
Comparing the lung isolation efficacy of bronchial blocker positioning via electromagnetic navigation bronchoscopy versus fiberoptic bronchoscopy: a randomized study
Highlight box
Key findings
• Electromagnetic navigation bronchoscopy (ENB)-guided bronchial blocker (BB) positioning demonstrates superior and more rapid lung collapse effects compared with conventional fiberoptic bronchoscopy (FOB)-guided BB placement.
What is known and what is new?
• FOB has been used for the real-time visualization of the airway anatomy to guide BB positioning for lung isolation.
• ENB-guided BB positioning is also an efficient method of lung isolation.
What is the implication, and what should change now?
• ENB-guided BB positioning shows potential for lung isolation, warranting further research to clarify its effectiveness and optimal usage in thoracic surgery.
Introduction
Lung isolation is commonly employed in clinical practice to achieve optimal exposure during surgery and create ideal therapeutic conditions. Bronchial blockers (BBs) are particularly effective for lung isolation in patients with limited mouth opening, a history of neck radiation therapy, a need for selective lobar blockade, or a requirement for postoperative ventilation support (1-3).
Electromagnetic navigation bronchoscopy (ENB) has become an effective tool for diagnosing peripheral pulmonary lesions, offering lower complication rates compared with traditional invasive techniques (4-6). ENB is also employed to assist in nodule localization during simultaneous thoracoscopic sub-lobectomies (7,8). Considering that a single-lumen tracheal tube serves as the common pathway for ENB and subsequent one-lung ventilation (OLV), utilizing a BB is suitable for achieving lung isolation during these procedures (9). Although fiberoptic bronchoscopy (FOB) has been used for the real-time visualization of the airway anatomy, its misplacement rate can exceed 30% due to practitioner inexperience and difficulties in identifying the anatomical structure of the distal bronchus occluded by the BB (10-12). Therefore, improved strategies for lung isolation should be developed in clinical practice.
Currently, the effectiveness and accuracy of ENB-guided BB placement for lung isolation have not been clarified. Therefore, this study aimed to compare the efficacy of lung isolation using ENB-guided versus FOB-guided BB placement in thoracic procedures requiring OLV. We hypothesize that ENB-guided BB placement has a significantly different effect on lung collapse than FOB-guided BB placement. We present this article in accordance with the CONSORT reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1516/rc).
Methods
Study design and participants
We conducted a single-center, parallel-group, randomized, assessor-masked, controlled, equivalence trial to compare the effects of lung isolation using BBs positioned with ENB versus FOB for thoracic surgeries. Patients were randomly assigned in a 1:1 ratio to receive either ENB or FOB for BB placement. The trial was performed at the Ninth People’s Hospital of Shanghai Jiao Tong University School of Medicine and was approved by the hospital’s Ethics Committee (approval No. SH9H-2023-T250-2). This study adhered to the principles of the Declaration of Helsinki (as revised in 2013) and was registered with the China Clinical Trial Registry before patient enrollment (registration No. ChiCTR2300076133, principal investigator: Rong Hu, date of registration: 2023-09-26). Informed consent was obtained from all individual participants. In total, 106 patients who underwent elective thoracoscopic surgery under OLV were enrolled.
Patient inclusion criteria were as follows: age, 18–85 years; scheduled for elective thoracoscopic surgery (including lung wedge resection, segmental resection, or lobectomy) under OLV; classified as American Society of Anesthesiologists (ASA) grade I or II; intraoperative ENB usage; and provision of informed consent. Exclusion criteria included severe lung diseases, such as pulmonary atelectasis and chronic obstructive pulmonary disease, recent respiratory tract infections, severe cardiovascular disease, or any contraindications to BB placement. Eligible patients were identified from operating room schedules or preadmission clinics and were recruited from the preadmission areas of the operating floor.
Randomization and masking
Patients were randomly assigned in a 1:1 ratio to receive either ENB or FOB for BB placement. Randomization was performed using a computer-generated random-allocation sequence, with blocks of four and a random seed of 111, implemented via the “blockrand” package in R (version 4.0.5; https://www.r-project.org) by a research assistant who was not involved in primary data collection or entry. The FOB group served as the control. The randomization results were stored in sequentially numbered opaque envelopes. Only the anesthesiologist knew the assignment of the patients, while both patients and surgeons responsible for evaluating lung isolation effects were blinded to the trial grouping.
Procedures
All patients were admitted to the operating room while lying flat on a surgical bed equipped with a magnetically navigated electromagnetic plate. Venous access was subsequently established in the nonsurgical upper extremity. All patients underwent standard monitoring, including heart rate (HR), noninvasive blood pressure, mean arterial pressure (MAP), and oxygen saturation (SpO2) by pulse oximetry. For most patients, a 9-Fr BB (EBT0209, Tampa, China) was used to ensure complete bronchial occlusion, as recommended by the manufacturer for normal-sized adults. A single-lumen tracheal tube with a 7.5-mm internal diameter was used along with the 9-Fr BB. However, a single-lumen tracheal tube with a 7.0-mm internal diameter was used with a 7-Fr BB (EBT0207, Tampa) in the following cases: patients weighing <45 kg, <150 cm tall, or when the 7.5-mm single-lumen tracheal tube could not pass smoothly through the vocal folds. Anesthesia was administered by the same senior and resident anesthesiologists.
