
Impact of multimorbidity on risk stratification and prognosis in elderly patients after acute myocardial infarction
Highlight box
Key findings
• Comorbidity in elderly acute myocardial infarction (AMI) patients allows for risk stratification and prognosis prediction.
What is known and what is new?
• There is a lack of evidence of the extent to which a multimorbidity condition impacts on the prognosis of elderly patients with AMI.
• This manuscript contributes to the investigation of the clinical characteristics and the prognosis in elderly AMI patients after emergency percutaneous coronary intervention with regard to number of comorbidities.
What is the implication, and what should change now?
• This retrospective observational study suggested that the burden of comorbidity allows for the identification of risk stratification and prognosis. The development of an evaluation of comorbidity for elderly AMI patients could help clinicians to determine the feasibility and complexity of comorbidity, provide better management options, and improve prognoses.
Introduction
Cardiovascular disease (CVD) has rapidly and substantially increased worldwide, and it remains a leading cause of morbidity and mortality, even with immediate invasive revascularization (1-4). Elderly patients with acute myocardial infarction (AMI) more often have severe complications, and they have higher in-hospital mortality rates despite early reperfusion and improvements in pharmacological therapy (5,6). A growing body of work corroborates the compounding effects of comorbidity on health outcomes attributable to individual diseases in patients who are at greater risk of poor outcomes (7,8).
Multimorbidity, defined as two or more co-occurring chronic diseases, has increased substantially in aged patients with a decline of cardiovascular structure and function, and it is highly disabling and costly (9-11). It is common that multiple comorbidities coexist in elderly patients. It is likely that clinical prognosis and complications will deteriorate with the increase in number of concomitant diseases in patients with AMI (12). As the number of elderly patients with multimorbidity continues to rise, physicians need to make effective management decisions and be aware of the clinical presentations, altered pharmacokinetics, and altered cognitive and functional status. The optimal strategies would depend on risk stratification of multimorbidity at admission in patients who experience AMI and would contribute to improve the prognosis of elderly AMI patients with multi-comorbidity. However, it is unclear and there is a lack of evidence of the extent to which multimorbidity conditions impact on the prognosis of elderly patients with AMI after percutaneous coronary intervention (PCI). Therefore, the aim of this study was to investigate the clinical characteristics and the short- and long-term prognosis in this population of elderly AMI patients after emergency PCI with regard to number of comorbidities. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-772/rc).
Methods
Study population
This was a retrospective observational study of elderly patients (older than 65 years) with a diagnosis of first AMI who were admitted to the cardiac intensive care unit between January 2014 and September 2019. The 498 consecutive elderly patients with AMI who underwent emergency PCI were enrolled and included in the absence of selection bias in current study. Eight patients were excluded because of incomplete data, 4 patients were excluded due to malignant tumor, 3 patients were excluded due to severe cardiac valve disease, and patients were excluded due to missed follow-up. The remaining 479 AMI patients were enrolled in the study. There were 351 males (73.28%) and 128 females (26.72%). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of the First Affiliated Hospital of Soochow University (No. 2024399). All enrolled patients provided written consent and the data were used in accordance with the directives of the ethics committee.
Specific comorbidities are closely related to the prognosis in patients with AMI. The enrolled patients were divided into three groups according to the burden of prior comorbidities: group A (with zero or one comorbidity, 220 cases, 45.93%, used as the control group), group B (with two comorbidities, 157 cases, 32.78%), and group C (with three or more comorbidities, 102 cases, 21.29%). We further examined the frequencies of possible comorbidity in our study population. The prevalence of comorbid conditions in all enrolled participants among three groups is presented in Figure 1. Hypertension, chronic obstructive pulmonary disease (COPD), and diabetes were the most common comorbidities combination in the three groups of patients. Only a small fraction of patients had thyroid dysfunction, chronic kidney disease, hyperlipidemia, heart failure, anemia, Alzheimer’s disease, and depression. In group A, 55.5% of patients had hypertension, 17.7% of patients had COPD, 6.4% of patients had diabetes, and 10.5% of patients did not have any comorbidity. In group B, 31.8% of patients had hypertension and diabetes, 26.8% of patients had hypertension and COPD, 8.3% of patients had hypertension and cerebrovascular disease, and other disease combinations. Meanwhile, 61.8% of patients had hypertension, diabetes, and another disease, 20.6% of patients had hypertension, COPD, and another disease, 4.9% of patients had hypertension, atrial fibrillation, and another disease, and other combinations in group C. All the enrolled participants were followed up for one year. The in-hospital complications were defined as the incidence of death, malignant ventricular tachycardia/fibrillation (VT/VF), ventricular aneurysm, acute attack of paroxysmal atrial fibrillation/flutter, cardiac rupture, high-grade atrioventricular block, and attack of acute heart failure.

