
Comparative prognosis of long-term follow-up over 10 years and dropout from follow-up after resection of lung cancer
Highlight box
Key findings
• In patients with non-small cell lung cancer (NSCLC) after lung resection, age ≥75 years and female sex were risk factors for drop-out from follow-up >10 years. In addition, although age ≥75 years and with stage ≥2 disease were significantly associated with overall survival, patients ≥75 years of age have a high risk of death from other diseases. Sufficient consideration and informed consent for surgical indications are therefore necessary.
What is known and what is new?
• Precisely how long lung cancer patients should be followed up after resection remains unclear.
• In patients with NSCLC after lung resection, age ≥75 years and female sex were risk factors for drop-out from follow-up >10 years. In addition, although age ≥75 years and with stage ≥2 disease were significantly associated with overall survival, patients ≥75 years of age have a high risk of death from other diseases.
What is the implication, and what should change now?
• This study adds novel insights into the factors influencing follow-up adherence, which is crucial for optimizing long-term outcomes in NSCLC patients.
Introduction
Generally, completing 5 years of follow-up after complete resection of a non-small cell lung cancer (NSCLC) might be sufficient to declare that a patient with lung cancer as cured (1,2). On the other hand, 11% of all cases reportedly developed late recurrence more than 5 years after lung cancer resection (3). It has also been reported that the probability of having died due to lung cancer continued to increase even if it has been more than five years since the operation (4). In addition, second primary lung cancers are detected among long-term survivors (5). That is to say, precisely how long lung cancer patients should be followed up after resection remains unclear.
In addition, prognosis after resection of NSCLC was found to not differ significantly between elderly patients >70 years and young patients (6). With that being said, sublobar resection may be preferable to lobectomy for elderly NSCLC patients (7,8). In particular, few studies have examined the long-term prognosis of elderly patients with NSCLC, and no reports have investigated drop-out from follow-up after resection of NSCLC, including in elderly patients. Elderly patients tend to become unable or unwilling to attend hospital follow-up visits year after year.
This study aimed to address the gap in the literature by investigating the long-term prognosis and drop-out from follow-up in cases of resected NSCLC, including elderly patients. Specifically, the primary aim was to examine the prognosis of long-term follow-up over 10 years including elderly patients and to investigate factors associated with drop-out from follow-up after NSCLC resection in our institution. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-909/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval for this study was granted by the ethics committee of Hokkaido Cancer Center (approval No. 03-26; date of approval: October 13, 2021); the requirement to obtain informed consent directly was waived for this retrospective study, and informed consent was obtained in the form of opt-out on the website of our institution. This retrospective cohort study reviewed the records of consecutive patients who underwent lung resection for lung cancer at Hokkaido Cancer Center in Sapporo, Japan, between January 1, 2009 and March 31, 2011. We included patients who had at least one follow-up visit after surgery. We investigated the postoperative recurrence of cases as of December 2022. Cases of recurrence of past lung carcinoma, exploratory thoracotomy, small cell carcinoma, malignant lymphoma with pulmonary metastasis and second surgery during the study period were excluded.
Clinical, and perioperative characteristics encompassed age, sex, performance status, body mass index, American Society of Anesthesiologists classification, forced expiratory volume in 1 s, smoking history, comorbidities, number of preoperative oral medications, tumor diameter, surgical approach, type of resection, blood loss, surgery duration, preoperative therapy, postoperative therapy, and pathological findings.
In our institution, a multidisciplinary team, including thoracic surgeons, radiologists, and oncologists, reviewed each case to ensure accurate staging based on clinical and imaging data. When mediastinal lymph node metastasis was suggested, we performed transbronchial nodal biopsy as possible. Staging of NSCLC was performed using the 7th edition of International Union for Cancer Control TNM staging system. Postoperative morbidity was assessed using Clavien-Dindo classification. We investigated whether preoperative or postoperative therapy was received by the patients (e.g., chemotherapy, radiotherapy or chemoradiotherapy).
