A case of anterior mediastinitis and bilateral multiple lung abscesses occurring after trans-subxiphoid video-assisted thoracoscopic extended thymectomy for thymoma with myasthenia gravis
Introduction
With regard to the video-assisted thoracoscopic surgery (VATS) for patients with MG or anterior mediastinal masses, previous reports indicated that TsVATET can provide a better surgical exposure than the unilateral thoracoscopic approach. In addition, TsVATET is comparable to median sternotomy in terms of the anterior mediastinal adipose tissues dissection. However, to our knowledge, the postoperative complications for the subxiphoid approach have hardly been reported since Hsu et al. (1) first introduced this method for extended thymectomy in 2002. Herein, we present a patient who received TsVATET suffered from postoperative subxiphoid wound infection, secondarily developing anterior mediastinitis, bilateral pneumonia and multiple lung abscesses.
Case presentation
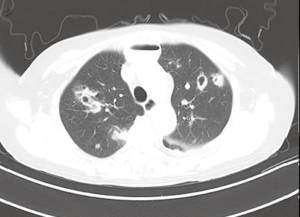
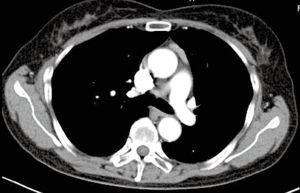
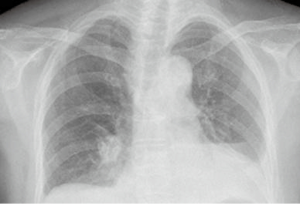
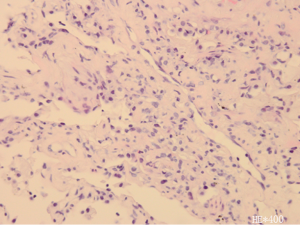
A 68-year-old female patient of Han nationality was diagnosed with thymoma and MG 5 months ago (Figure 1), with the presentation of ptosis, diplopia, and difficulties in mastication and swallowing. She had no other comorbidities and remained asymptomatic on mestinon, tacrolimus and prednisone therapy. Then she received TsVATET at our department. The surgical procedure is similar to the technique performed by Wu et al. (2). Under general anesthesia with bilateral lung ventilations, a 3.0 cm longitudinal incision was made below the xiphoid process as the observation hole, and additional two 0.5 cm operation holes were created at the bilateral midclavicular line in the seventh intercostal space. The bilateral mediastinal pleura were routinely opened and CO2 gas was injected at 8 mmHg through the subxiphoid port to widen the operation space. Then the whole thymus and anterior mediastinal adipose tissues were excised en bloc. Haemostasis is checked, followed by insertion of a chest tube through the camera port, which was removed on the postoperative day 3. The operation was performed smoothly and the patient had an uneventful recovery for the duration of hospitalization. A repeated chest radiograph after 3 days of surgery showed normal postoperative appearance (Figure 2). So she was discharged home on the next day. However, 7 days after the surgery, the patient was readmitted to our hospital presenting with progressive cough, stethalgia and fever. Physical examination revealed the subxiphoid wound suppuration. CT scans of the chest showed anterior mediastinal oedema, and infiltrative masses involved bilateral lung (Figure 3). On admission, the original subxiphoid wound was re-opened, and the necrotic tissues were removed. Mediastinal sample bacteriology cultures revealed staphylococcus aureus was responsible for the infection. Anti-infection treatment combined with anterior mediastinum irrigation and drainage had been administered to eliminate staphylococcus aureus. Then the patient felt well but non-productive cough. And the chest CT scans were suggestive of multiple pulmonary abscesses developing (Figure 4). Instead of re-operation, using conservative treatment with antibiotics, there was no organ failure emerging. However, several lung nodules still existed on the radio appearance after one-month treatment. For the aim of making an exact diagnosis, CT-guided needle biopsy of the lesion was conducted and histological features of the specimen revealed: chronic inflammation, characterized by hyperplasia of fibrous tissues, hyalinization and necrotic tissues (Figure 5). There is no evidence of tuberculosis and other pathogens for these foci. The patient was currently symptom free and then discharged home 40 days after hospitalization. No relapse was observed during the 1-year follow-up period.