Exposure definitions
The time from attack to reperfusion represents the time difference from symptom onset to the insertion of the catheter through the lesion. The major adverse cardiovascular events (MACEs) were defined as the composite of all-cause death, recurrent non-fatal myocardial infarction, non-fatal ischemic stroke, acute heart failure, and late revascularization (>90 days) in the current study.
Data collection
All patients’ demographic data, clinical characteristics, laboratory findings, echocardiographic data, angiography data, and medical treatments were collected and analyzed. The clinical characteristics included age, gender, prior hypertension, prior diabetes mellitus, alcohol consumption, and smoking. The baseline characteristics were age, gender, prior smoking, and length of hospital stay, heart rate, systolic blood pressure (SBP), and diastolic blood pressure (DBP). Laboratory biomarkers, including white blood cell (WBC) count, serum uric acid, serum creatinine (Scr), glucose, total bilirubin, high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), total cholesterol (TC), and triglyceride (TG), were measured at admission. Peak MB isoenzyme of creatine kinase (CK-MB) was measured 24 hours after the AMI attack. Cardiac structure and function were measured by M-mode and two-dimensional Doppler echocardiography at admission, including left atrium diameter (LAd), left ventricular end systolic diameter (LVESd), left ventricular end diastolic diameter (LVEDd), and left ventricular ejection fraction (LVEF). The relative number of diseased vessels, number of infarction-related arteries (IRAs), and number of culprit vessels located in the left main (LM) artery, left anterior descending artery (LAD), left circumflex artery (LCX), and right coronary artery (RCA) were analyzed. Coronary blood flow was assessed by thrombolysis in myocardial infarction (TIMI) coronary grade flow 0–3 after cardiac catheter angiography (13). The results of TIMI coronary grade flow were independently analyzed by two trained physicians who were blinded to the clinical data. A third physician was engaged if there was a difference in assessment between the two physicians. Each patient underwent emergency PCI therapy and was given appropriate prescriptions. The associated coronary angiographic changes, other medical assistance {intra-aortic balloon pump (IABP), thrombus aspiration catheter, intravenous injection of glycoprotein IIb/IIIa inhibitors, and oral administration of medication [aspirin combined clopidogrel, aspirin combined ticagrelor, proton pump inhibitors (PPIs), renin-angiotensin system inhibitors, beta-receptor blockers, and diuretics]} were analyzed. The prevalence of in-hospital complications in the older patients with AMI was analyzed. The MACE rates of patients at the one-year follow-up were obtained by reviewing medical records and through telephone interviews based on the number of multimorbidity. The prognostic value of comorbid conditions in predicting one-year MACE and all-cause death was assessed by receiver operating characteristic (ROC) curve analysis.
Statistical analyses
All data were analyzed using the SPSS software package (Version 25.0; IBM Corp., Armonk, NY, USA). Continuous variables were presented as mean ± standard deviation, and they were compared using one-way analysis of variance (ANOVA) (data with normal distribution), or presented as median (quartile range) values and were compared by Kruskal-Wallis H test (data with non-normal distribution). Categorical variables were expressed by numbers (percentage) and then they were compared by the chi-squared or Fisher’s exact test. The one-year rates of cumulative MACE were evaluated by the Kaplan-Meier method. The prognostic value of comorbid condition in predicting one-year MACE and all-cause death was assessed by ROC curve analysis. A P<0.05 (two-sided) was considered statistically significant.