We investigated all patients in whom recurrence was detected on physical examination, chest radiography, computed tomography (CT), or blood examination including tumor markers during follow-up every 6 months for 5 years. Patients were then followed up using CT once a year after follow-up of 5 years even if more than 10 years later. A diagnosis of recurrence was determined by multidisciplinary discussion using risk of recurrence, clinical course, and results from various imaging modalities and biopsy. Local relapse was defined as tumor relapse in the ipsilateral thorax, which included the resection margin of the lung lymph node or bronchus, hilar lymph nodes, mediastinal lymph nodes, and malignant pleural effusion. Confirmation of survival or death of patients who were lost to follow-up was performed by telephone interview or documentation from patients or the public office. Missing cases even after these methods were defined as drop-out cases.
Pulmonary resection of lung carcinoma was performed for 349 cases during this study period. In total, 327 patients were included in this analysis (Figure 1). The primary aim was to examine the prognosis of long-term follow-up over 10 years and drop-out from follow-up after resection of NSCLC and to investigate factors associated with drop-out from follow-up after NSCLC resection in our institution. The secondary aim was to compare overall survival and disease-specific survival of long-term follow-up (over 10 years) between elderly (≥75 years) and younger patients (<75 years) and to investigate factors associated with overall survival.
Statistical analysis
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, EZR is a modified version of R Commander designed to add statistical functions frequently used in biostatistics. The chi-square test, Fisher’s exact test, and Mann-Whitney U test were used for statistical analyses.
For exploratory analyses, logistic regression models were prepared to determine associations between clinical characteristics and drop out from follow-up in all cases. The final multivariable model included those variables for which the statistical significance was P≤0.10 in univariate analysis. Values of P<0.05 were considered significant.
Overall survival and disease-specific survival were analyzed using Kaplan-Meier curves and log-rank test. Factors associated with overall survival were explored using Cox hazard models.
Results
Follow-up over 10 years was achieved in 246 cases, while 81 cases dropped out. Between cases with follow-up over 10 years and cases of drop-out, univariate analyses showed significant differences in sex, age, tumor status on CT, tumor diameter, solid diameter, clinical stage, surgical approach, operative time, bleeding, lymphatic invasion, pleural invasion, pathological stage and postoperative therapy (Table 1).
Table 1
| Characteristics | Follow-up cases (n=246) | Drop-out cases (n=81) | P value |
|---|---|---|---|
| Sex | 0.001 | ||
| Male | 140 (56.9) | 29 (35.8) | |
| Female | 106 (43.1) | 52 (64.2) | |
| Age (years) | 67.00 [39.00, 90.00] | 74.00 [16.00, 86.00] | 0.003 |
| BMI (kg/m2) | 22.68 [14.74, 32.89] | 22.72 [16.19, 35.30] | 0.89 |
| PS | |||
| 0 | 212 (86.2) | 75 (92.6) | 0.07 |
| 1 | 33 (13.4) | 5 (6.2) | |
| 2 | 1 (0.4) | 0 (0.0) | |
| 4 | 0 (0.0) | 1 (1.2) | |
| ASA classification | 0.60 | ||
| 1 | 28 (11.4) | 6 (7.4) | |
| 2 | 199 (80.9) | 70 (86.4) | |