All patients underwent positive pressure ventilation using a mask for at least 3 min. Anesthesia was induced with intravenous injections of penehyclidine hydrochloride (0.01 mg/kg), dolasetron (12.5 mg), midazolam (0.05 mg/kg), sufentanil (0.2–0.4 µg/kg), propofol (1–2 mg/kg), and rocuronium (0.6 mg/kg). During the induction, the radial artery on the same side as the venous access was punctured and cannulated for invasive blood pressure monitoring, and the first arterial blood gas analysis was performed simultaneously. A single-lumen tracheal tube (Teleflex, USA) was inserted under video laryngoscopy by an experienced anesthesiologist. Additionally, the right internal jugular vein was punctured in all patients, and a double-lumen central venous catheter was placed to provide deep venous access.
Image registration was performed to construct a three-dimensional virtual airway roadmap, enabling the localization of target lesions using the ENB guidance system. Surgeons first use ENB through the single-lumen tracheal tube to locate lung lesions. A BB was then placed to achieve lung isolation for the subsequent surgical procedure. Peak airway pressure (Ppeak), HR, and MAP were measured immediately before BB positioning (T1).
For patients assigned to the ENB group, the BB was placed under magnetic navigation guidance. The magnetic navigation guidewire was inserted through the FOB inlet of the BB, with its cephalic end aligned with the rounded bulge of the blue demarcation line proximal to the trocar. This ensured that the positioning catheter remained snug and parallel to the BB, in the same direction as the trocar’s bend. A sterile patch was cut into 5-mm-wide strips and secured in a continuous spiral from the tip of the localization catheter to the “15 cm” mark of the BB. The guidewire and BB were fixed tightly and kept parallel (Figure 1) to ensure that the relative positions of the positioning catheter and BB remained stable during the procedure. During magnetic navigation, registration was conducted by driving the guidewire through segments of both sides of the bronchial tree to align the actual and virtual bronchi. Navigation followed the virtual pathway using live airway visualizations displayed alongside the virtual pathway on the system cart monitor. After applying petroleum jelly to lubricate the cuff, the BB was inserted in the appropriate position in the bronchus on the isolation side under magnetic navigation guidance. We aimed to locate the center of the BB cuff at the midpoint of the main bronchus. The distance between the guidewire and the center of the cuff was fixed at 2 cm for the 9-Fr BB and 1.5 cm for the 7-Fr BB (Figure 2).

For patients in the FOB group, the BB was positioned under FOB guidance. The BB was adjusted such that the proximal end of the cuff was positioned approximately 1 cm below the tracheal carina within the left bronchus or 0.5 cm below the tracheal carina within the right bronchus.
In both groups, the respiratory circuit and the tracheal catheter were disconnected, and the apnea method was performed. After 30 s, the cuff was inflated without herniating into the tracheal carina, ensuring that the cuff pressure did not exceed 30 cmH2O (13). The inflation volume was based on the BB size, determined by the diameter of the main bronchus measured according to the computed tomography (CT) image, as follows:
- For the 7-Fr BB with a diameter of less than 10 mm, an inflation volume of 2 mL was used.
- For the 7-Fr BB with a diameter of 10 mm or more, an inflation volume of 3 mL was used.
- For the 9-Fr BB with a diameter of less than 15 mm, an inflation volume of 4 mL was used.
- For the 9-Fr BB with a diameter of 15 mm or more, an inflation volume of 5 mL was used.
The duration of BB positioning was defined as the time from when the BB tip entered the tracheal tube until it reached a position that ensured satisfactory ventilation. The number of positioning attempts was recorded for both groups. Furthermore, the HR, MAP, and Ppeak were recorded immediately after positioning was completed (T2).
After inflating the BB cuff to initiate OLV, mechanical ventilation was performed in the volume-controlled mode with the following parameters: tidal volume, 4–6 mL/kg (ideal body weight); respiratory rate, 12–14 breaths per min; inspiratory/expiratory ratio, 1:2; fresh gas flow, 2 L per min; FiO2, 100%. The partial pressure of end-tidal carbon dioxide was maintained at 35–45 mmHg, and Ppeak was maintained at <30 cmH2O. After OLV began, the patient was adjusted to a lateral position; the cuff remained inflated during this period.
In both groups, the BB position was directly evaluated when the surgeon opened the pleura. If the surgeon was dissatisfied with lung deflation [verbal analogue scale (VAS) score <5] immediately after opening the pleura, FOB was used to reconfirm the BB position. If the BB position was found to have shifted, we assumed that the BB was displaced while the patient was positioned in the lateral decubitus position.