Results
Clinical characteristics, laboratory examination, and echocardiographic findings in the older patients with AMI
The clinical characteristics, laboratory data, and echocardiographic measurements of the patients at admission are presented in Table 1. The AMI patients who had two or more comorbidities in groups B and C were significantly older, had higher heart rates, higher levels of serum uric acid, Scr, and glucose than the those in the control group, whereas the proportion of gender and smoking, length of hospital stay, SBP and DBP values, level of WBC, peak CK-MB, total bilirubin, TC, LDL-C, and TG did not reach statistical significance. Moreover, there was a significantly higher level of glucose in the older AMI patients with three or more comorbidities than in those with two comorbidities.
Table 1
| Variables | Group A (n=220) | Group B (n=157) | Group C (n=102) | P value |
|---|---|---|---|---|
| Age, years | 71 [68, 77] | 74 [70, 79]* | 75 [70, 80]* | 0.001 |
| Sex | ||||
| Male | 166 (75.5) | 116 (73.9) | 69 (67.6) | 0.33 |
| Female | 54 (24.5) | 41 (26.1) | 33 (32.4) | 0.33 |
| Smoking | 107 (48.6) | 64 (40.8) | 42 (41.2) | 0.24 |
| Length of hospital stay, days | 9 [6, 11] | 9 [7, 13] | 9 [6, 13] | 0.72 |
| STEMI | 197 (89.5) | 123 (78.3)* | 86 (84.3) | 0.01 |
| NSTEMI | 23 (10.5) | 34 (21.7)* | 16 (15.7) | 0.01 |
| Heart rate, bpm | 77±14 | 82±18* | 86±19* | <0.001 |
| SBP, mmHg | 124±24 | 124±24 | 124±23 | 0.87 |
| DBP, mmHg | 75±13 | 75 [67, 85] | 75±14 | 0.64 |
| Laboratory findings | ||||
| White blood cell counts (×1012/L) | 9.57 [7.54, 12.05] | 9.52 [7.58, 12.67] | 10.49 [8.55, 12.54] | 0.13 |
| Peak CK-MB (μg/L) | 167.6 [68.4, 300.0] | 136.1 [62.2, 267.7] | 123.1 [37.7, 265.6] | 0.056 |
| Serum uric acid (μmol/L) | 343±97 | 383 [323, 471]* | 382 [294, 507]* | <0.001 |
| Serum creatinine (mg/dL) | 0.84 [0.72, 0.97] | 0.93 [0.75, 1.14]* | 1.01 [0.81, 1.42]* | <0.001 |
| Glucose (mmol/L) | 5.72 [4.97, 6.64] | 6.69 [5.44, 8.05]* | 7.73 [5.95, 10.49]*# | <0.001 |
| Total bilirubin (μmol/L) | 16.4 [12.8, 21.7] | 17.7 [13.1, 23.3] | 16.5 [11.9, 23.2] | 0.48 |
| LDL-C (μmol/L) | 2.87 [2.28, 3.45] | 2.76±0.90 | 2.70 [2.10, 3.30] | 0.25 |
| Total cholesterol (mmol/L) | 4.57 [3.88, 5.30] | 4.45±1.01 | 4.39 [3.59, 5.12] | 0.19 |
| Triglyceride (mmol/L) | 1.11 [0.82, 1.52] | 1.22 [0.87, 1.71] | 1.27 [0.89, 1.74] | 0.14 |
| Echocardiogram findings at admission | ||||
| LAd (mm) | 39 [36, 42] | 40±5* | 41 [39, 45]* | <0.001 |
| LVESd (mm) | 38 [33, 41] | 39±6 | 38 [36, 42] | 0.08 |
| LVEDd (mm) | 50 [47, 53] | 50 [47, 54] | 50 [48, 53] | 0.24 |
| LVEF | 0.47 [0.42, 0.54] | 0.45 [0.40, 0.53] | 0.45±0.09* | 0.005 |
Data are presented as mean ± standard deviation, median [quartile range] or n (%). *, P<0.05 (group B or group C vs. group A); #, P<0.05 (group C vs. group B). Group A: with zero or one comorbidity, used as the control group; group B: with two comorbidities; group C: with three or more comorbidities. STEMI, ST segment elevation myocardial infarction; NSTEM, non-ST segment elevation myocardial infarction; SBP, systolic blood pressure; DBP, diastolic blood pressure; CK-MB, MB isoenzyme of creatine kinase; LDL-C, low-density lipoprotein cholesterol; LAd, left atrial diameter; LVESd, left ventricular end-systolic diameter; LVEDd, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction.