| 3 | 19 (7.7) | 5 (6.2) | |
| Smoking | 0.12 | ||
| Never | 88 (35.8) | 39 (48.1) | |
| Ex-smoker | 100 (40.7) | 29 (35.8) | |
| Current smoker | 58 (23.6) | 13 (16.0) | |
| COPD | 47 (19.1) | 15 (18.5) | >0.99 |
| Hypertension | 101 (41.1) | 41 (50.6) | 0.16 |
| Dyslipidemia | 61 (24.8) | 26 (32.1) | 0.20 |
| Diabetes mellitus | 26 (10.6) | 14 (17.3) | 0.12 |
| Cardiovascular | 34 (13.8) | 6 (7.4) | 0.17 |
| Cerebral infarction | 17 (6.9) | 10 (12.3) | 0.16 |
| Dementia | 2 (0.8) | 0 (0.0) | >0.99 |
| Number of preoperative oral medications | 3.00 [0.00, 15.00] | 3.00 [0.00, 23.00] | 0.19 |
| Preoperative FEV1 (mL) | 2,175.00 [1,050.00, 4,050.00] | 2,080.00 [1,170.00, 4,190.00] | 0.16 |
| Tumor on CT | 0.03 | ||
| Pure ground glass type | 11 (4.5) | 8 (9.9) | |
| Partially solid type | 48 (19.5) | 23 (28.4) | |
| Solid type | 187 (76.0) | 50 (61.7) | |
| Solid diameter (mm) | 23.00 [0.00, 120.00] | 18.00 [0.00, 56.00] | 0.001 |
| Solid diameter >20 mm | 136 (55.3) | 29 (35.8) | 0.003 |
| Tumor diameter (mm) | 25.00 [3.00, 120.00] | 22.00 [8.00, 56.00] | 0.01 |
| Tumor diameter >30 mm | 92 (37.4) | 20 (24.7) | 0.043 |
| Clinical stage | 0.01 | ||
| IA | 136 (55.3) | 59 (72.8) | |
| IB | 43 (17.6) | 16 (19.8) | |
| IIA | 20 (8.2) | 3 (3.7) | |
| IIB | 12 (4.9) | 1 (1.2) | |
| III | 30 (12.2) | 2 (2.5) | |
| IV | 5 (2.0) | 0 (0.0) | |
| Preoperative treatment | 0.20 | ||
| No | 239 (97.2) | 81 (100.0) | |
| Yes | 7 (2.8) | 0 (0.0) | |
| Type of resection | 0.47 | ||
| Lobectomy or more | 184 (74.8) | 57 (70.4) | |
| Wedge resection or segmentectomy | 62 (25.2) | 24 (29.6) | |
| VATS or thoracotomy | <0.001 | ||
| Thoracotomy | 53 (21.5) | 4 (4.9) | |
| VATS | 193 (78.5) | 77 (95.1) | |
| Mediastinal lymphadenectomy | 198 (80.5) | 68 (84.0) | 0.62 |
| Operative time (min) | 210.00 [40.00, 580.00] | 185.00 [45.00, 310.00] | 0.004 |
| Operative time >240 min | 64 (26.0) | 11 (13.6) | 0.02 |
| Bleeding (mL) | 28.00 [0.00, 1,881.00] | 15.00 [0.00, 1,000.00] | 0.001 |
| Bleeding >200 mL | 30 (12.2) | 2 (2.5) | 0.009 |
| Postoperative morbidity (Clavien-Dindo classification ≥3) | 23 (9.3) | 6 (7.4) | 0.82 |
| Histological subtype | 0.46 | ||
| Adenocarcinoma | 185 (75.2) | 66 (81.5) | |
| Squamous cell carcinoma | 42 (17.1) | 11 (13.6) | |
| Adenosquamous cell carcinoma | 4 (1.6) | 1 (1.2) | |
| Large cell carcinoma | 3 (1.2) | 2 (2.5) | |
| Others | 12 (4.9) | 1 (1.2) | |
| Ly+ | 55 (22.4) | 7 (8.6) | 0.005 |
| V+ | 36 (14.6) | 8 (9.9) | 0.35 |
| pl+ | 79 (32.1) | 14 (17.3) | 0.01 |
| Pathological stage | 0.01 | ||
| IA | 113 (45.9) | 51 (63.0) | |
| IB | 42 (17.1) | 17 (21.0) | |
| IIA | 22 (8.9) | 6 (7.4) | |
| IIB | 16 (6.5) | 1 (1.2) | |
| III | 44 (17.9) | 5 (6.2) | |
| IV | 9 (3.7) | 1 (1.2) | |
| ≥ pStage II | 91 (37.0) | 13 (16.0) | <0.001 |
| R | 0.18 | ||
| R0 | 229 (93.1) | 80 (98.8) | |
| R1 | 13 (5.3) | 1 (1.2) | |
| R2 | 4 (1.6) | 0 (0.0) | |
| Postoperative therapy | 0.003 | ||
| Chemotherapy | 96 (39.0) | 17 (21.0) | |
| Chemoradiotherapy | 12 (4.9) | 3 (3.7) | |
| Radiotherapy | 7 (2.8) | 0 (0.0) | |
| None | 131 (53.3) | 61 (75.3) | |
| Follow-up period (months) | 92.50 [0.00, 164.00] | 81.00 [0.00, 119.00] | 0.25 |
Values are presented as median [minimum, maximum] or n (%). BMI, body mass index; PS, performance status; ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in one second; CT, computed tomography; VATS, video-assisted thoracic surgery.
