent tissue (7). Because our patient deteriorated into a critical condition in a short time, we need to secure the airway and control the massive hemoptysis. In addition, adhesion between the aorta and lung was extensive; therefore, we chose lung hematoma wedge resection to divide the lung and dissected aorta.
We could use the black cartridge endostapler since 2012 in Japan. The Black cartridge endostapler is designed to create a secure staple line for thick tissues. It was useful for the proximal side lung wedge resection with hematoma of our case. Stapling is a simple and easy technique, and staples did not fail during firing, and the stapled visceral pleura have adequate strength to prevent the bleeding into the thoracic space.
Several roots for the dividing aorta and lung are found. We speculate that the aortopulmonary window is one of the appropriate and easy spaces. The aortopulmonary window is a small space between the aortic arch and the pulmonary artery, which is bounded by the aorta, pulmonary artery, and bronchus (8). Although this window is long and curved, this is the only location without adhesion between the dissected aorta and lung hematoma when surgeons create the tunnel. Surgeons could choose inside or outside of the mediastinal pleura due to the adhesions. We speculate that creating a tunnel outside of the mediastinal pleura has a lower risk for pulmonary artery injury.
Endovascular stent graft repair has been reported as a less-invasive treatment for the aortobronchial fistula for the last decade. This procedure could avoid thoracotomy, aortic clamping, and single-lung ventilation and has acceptable morbidity and mortality rates (2). However, endovascular stenting have the risk of endoleak, migration, left arm ischemia, and infection due to the direct communication with the contaminated airway. Recurrent hemorrhage occurred in 14% of patients from 2 weeks to 9 years after stenting, and long-term result remains unknown. Its indication and usefulness for aortic dissection is also still controversial.
In summary, thick lung wedge resection by using the black cartridge stapler is a simple and rapid method to control massive hemoptysis from aortic dissections; hence, this procedure is one of options to control massive hemoptysis due to aortobronchial fistula. This technique could stop massive hemoptysis rapidly and prevent the dissection of the adherent lung tissue and intra-thoracic infection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Favre JP, Gournier JP, Adham M, et al. Aortobronchial fistula: report of three cases and review of the literature. Surgery 1994;115:264-70. [PubMed]
- De Rango P, Estrera AL, Azizzadeh A, et al. Stent-graft repair of aortobronchial fistula: a review. J Endovasc Ther 2009;16:721-32. [Crossref] [PubMed]
- Oppenheimer R, Brotherton L. Aortobronchial fistula: a rare etiology for hemoptysis. Ear Nose Throat J 2002;81:257-9. [PubMed]
- Nishizawa J, Matsumoto M, Sugita T, et al. Surgical treatment of five patients with aortobronchial fistula in the aortic arch. Ann Thorac Surg 2004;77:1821-3. [Crossref] [PubMed]
- Liu SF, Chen YC, Lin MC, et al. Thoracic aortic aneurysm with aortobronchial fistula: a thirteen-year experience. Heart Lung 2004;33:119-23. [Crossref] [PubMed]
- Kokotsakis J, Misthos P, Athanasiou T, et al. Endovascular stenting for primary aortobronchial fistula in association with massive hemoptysis. Tex Heart Inst J 2007;34:369-72. [PubMed]
- Eren E, Keles C, Toker ME, et al. Surgical treatment of aortobronchial and aortoesophageal fistulae due to thoracic aortic aneurysm. Tex Heart Inst J 2005;32:522-8. [PubMed]
- Dewey M, Magid D, Wheeler PS, et al. Aortopulmonary window or angle on the chest radiograph? AJR Am J Roentgenol 2004;182:1085-6. [Crossref] [PubMed]