With respect to echocardiographic data, elderly AMI patients who were complicated with two or more comorbidities presented with a more enlarged LAd than the control cases in group A, and there was lower LVEF in elderly AMI patients with three or more comorbidities than patients in group A. However, there was no significant difference in LVESd and LVEDd among the three groups. These data indicated that the elderly AMI patients with a greater burden of comorbidity had more serious clinical presentations.
Comparison of in-hospital angiographic characteristics and other medical procedures
Further comparisons of the angiographic findings and medical procedures were conducted among the three groups (Table 2). A more prolonged time of attack to reperfusion was found among the patients with three or more comorbidities than among those in the other two groups. A significantly higher number of patients with two or more comorbidities had multivessel disease, whereas a significantly lower number of these patients had single-vessel disease than those with zero or one comorbidity. In addition, there was a notable increase in the proportion of IRA located in the LM in patients with two or more comorbidities as compared with those with zero or one comorbidity. In addition to the above parameters, there was no difference in the relative number of two-vessel disease, the relative number of single, two, and multiple IRA, and the relative number of culprit vessel located in the LAD, LCX, and RCA. In addition, we found significant differences among the three groups regarding the relative number patients of TIMI flow grades after PCI. The patients who had two or more comorbidities were more likely to present with TIMI flow grade 0–1 or 2 after PCI, but less likely to present with TIMI flow 3 after PCI, compared with the patients in group A. These results suggested that patients with multiple comorbidities might have had serious changes to their coronary arteries.
Table 2
| Variables | Group A (n=220) | Group B (n=157) | Group C (n=102) | P |
|---|---|---|---|---|
| Time from attack to reperfusion (hours), median (quartile range) | 6.0 (4.0, 9.5) | 7.0 (4.8, 11.0) | 8.0 (5.0, 12.0)* | 0.002 |
| Number of diseased vessels, n (%) | 0.001 | |||
| Single | 105 (47.7) | 53 (33.8)* | 31 (30.4)* | 0.003 |
| Two | 78 (35.5) | 56 (35.7) | 35 (34.3) | 0.97 |
| Multiple | 37 (16.8) | 48 (30.6)* | 36 (35.3)* | <0.001 |
| Number of infarction-related arteries, n (%) | 0.61 | |||
| Single | 197 (89.5) | 137 (87.3) | 87 (85.3) | 0.53 |
| Two | 22 (10.0) | 18 (11.5) | 13 (12.7) | 0.75 |
| Multiple | 1 (0.5) | 2 (1.3) | 2 (2.0) | 0.30 |
| Location of culprit vessel, n (%) | ||||
| LM | 2 (0.9) | 10 (6.4)* | 8 (7.8)* | 0.001 |
| LAD | 135 (61.4) | 88 (56.1) | 62 (60.8) | 0.56 |
| LCX | 35 (15.9) | 19 (12.1) | 14 (13.7) | 0.57 |
| RCA | 69 (31.4) | 60 (38.2) | 31 (30.4) | 0.29 |
| TIMI flow grade after PCI, n (%) | ||||
| 0–1 | 0 (0.0) | 5 (3.2)* | 8 (7.8)* | <0.001 |
| 2 | 18 (8.2) | 25 (15.9) | 19 (18.6)* | 0.01 |
| 3 | 202 (91.8) | 127 (80.9)* | 75 (73.5)* | <0.001 |
| Medical treatment, n (%) | ||||
| Intra-aortic balloon pump | 4 (1.8) | 11 (7.1)* | 4 (4.0) | 0.04 |
| Thrombus aspiration catheter | 7 (3.2) | 8 (5.1) | 8 (7.8) | 0.17 |
| Aspirin + clopidogrel | 93 (42.3) | 64 (40.8) | 53 (52.0) | 0.17 |
| Aspirin + ticagrelor | 127 (57.7) | 93 (59.2) | 49 (48.0) | 0.17 |
| PPI | 199 (90.5) | 142 (90.4) | 96 (94.1) | 0.51 |
| Renin-angiotensin system inhibitors | 141 (64.1) | 108 (68.8) | 70 (68.6) | 0.56 |
| Beta-blockers | 182 (82.7) | 111 (70.7)* | 79 (77.5) | 0.02 |
| Diuretic | 111 (50.5) | 99 (63.1)* | 71 (69.6)* | 0.002 |
| Statin | 210 (95.5) | 143 (91.1) | 90 (88.2) | 0.053 |
*, P<0.05 (group B or group C vs. group A); #, P<0.05 (group C vs. group B). Group A: with zero or one comorbidity, used as the control group; group B: with two comorbidities; group C: with three or more comorbidities. Diseased vessels was defined as ≥50% diameter stenosis in major epicardial branches (LAD, LCX, RCA). LM, left main; LAD, left anterior descending artery; LCX, left circumflex artery; RCA, right coronary artery; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction; PPI, proton pump inhibitor.