Multivariable analysis demonstrated age ≥75 years [odds ratio 1.83, 95% confidence interval (CI) 1.01–3.32] and female sex (odds ratio 1.87, 95% CI: 1.06–3.3) were independent risk factors for dropout from follow-up (Figure 2).

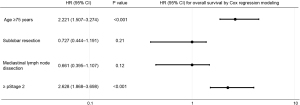
The 246 patients with follow-up over 10 years were divided into two groups, comprising 189 patients ≥75 years of age and 57 patients <75 years of age. In univariate analyses, significant differences were observed in age, American Society of Anesthesiologists physical status, smoking history, chronic obstructive pulmonary disease, hypertension, cardiovascular disease, cerebral infarction, number of oral medications, clinical stage, type of resection and mediastinal lymphadenectomy between groups (Table 2). Overall survival was significantly better in the group with age ≥75 years than in the group with age <75 years (Figure 3A). Disease-specific survival did not differ significantly between groups (5-year disease-specific survival rate: 71.9% vs. 73.4%, 10-year disease-specific survival: 66.0% vs. 61.2%, P=0.80) (Figure 3B). Recurrence after more than 5 years of follow-up was detected in 5 of 246 cases (2.0%). Using Cox proportional hazard regression, age ≥75 years (hazard ratio 2.221; 95% CI: 1.507–3.274; P<0.001) and stage ≥2 (hazard ratio 2.628; 95% CI: 1.868–3.698; P<0.001) were significantly associated with poorer overall survival (Figure 4).
Table 2
| Characteristics | Age | P value | |
|---|---|---|---|
| <75 years (n=189) | ≥75 years (n=57) | ||
| Sex | 0.22 | ||
| Male | 112 (59.3) | 28 (49.1) | |
| Female | 77 (40.7) | 29 (50.9) | |
| Age (years) | 64.00 [39.00, 74.00] | 79.00 [75.00, 90.00] | <0.001 |
| BMI (kg/m2) | 22.89 [14.74, 32.89] | 22.51 [16.37, 28.84] | 0.20 |
| PS | |||
| 0 | 169 (89.4) | 43 (75.4) | 0.01 |
| 1 | 19 (10.1) | 14 (24.6) | |
| 2 | 1 (0.5) | 0 (0.0) | |
| ASA classification | <0.001 | ||
| 1 | 28 (14.8) | 0 (0.0) | |
| 2 | 154 (81.5) | 45 (78.9) | |
| 3 | 7 (3.7) | 12 (21.1) | |
| Smoking | 0.03 | ||
| Never | 61 (32.3) | 27 (47.4) | |
| Ex-smoker | 77 (40.7) | 23 (40.4) | |
| Current smoker | 51 (27.0) | 7 (12.3) | |
| COPD | 26 (13.8) | 21 (36.8) | <0.001 |
| Hypertension | 67 (35.4) | 34 (59.6) | 0.002 |
| Dyslipidemia | 45 (23.8) | 16 (28.1) | 0.60 |
| Diabetes mellitus | 24 (12.7) | 2 (3.5) | 0.051 |
| Cardiovascular | 17 (9.0) | 17 (29.8) | <0.001 |
| Cerebral infarction | 4 (2.1) | 13 (22.8) | <0.001 |
| Dementia | 0 (0.0) | 2 (3.5) | 0.053 |
| Number of preoperative oral medications | 2.00 [0.00, 15.00] | 5.00 [0.00, 11.00] | <0.001 |
