Excision of middle mediastinal parathyroid adenoma by videoscopic assisted mediastinoscopy (VAM)
Introduction
Symptomatic hypercalcemia from primary hyperparathyroidism secondary to a middle mediastinal parathyroid adenoma is an uncommon occurrence. Careful preoperative localization, intra-operative monitoring and surgical approach is crucial for successful complete surgical excision with least associated morbidity possible. We present a case of a middle mediastinal parathyroid adenoma treated successfully through the use of videoscopic assisted mediastinoscopy (VAM).
Case presentation
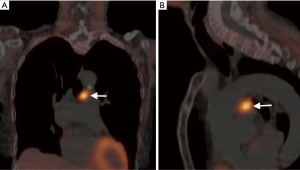
A 77-year-old female with a past medical history of dyslipidemia, hypertension and osteoporosis presented with a 6-month history of polyuria and renal colic due to recurrent stone formation. Blood work revealed an elevated calcium level of 2.80 mmol/L (normal range, 2.10–2.60 mmol/L) with a normal albumin level. Intact parathyroid hormone (iPTH) level was elevated at 29.9 pmol/L (normal range, 1.1–6.8 pmol/L). A high-resolution ultrasound of the neck revealed a 1.7 cm × 1.0 cm homogenous, non-cystic nodule within the right lower lobe of the thyroid. A fine needle aspirate was performed with pathology revealing features consistent with a benign thyroid nodule. Subsequently single-photon emission computed tomography (SPECT/CT) imaging of the neck and chest was performed in order to facilitate parathyroid localization. Intense radiotracer uptake was seen on initial and delayed images within the middle mediastinum, corresponding to a soft tissue density measuring 2.3 cm × 1.7 cm (Figure 1). No lymphadenopathy in the neck or mediastinum was seen.
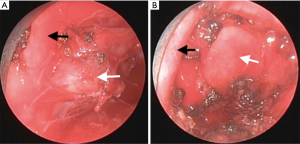
Given the location of the adenoma within the mediastinum; VAM, video assisted thoracoscopic surgery and thoracotomy were surgical options discussed with the patient. VAM combined with intra-operative iPTH level monitoring was the initial procedure of choice given the low associated surgical morbidity. The patient was placed in supine position with slight extension of the neck. The baseline intact PTH level taken was found to be 23.7 pmol/L (normal range, 1.1–6.8 pmol/L). A small transverse suprasternal incision was made. The subcutaneous tissues were divided and the strap muscles were divided in the midline. Blunt dissection was used to enter the mediastinum, at which point the video mediastinoscope was inserted. No masses or lymphadenopathy was noted. Initial dissection included en bloc resection of the 4R lymph node station. This allowed for clear visualization of the azygous vein entering the vena cava as well as aortic arch. Inferiorly, a homogenous pale yellow mass inconsistent with mediastinal fat was found adjacent to the left pulmonary artery and aortic arch (Figure 2A,B). A clear plane of dissection was achieved between the adenoma and the left mainstem bronchus using a combination of cautery and surgical clips in order to control the arterial and venous blood supply of the adenoma. The iPTH levels 5 and 10 minutes after the parathyroid adenoma excision were found to be <0.6 pmol/L. Intra-operative frozen section confirmed the presence of parathyroid tissue. Final pathology revealed uniform parathyroid tissue consisting of polygonal chief cells with small, centrally placed nuclei exhibiting oncocytic change lacking chief cell hyperplasia, all of which are consistent with a parathyroid adenoma (1). Blood work performed four months post-operatively revealed both normal calcium and iPTH levels with complete resolution of her presenting symptoms.
Discussion
Primary hyperparathyroidism affects approximately 0.1–0.5% of the population with the incidence increasing after the age of 50 (1). The majority of primary hyperparathyroidism cases are secondary to a single parathyroid adenoma (range, 75–80%). Multiple adenomas and parathyroid hyperplasia combined constitute the majority of remaining cases, with parathyroid carcinoma accounting for approximately 1% of cases (2). Up to 25% of adenomas may be ectopic with an estimated 2% situated in the mediastinum (2). The small subset of patients with mediastinal parathyroid adenomas present unique management issues. Imaging contributes a pivotal role in deciding the procedure of choice. A technetium Tc 99m sestamibi–sodium iodide I123 para-thyroid subtraction scintigram alone or combined with SPECT/CT are routinely performed with sensitivities exceeding 90% (3). Selective venous catheterization and PTH measurement can be utilized if diagnostic uncertainty exists, however its invasiveness limits clinical applicability (3). Intra-operative iPTH measurement is an extremely vital measure as distinguishing parathyroid tissue in the mediastinum may be very difficult. An iPTH level decrease of at least 50% from the preoperative baseline is a strong predictor of future long-term normocalcemia (4,5). Intra-operative iPTH monitoring provides direct assurance of complete parathyroid adenoma excision and rules out the possibility of patients who are image negative with multiple gland involvement. Its use decreases the failure rate from 21.3% to approximately 3% (4). The vast majority (~90%) of parathyroid carcinomas are functional (6). Patients tend to have more severe symptomatology at presentation than individuals with a functional adenoma, with 50% having bone or renal disease. Carcinoma must be kept in the differential of the five hyperparathyroid patients.
Conclusions
Successful surgical excision using VAM resulted in complete resolution of the patient’s hyperparathyroidism with a return to normocalcemia. VAM should be considered as a surgical option given the thoracic surgeon’s familiarity with the procedure and the potential for curative excision with minimal associated morbidity as compared to a sternotomy or thoracotomy. Precise preoperative localization and intraoperative iPTH monitoring are critical in achieving complete surgical resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Maitra A. The endocrine system. In: Kumar V, Abbas AK, Fausto N, et al. editors. Robbins and cotran pathological basis of disease. 8th ed. Philadelphia: Elsevier, 2009:1097-164.
- Boushey RP, Todd TR. Middle mediastinal parathyroid: diagnosis and surgical approach. Ann Thorac Surg 2001;71:699-701. [Crossref] [PubMed]
- Vazquez BJ, Richards ML. Imaging of the thyroid and parathyroid glands. Surg Clin North Am 2011;91:15-32. [Crossref] [PubMed]
- Sagan D, Goździuk K. Surgical treatment of mediastinal parathyroid adenoma: rationale for intraoperative parathyroid hormone monitoring. Ann Thorac Surg 2010;89:1750-5. [Crossref] [PubMed]
- Carneiro DM, Solorzano CC, Nader MC, et al. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery 2003;134:973-9; discussion 979-81. [Crossref] [PubMed]
- McClenaghan F, Qureshi YA. Parathyroid cancer. Gland Surg 2015;4:329-38. [PubMed]