With respect to medical treatments, the patients in group B were more likely to undergo IABP measurements than the patients in the other groups. The patients received diuretics more frequently in groups B and C and beta-blockers less frequently in group B than those in control group A. However, no significant difference was observed with respect to the utilization rate of thrombus aspiration catheter, and oral usage of antiplatelet, PPI, and RAS among the three groups.
Comparison of in-hospital adverse events and one-year MACE
The in-hospital cardiovascular complications in the older patients after AMI and one-year MACE are summarized in Table 3. We found that the incidence of in-hospital death, paroxysmal atrial fibrillation/flutter, cardiac rupture, and acute heart failure was significantly higher in patients with two or more comorbidities than in those with zero or one comorbidity. Similarly, the incidence of cardiac rupture was notably higher in patients with three or comorbidities than the control cases in group A. Furthermore, the incidence of in-hospital death was remarkably higher in patients with three or comorbidities than patients with two comorbidities. However, the proportion of malignant VT/VF, ventricular aneurysm, and high-grade atrioventricular block showed no significant difference across the three groups. These data suggested that patients with a greater burden of chronic comorbidity had more severe in-hospital complications, and this comports with our previous data analyses.
Table 3
| Variables | Group A (n=220) | Group B (n=157) | Group C (n=102) | P value |
|---|---|---|---|---|
| In-hospital complications after myocardial infraction, n (%) | ||||
| Death in hospital | 5 (2.3) | 13 (8.3)* | 30 (29.4)*# | <0.001 |
| Malignant VT/VF | 11 (5.0) | 11 (7.0) | 12 (11.8) | 0.09 |
| Ventricular aneurysm | 22 (10.0) | 20 (12.7) | 20 (19.6) | 0.057 |
| Paroxysmal atrial fibrillation/flutter | 14 (6.4) | 22 (14.0)* | 25 (24.5)* | <0.001 |
| Cardiac rupture | 2 (0.9) | 5 (3.2) | 6 (5.9)* | 0.03 |
| High-grade atrioventricular block | 11 (5.0) | 5 (3.2) | 9 (8.8) | 0.13 |
| Acute heart failure | 9 (4.1) | 24 (15.3)* | 23 (22.5)* | <0.001 |
| MACE at one-year, n (%) | ||||
| MACE | 42 (19.1) | 78 (49.7)* | 75 (73.5)*# | <0.001 |
| All-cause death | 14 (6.4) | 26 (16.7)* | 44 (43.1)*# | <0.001 |
| Acute heart failure | 21 (9.5) | 36 (22.9)* | 23 (22.5)* | 0.001 |
| non-fatal ischemic stroke | 0 (0.0) | 2 (1.3) | 6 (5.9)* | <0.001 |
| Recurrent non-fatal MI | 5 (2.3) | 6 (3.8) | 5 (4.9) | 0.41 |
| Late revascularization | 8 (3.6) | 17 (10.8)* | 8 (7.9) | 0.02 |
*, P<0.05 (group B or group C vs. group A); #, P<0.05 (group C vs. group B). Group A: with zero or one comorbidity, used as the control group; group B: with two comorbidities; group C: with three or more comorbidities. VT, ventricular tachycardia; VF, ventricular fibrillation; MACE, major adverse cardiovascular event; MI, myocardial infarction.