| Preoperative FEV1 (mL) | 2,325.00 [1,050.00, 4,050.00] | 1,785.00 [1,050.00, 3,180.00] | <0.001 |
| Tumor on CT | 0.050 | ||
| GGO (pure ground glass type) | 5 (2.6) | 6 (10.5) | |
| Mixed GGO (partially solid type) | 39 (20.6) | 9 (15.8) | |
| Solid tumor (solid type) | 145 (76.7) | 42 (73.7) | |
| Solid diameter (mm) | 22.00 [0.00, 120.00] | 26.00 [0.00, 100.00] | 0.30 |
| Tumor diameter (mm) | 24.00 [3.00, 120.00] | 29.00 [8.00, 100.00] | 0.04 |
| Clinical stage | 0.02 | ||
| IA | 106 (56.1) | 30 (52.6) | |
| IB | 31 (16.5) | 12 (21.1) | |
| IIA | 12 (6.4) | 8 (14.0) | |
| IIB | 7 (3.7) | 5 (8.8) | |
| III | 28 (14.9) | 2 (3.5) | |
| IV | 5 (2.7) | 0 (0.0) | |
| Preoperative treatment | >0.99 | ||
| No | 183 (96.8) | 56 (98.2) | |
| Yes | 6 (3.2) | 1 (1.8) | |
| Type of resection | <0.001 | ||
| Lobectomy or more | 152 (80.4) | 32 (56.1) | |
| Wedge resection or segmentectomy | 37 (19.6) | 25 (43.9) | |
| VATS or thoracotomy | 0.72 | ||
| Thoracotomy | 42 (22.2) | 11 (19.3) | |
| VATS | 147 (77.8) | 46 (80.7) | |
| Mediastinal lymphadenectomy | 166 (87.8) | 32 (56.1) | <0.001 |
| Operative time (min) | 210.00 [55.00, 580.00] | 195.00 [40.00, 440.00] | 0.07 |
| Bleeding (mL) | 25.00 [0.00, 1,881.00] | 36.00 [0.00, 850.00] | 0.74 |
| Postoperative morbidity (Clavien-Dindo classification ≥3) | 16 (8.5) | 7 (12.3) | 0.44 |
| Histological subtype | 0.61 | ||
| Adenocarcinoma | 143 (75.7) | 42 (73.7) | |
| Squamous cell carcinoma | 33 (17.5) | 9 (15.8) | |
| Adenosquamous cell carcinoma | 2 (1.1) | 2 (3.5) | |
| Large cell carcinoma | 2 (1.1) | 1 (1.8) | |
| Other | 9 (4.8) | 3 (5.3) | |
| Ly+ | 44 (23.3) | 11 (19.3) | 0.59 |
| V+ | 27 (14.3) | 9 (15.8) | 0.83 |
| pl+ | 64 (33.9) | 15 (26.3) | 0.33 |
| Pathological stage | 0.11 | ||
| IA | 87 (46.0) | 26 (45.6) | |
| IB | 29 (15.3) | 13 (22.8) | |
| IIA | 16 (8.5) | 6 (10.5) | |
| IIB | 11 (5.8) | 5 (8.8) | |
| III | 40 (21.2) | 4 (7.0) | |
| IV | 6 (3.2) | 3 (5.3) | |
| R | 0.02 | ||
| R0 | 180 (95.2) | 49 (86.0) | |
| R1 | 6 (3.2) | 7 (12.3) | |
| R2 | 3 (1.6) | 1 (1.8) | |
| Postoperative therapy | <0.001 | ||
| Yes | 104 (55.0) | 11 (19.3) | |
| None | 85 (45.0) | 46 (80.7) | |
| Recurrence | 0.053 | ||
| Distant | 50 (26.5) | 8 (14.0) | |
| Locoregional | 22 (11.6) | 12 (21.1) | |
| None | 117 (61.9) | 37 (64.9) | |
| Follow-up period (months) | 121.00 [1.00, 164.00] | 49.00 [0.00, 152.00] | <0.001 |
Values are presented as median [minimum, maximum] or n (%). BMI, body mass index; PS, performance status; ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in one second; CT, computed tomography; GGO, ground-glass opacity; VATS, video-assisted thoracic surgery.