Discussion
Even though median sternotomy is the gold standard for patients with MG, VATS have been increasingly applied in extended thymectomy because of good aesthetic outcomes, less trauma and a lower incidence of postoperative complications, especially myasthenic crisis. VATS for extended thymectomy is performed by various approaches, and widely adopted by left or right route. However, this minimally invasive procedure can not provide a sufficient visualization of bilateral upper thymus lobes and the contralateral phrenic nerve. Compared with unilateral thoracoscopic approach, the trans-subxiphoid route does not require one-lung ventilation, provide less intercostal nerve damage and can obtain the same operation field as sternotomy, which is essential for adequate anterior mediastinal adipose tissues and intact thymus dissection. Since the subxiphoid route has some advantages, Suda et al. (3) has attempted to perform single-port thymectomy via a single subxiphoid incision and trans-subxiphoid robotic thymectomy.
TsVATET is preformed through the subxiphoid route and has also been proved to be a safe and feasible surgical procedure, especially for extended thymectomy. According to Hsu and his colleagues (1), the comparison of postoperative complications for the subxiphoid approach and the unilateral route showed no significant difference. They performed TsVATET for 23 non thymomatous myasthenic patients in 2001 to 2003, Except for one patient who needed prolonged ventilator support, there were no other surgical complications or mortalities. And since January 1, 2015, we have performed TsVATET for 25 patients with MG or anterior mediastinal masses, two of whom suffered from post-surgical subxiphoid wound complications. One is fat liquefaction (not being reported), while the other is the presented case.
According to the available literature, there are few papers about postoperative infection for patients who received neither open nor VATS extend thymectomy. Andreas Machens et al. (4) carried out a retrospective analysis of 125 patients who had undergone transsternal thymectomy for myasthenia gravis. In their study, postoperative wound infection and mediastinitis occurred in 2.4% and 1.6% of the patients. So in our opinions, the presented case seems to be an important case report to the attention. The authors speculate that the subxiphoid wound is more vulnerable than the intercostals incision, especially for patients taking steroid or immunosuppressants. There may exist three potential risks for the subxiphoid incision complications: (I) compared with the intercostals wound which contains three layers of muscle and intercostal artery which originated directly from aorta, the subxiphoid longitudinal incision was made along the linea alba which has a poorer blood supply, so it is relatively easy to develop wound complications, such as poor healing or infection; (II) the unilateral thoracoscopic approach provide a wide room for the assistant to manipulate the thoracoscopy. On the contrary, as for the subxiphoid route, the pulsatile heart, diaphragm and sternum make up a narrow space which seriously limits the thoracoscopy movement although the bilateral mediastinal pleura were routinely opened and CO2 was injected to widen the space behind the sternum, so in order to improve exposure and avoid interfering with bilateral forceps use, the thoracoscopy inevitably long-time compress the surrounding tissues of the subxiphoid incision to obtain an appropriate orientation of the camera head. This may be another precipitating factor for the incision infection; (III) the patient chronically took tacrolimus and prednisone.
In particular, unlike the unilateral route, the subxiphoid incision communicates with the anterior mediastinum directly after TsVATET, infectious wound easily influences the anterior mediastinum, progressing to anterior mediastinitis. Meanwhile, bilateral mediastinal pleura were routinely opened, so the right and left thoracic cavity communicated in the anterior mediastinum after thymectomy, secondary infection of bilateral pleural cavity or pneumonia may happen after anterior mediastinitis. Unfortunately, our case developed bilateral multiple lung abscesses after pneumonia. Through Anti-infection treatment combined with anterior mediastinum irrigation and drainage, the patient recovered.
Conclusions
In view of the characteristics of the subxiphoid incision, the authors feel that this severe infection is not an incidental complication for TsVATET. We should be careful and prevent anterior mediastinitis, the infection of bilateral pleural cavity, pneumonia and multiple lung abscesses following subxiphoid incision infection when we perform TsVATET for patients with MG.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Hsu CP, Chuang CY, Hsu NY, et al. Comparison between the right side and subxiphoid bilateral approaches in performing video-assisted thoracoscopic extended thymectomy for myasthenia gravis. Surg Endosc 2004;18:821-4. [Crossref] [PubMed]
- Wu L, Lin L, Liu M, et al. Subxiphoid uniportal thoracoscopic extended thymectomy. J Thorac Dis 2015;7:1658-60. [PubMed]
- Suda T, Kaneda S, Hachimaru A, et al. Thymectomy via a subxiphoid approach: single-port and robot-assisted. J Thorac Dis 2016;8:S265-71. [PubMed]
- Machens A, Emskötter T, Busch C, et al. Postoperative infection after transsternal thymectomy for myasthenia gravis: a retrospective analysis of 125 cases. Surg Today 1998;28:808-10. [Crossref] [PubMed]