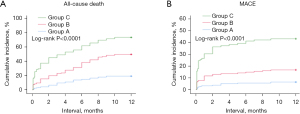
We found that the incidence of MACE, all-cause death, and attack of acute heart failure were significantly higher in groups B and C than in the control cases in group A, and that there was a higher probability of MACE and all-cause death in group C than the patients in group B. In addition, we found a higher probability of non-fatal ischemic stroke in patients with three or more comorbidities than in the cases in group A, and there was a significant difference in the proportion of late revascularization in patients with two comorbidities versus those with zero or one comorbidity. However, there was no difference in the incidence of recurrent non-fatal myocardial infarction (MI) across the three groups. The cumulative rates of all-cause death and one-year incidence of MACE were remarkably higher in patients with three or more mortalities, compared to the patients in the other two groups, and they were also significantly higher in patients with two comorbidities compared to patients with zero or one comorbidity (log-rank P<0.0001, Figure 2). After stratifying the patients by the number of comorbidities, we found that the number of comorbidities provided modest prognostic value for one-year MACE [area under the curve (AUC) =0.740] and all-cause death (AUC =0.742) rates assessed by ROC curve analysis (Figure 3). These data suggested that the greater burden of comorbidities in the older patients with AMI, the worse prognosis.

Discussion
Patients with an increased burden of co-occurring chronic diseases are at increased risk of poor outcomes (9,11). Information is limited concerning the association of comorbidity with prognosis of elderly patients with AMI after stratifying by multimorbid conditions. This study was a cohort study of 479 elderly patients with AMI. By analyzing the clinical characteristics, postoperative medication, and in-hospital complications of elderly AMI patients with multiple comorbidities, we found that patients with two or more comorbidities coexisting had more serious clinical conditions, required more medical treatments, presented with worse cardiac function and renal function, had more serious coronary artery lesions, had a higher incidence of in-hospital complications, and had poorer prognosis at one-year, compared with patients with zero or one comorbidity.
Older people typically have more comorbidities and lower organ functional status. A number of studies have shown how the individual comorbidities are related to poor outcomes in patients who developed AMI (7,8,14,15). The effect of multimorbidity on individual patients would vary with the combination and severity of comorbidities (16). For each comorbidity condition, the mortality rates of the AMI patients who experienced heart failure, renal failure or cerebrovascular disease were 63.5%, 57.2%, and 50.7%, respectively, after 8.4 years of follow-up (17), indicating a poor prognosis of AMI patients. Compared with one coexisting disease, the accumulation of multimorbid conditions has more adverse effects on the short- and long-term outcomes of elderly patients who develop from acute coronary syndrome (15). However, the association of outcomes to different levels of burden from comorbidity as well as treatments and clinical characteristics, is unclear. In this study, we evaluated the clinical manifestation and prognosis of elderly patients with different levels of burden from comorbidities.
With the aging of the population, some older individuals affected by coronary artery disease bear a greater burden from additional comorbidities (14,18). Elderly patients with comorbidity have other particular features that require attention, such as nutritional deficiency, progression of frailty, drug safety, intervention of combined diseases, and psychological status. These are closely related to the development and outcome of comorbidities, and they often require individualized therapy. Older patients with multimorbidity might be prescribed several drugs, each of which is recommended by a disease-specific guideline, but the overall drug burden is difficult for patients to manage, and it can be harmful. In the current study, we examined the correlation between medication and multiple comorbidities, and we evaluated whether the presence of multiple concurrent chronic diseases influenced medical treatment. In our study, the clinical diagnosis and treatment of elderly patients with multimorbidity coexistence were found to be complex, which increases the consumption of medical resources. Furthermore, the clinical manifestation, drug dosage, drug tolerance, and post-treatment response of elderly patients complicated with AMI varied with different types and different burden of comorbidities. The treatments of patients with multiple comorbidities should evaluate the risks and benefits of clinical decision-making and the feasibility and complexity of the treatment scheme. For example, AMI patients with chronic kidney disease should carefully consider angiotensin-converting enzyme inhibitor (ACEI) or angiotensin II receptor blocker (ARB) drug use to delay renal dysfunction. AMI patients with atrial fibrillation need to assess the risk of thrombosis and bleeding and determine whether antiplatelet drugs combined with anticoagulants can be used (19,20). Thus, elderly AMI patients with a different burden of comorbidity might receive different medical drugs and treatment with invasive devices.