Discussion
Our study showed that following up elderly individuals after resecting NSCLC in the lung is difficult. Moreover, disease-specific survival after lung resection of NSCLC did not differ significantly between young and old patients, despite the use of limited resection.
Many reports have investigated follow-up and prognosis after lung cancer resection. Recurrence of NSCLC after lung resection, maximum standardized uptake value >5, increasing pathologic stage, and preoperative radiation therapy have been reported to be independently associated with NSCLC recurrence after resection (9). No significant difference in survival was reported when comparing the approaches of thoracoscopic and open lobectomy (10). Our results are also similar to those of previous studies.
Taylor et al. reported that sublobar resection was independently associated with locoregional recurrence and lymphovascular invasion was associated with distant recurrence (9). On the other hand, prognosis after segmentectomy of NSCLC ≤2 cm in diameter does not show any significant difference from lobectomy (11). In NSCLC with a tumor size of 2 cm or less and pathologically confirmed node-negative disease in the hilar and mediastinal lymph nodes, sublobar resection was not inferior to lobectomy with respect to disease-free survival. Overall survival was similar with the two procedures (12). Although our study was small in size and segmentectomy cases were more common among elderly patients than among young patients in our study, disease-specific survival did not differ significantly between groups. Having said that, age ≥75 years and ≥ stage 2 were factors associated with poorer overall survival in our study. That is to say, elderly patients could not receive sufficient chemotherapy and most causes of death in elderly patients were attributable to other diseases. Our findings highlight the challenges in maintaining long-term follow-up in elderly NSCLC patients. Although older age and advanced stage were associated with poorer overall survival, disease-specific survival did not significantly differ by age, indicating that elderly patients may benefit from continuous follow-up and tailored management strategies. This study adds novel insights into the factors influencing follow-up adherence, which is crucial for optimizing long-term outcomes in NSCLC patients.
Maeda et al. reported patients who were free of recurrence at 5 years were 11% cases developed a subsequent recurrence (3). Sonoda et al. reported the possibility of ultra-late recurrence developing >10 years after resection of invasive NSCLC and developed in 2.5% cases (13). On the other hand, the late recurrence rate of our study was lower than these reports. It should also be noted, however, that late recurrence is difficult to strictly distinguish from second lung cancer. Although we conducted discussions with other professional oncologists and radiologists with consideration of risk of recurrence, clinical course, and imaging and made diagnoses with care, this may not have been sufficient for accurate differentiation. In the future, if genetic testing becomes commonplace, differentiation may become easy.
Several potential limitations to this study need to be considered. First, this was a retrospective study and had a selection bias toward patients who had undergone surgery. This was because no strict criteria exist for patients who had not undergone surgery. However, the real-world results obtained here are important. Second, our prognosis survey was strictly pursued however dropout cases of follow-up arose irrespective of the reason for drop-out. We therefore think that these findings should also be recognized as real-world data.