Previous studies have found that TIMI flow grade is significantly associated with poor clinical prognosis (21,22). Similarly, we found that patients with two or more comorbidities presenting with more serious TIMI flow grade after PCI had poorer clinical outcomes compared to those with zero or one comorbidity in the study. Several systemic and local factors could impact TIMI flow, such as C-reactive protein, endothelin-1, thromboxane A2, WBC, glucose, adenosis, composition of the culprit plaques, history of diabetes mellitus, and long tubular lesion (23). Moreover, poor prognosis was significantly increased with the number of comorbidities, as shown in the investigation on the clinical characteristics and prognosis of elderly patients with cardiac failure (24). Given the strong relationship between comorbidity and prognosis, we observed that an increased incidence of in-hospital complications and one-year clinical MACE were likely related to the increasing number of comorbidities in older patients hospitalized with AMI after PCI according to the current study by evaluating the association of multimorbidity conditions and in-hospital and post-hospital adverse events, and this is consistent with previous results (5,24).
In elderly patients with AMI, the number of comorbidities is closely related to prognosis. Therefore, early stratification of co-occurring chronic disease contributes to early prediction short- and long-term mortality in elderly AMI patients. It is acceptable to use the burden of comorbidity to predict an unfavorable prognosis. With this information, physicians can make better choices about early evaluation, nursing, balancing patients’ circumstances, and avoiding adverse events, and patients might benefit from early invasive management and more aggressive use of hemodynamic supports in older patients after AMI.
Some limitations inherent to the study design should be acknowledged. The study did not further evaluate the impact of the patterns, duration, and management of comorbidities on the prognosis. Although a comprehensive group of variables was used in this study, not all chronic comorbidities were included for risk stratification and prognosis assessments.
Conclusions
Chronic diseases may lead clinicians to provide unnecessary or potentially harmful care to older adults with multimorbidity. This study retrospectively analyzed the coexistence of multiple diseases in elderly patients with AMI and compared the clinical characteristics, clinical medication, results of coronary angiography, and in-hospital and one-year outcomes. It was found that a higher burden of diseases was associated with a more serious clinical condition, higher in-hospital mortality, and worse long-term prognosis. These findings highlight the importance of comorbidity in elderly patients presenting with AMI and it suggested that clinicians should focus on establishing effective health management including early assessments, early supports, and individualized treatments for these patients. The knowledge of comorbidity allows for the identification of risk stratification, adverse events, and prognosis, and this may help clinicians to determine the feasibility and complexity of treatments, and improve the short- and long-term prognoses of elderly AMI patients with multiple coexisting diseases.
Acknowledgments
Funding: This study was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-772/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-772/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-772/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-772/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li R, Huddleston S. Development of Comorbidity Index for in-hospital mortality for patients who underwent coronary artery revascularization. J Cardiovasc Surg (Torino) 2023;64:678-85. [Crossref] [PubMed]
- Global Burden of Cardiovascular Diseases Collaboration. The Burden of Cardiovascular Diseases Among US States, 1990-2016. JAMA Cardiol 2018;3:375-89. [Crossref] [PubMed]
- Sanchis J, Soler M, Núñez J, et al. Comorbidity assessment for mortality risk stratification in elderly patients with acute coronary syndrome. Eur J Intern Med 2019;62:48-53. [Crossref] [PubMed]