Conclusions
In patients with NSCLC after lung resection, age ≥75 years and female sex were risk factors for drop-out from follow-up >10 years. In addition, although age ≥75 years and with stage ≥2 disease were significantly associated with overall survival, patients ≥75 years of age have a high risk of death from other diseases. Sufficient consideration and informed consent for surgical indications are therefore necessary.
Acknowledgments
The authors would like to acknowledge all the staff involved in patient care in the Department of Thoracic Surgery at the National Hospital Organization, Hokkaido Cancer Center.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-909/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-909/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-909/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-909/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval for this study was granted by the ethics committee of Hokkaido Cancer Center (approval no. 03-26; date of approval: October 13, 2021); the requirement to obtain informed consent directly was waived for this retrospective study, and informed consent was obtained in the form of opt-out on the website of our institution.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Okada M, Nishio W, Sakamoto T, et al. Long-term survival and prognostic factors of five-year survivors with complete resection of non-small cell lung carcinoma. J Thorac Cardiovasc Surg 2003;126:558-62. [Crossref] [PubMed]
- Martini N, Rusch VW, Bains MS, et al. Factors influencing ten-year survival in resected stages I to IIIa non-small cell lung cancer. J Thorac Cardiovasc Surg 1999;117:32-6; discussion 37-8. [Crossref] [PubMed]
- Maeda R, Yoshida J, Hishida T, et al. Late recurrence of non-small cell lung cancer more than 5 years after complete resection: incidence and clinical implications in patient follow-up. Chest 2010;138:145-50. [Crossref] [PubMed]
- Bugge AS, Lund MB, Valberg M, et al. Cause-specific death after surgical resection for early-stage non-small-cell lung cancer. Eur J Cardiothorac Surg 2018;53:221-7. [Crossref] [PubMed]
- Martini N, Bains MS, Burt ME, et al. Incidence of local recurrence and second primary tumors in resected stage I lung cancer. J Thorac Cardiovasc Surg 1995;109:120-9. [Crossref] [PubMed]
- Morandi U, Stefani A, Golinelli M, et al. Results of surgical resection in patients over the age of 70 years with non small-cell lung cancer. Eur J Cardiothorac Surg 1997;11:432-9. [Crossref] [PubMed]
- Okamoto J, Kubokura H, Usuda J. Factors Determining the Choice of Surgical Procedure in Elderly Patients with Non-Small Cell Lung Cancer. Ann Thorac Cardiovasc Surg 2016;22:131-8. [Crossref] [PubMed]
- Dell'Amore A, Monteverde M, Martucci N, et al. Lobar and sub-lobar lung resection in octogenarians with early stage non-small cell lung cancer: factors affecting surgical outcomes and long-term results. Gen Thorac Cardiovasc Surg 2015;63:222-30. [Crossref] [PubMed]
- Taylor MD, Nagji AS, Bhamidipati CM, et al. Tumor recurrence after complete resection for non-small cell lung cancer. Ann Thorac Surg 2012;93:1813-20; discussion 1820-1. [Crossref] [PubMed]
- Nwogu CE, D'Cunha J, Pang H, et al. VATS lobectomy has better perioperative outcomes than open lobectomy: CALGB 31001, an ancillary analysis of CALGB 140202 (Alliance). Ann Thorac Surg 2015;99:399-405. [Crossref] [PubMed]
- Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022;399:1607-17. [Crossref] [PubMed]
- Altorki N, Wang X, Kozono D, et al. Lobar or Sublobar Resection for Peripheral Stage IA Non-Small-Cell Lung Cancer. N Engl J Med 2023;388:489-98. [Crossref] [PubMed]
- Sonoda D, Matsuura Y, Ichinose J, et al. Ultra-late recurrence of non-small cell lung cancer over 10 years after curative resection. Cancer Manag Res 2019;11:6765-74. [Crossref] [PubMed]