- Townsend N, Wilson L, Bhatnagar P, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J 2016;37:3232-45. [Crossref] [PubMed]
- Roe MT, Messenger JC, Weintraub WS, et al. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol 2010;56:254-63. [Crossref] [PubMed]
- Nishihira K, Kuriyama N, Kadooka K, et al. Outcomes of Elderly Patients With Acute Myocardial Infarction and Heart Failure Who Undergo Percutaneous Coronary Intervention. Circ Rep 2022;4:474-81. [Crossref] [PubMed]
- Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition--multimorbidity. JAMA 2012;307:2493-4. [Crossref] [PubMed]
- Bobo WV, Yawn BP, St Sauver JL, et al. Prevalence of Combined Somatic and Mental Health Multimorbidity: Patterns by Age, Sex, and Race/Ethnicity. J Gerontol A Biol Sci Med Sci 2016;71:1483-91. [Crossref] [PubMed]
- Salive ME. Multimorbidity in older adults. Epidemiol Rev 2013;35:75-83. [Crossref] [PubMed]
- Goodman RA, Ling SM, Briss PA, et al. Multimorbidity Patterns in the United States: Implications for Research and Clinical Practice. J Gerontol A Biol Sci Med Sci 2016;71:215-20. [Crossref] [PubMed]
- Marengoni A, von Strauss E, Rizzuto D, et al. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med 2009;265:288-95. [Crossref] [PubMed]
- Hudzik B, Korzonek-Szlacheta I, Szkodziński J, et al. Prognostic impact of multimorbidity in patients with type 2 diabetes and ST-elevation myocardial infarction. Oncotarget 2017;8:104467-77. [Crossref] [PubMed]
- Ganz W. The thrombolysis in myocardial infarction (TIMI) trial. N Engl J Med 1985;313:1018. [Crossref] [PubMed]
- Sachdev M, Sun JL, Tsiatis AA, et al. The prognostic importance of comorbidity for mortality in patients with stable coronary artery disease. J Am Coll Cardiol 2004;43:576-82. [Crossref] [PubMed]
- Breen K, Finnegan L, Vuckovic K, et al. Multimorbidity in Patients With Acute Coronary Syndrome Is Associated With Greater Mortality, Higher Readmission Rates, and Increased Length of Stay: A Systematic Review. J Cardiovasc Nurs 2020;35:E99-E110. [Crossref] [PubMed]
- Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43. [Crossref] [PubMed]
- Hall M, Dondo TB, Yan AT, et al. Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: Latent class analysis of a nationwide population-based cohort. PLoS Med 2018;15:e1002501. [Crossref] [PubMed]
- Lin CC, Lee PY, Chen KC, et al. Clinical, Demographic, and Biochemical Characteristics of Patients with Acute ST-Segment Elevation Myocardial Infarction: An Analysis of Acute Coronary Syndrome Registry Data of a Single Medical Center from 2005 to 2016. Acta Cardiol Sin 2020;36:1-7. [Crossref] [PubMed]
- Cannon CP, Gropper S, Bhatt DL, et al. Design and Rationale of the RE-DUAL PCI Trial: A Prospective, Randomized, Phase 3b Study Comparing the Safety and Efficacy of Dual Antithrombotic Therapy With Dabigatran Etexilate Versus Warfarin Triple Therapy in Patients With Nonvalvular Atrial Fibrillation Who Have Undergone Percutaneous Coronary Intervention With Stenting. Clin Cardiol 2016;39:555-64. [Crossref] [PubMed]
- Cannon CP, Lip GYH, Oldgren J. Dual Antithrombotic Therapy with Dabigatran after PCI in Atrial Fibrillation. N Engl J Med 2018;378:485-6. [Crossref] [PubMed]
- De Luca G, Ernst N, Zijlstra F, et al. Preprocedural TIMI flow and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol 2004;43:1363-7. [Crossref] [PubMed]
- García-García C, Oliveras T, Serra J, et al. Trends in Short- and Long-Term ST-Segment-Elevation Myocardial Infarction Prognosis Over 3 Decades: A Mediterranean Population-Based ST-Segment-Elevation Myocardial Infarction Registry. J Am Heart Assoc 2020;9:e017159. [Crossref] [PubMed]
- Bahrehmand M, Sadeghi E, Shafiee A, et al. Predictors of delayed and no-reflow as recognized with Thrombolysis in Myocardial Infarction [TIMI] flow grade following Primary Percutaneous Coronary Angioplasty. J Med Life 2015;8:59-65.
- Rashid M, Kwok CS, Gale CP, et al. Impact of co-morbid burden on mortality in patients with coronary heart disease, heart failure, and cerebrovascular accident: a systematic review and meta-analysis. Eur Heart J Qual Care Clin Outcomes 2017;3:20-36. [Crossref] [PubMed]
(English Language Editor: J. Jones)