Outcomes
The primary outcome was the effect of lung collapse, assessed immediately after intraoperative pleural opening by a surgeon who was blinded to the trial grouping. The degree of lung collapse was scored using the VAS, where 0 indicated no collapse, and 10 indicated complete collapse (14). Secondary outcomes included blood gas analysis, blood counts on the first postoperative day, and the incidence of postoperative pulmonary complications. Details of these measures are as follows:
Blood gas analysis was conducted in both groups after 10 and 30 min of OLV. Arterial oxygen pressure (PaO2) and arterial carbon dioxide pressure (PaCO2) were also recorded at these time points. The incidence of BB displacement after position changes and the frequency of intraoperative FOB use were also recorded. On the first postoperative day, blood counts (hemoglobin, leukocyte, platelet, and neutrophil levels) and C-reactive protein (CRP) levels were recorded for both groups. After the patients were discharged from the hospital, the incidence of postoperative pulmonary complications, as identified by chest plain CT scan (pleural effusion, pulmonary atelectasis, or lung inflammation), along with the total days of hospitalization, days in the intensive care unit, and total hospitalization costs, were recorded.
All study data were sent to the Ninth People’s Hospital of Shanghai Jiao Tong University School of Medicine. All data forms were reviewed by a research assistant who was not involved in primary data collection or entry. Data on test forms not completed according to the test manual instructions were discarded.
Statistical analysis
Based on previous literature (14), the mean value of the VAS lung collapse score is 6 and the standard deviation (SD) is 1.5. Due to VAS being a relatively new indicator in lung collapse score, we were unable to obtain a clear clinical efficacy threshold. We assumed that a mean difference of about 0.7 (about 0.5 SD point) change between the two groups had clinical significance. Thus, a sample size of 106 patients (53 in each group) was deemed sufficient for providing 80% power to detect a significant difference of lung collapse score to a two-sided α-level of 5%.
Data were anonymized before statistical analyses, which were performed using R version 4.0.5. Hypothesis tests were used to compare differences between groups. All indicators were described based on their nature. Continuous variables were analyzed according to their distribution. For non-normally distributed data, including correct BB positioning time, anesthesia and surgery duration, intraoperative blood loss, CRP levels, hospitalization days, and total hospitalization costs, the median (P25, P75) was used for presentation, and the rank sum test was applied for analysis. The remaining data, which conformed to a normal distribution, were expressed as mean (SD), and analyzed using a t-test. Categorical variables were analyzed using the Chi-squared test or Fisher’s exact test.
All tests were two-sided, with P values <0.05 considered statistically significant. Additionally, 95% confidence intervals (CIs) were calculated.
Results
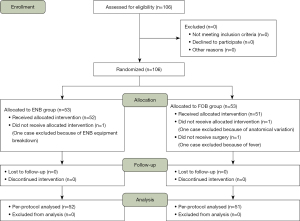
From September 2023 to March 2024, 106 patients were enrolled in this study. Two patients were excluded from the FOB group due to changes in surgical plans, and one patient was excluded from the ENB group due to a malfunction of the ENB device. Consequently, 103 patients participated in this trial, with 51 patients in the FOB group and 52 in the ENB group (Figure 3). Outcome analyses were performed in the per-protocol population (n=103).
No significant differences were observed in the general condition of the patients between the groups (Table 1). The ENB group showed a trend towards less intraoperative blood loss compared to the FOB group [80.00 (50.00, 100.00) vs. 100.00 (70.00, 100.00), P=0.10]. Tables 2,3 show the primary and secondary outcomes for continuous and categorical variables, respectively.
Table 1
| Parameter | ENB group (n=52) | FOB group (n=51) | P value |
|---|---|---|---|
| Age (years) | 54.25 (13.47) | 56.29 (11.95) | 0.42 |
| Sex (male/female) | 19/33 | 14/37 | 0.44 |
| Body mass index (kg/m2) | 23.9 (3.85) | 23.70 (3.34) | 0.80 |
| Surgical site (left/right) | 24/28 | 16/35 | 0.18 |
| Basal SpO2 (%) | 97.90 (1.32) | 98.10 (1.27) | 0.49 |
| Duration of anesthesia (min) | 150.00 [135.00, 198.75] | 150.00 [135.00, 195.00] | 0.85 |
| Duration of surgery (min) | 127.50 [105.00, 168.75] | 150.00 [105.00, 165.00] | 0.71 |
| Intraoperative blood loss (mL) | 80.00 [50.00, 100.00] | 100.00 [70.00, 100.00] | 0.10 |
Data are number of patients, mean (standard deviation), or median [P25, P75]. Different display methods and statistical analysis are chosen based on data distributed types. ENB, electromagnetic navigation bronchoscopy; FOB, fiberoptic bronchoscopy; SpO2, peripheral capillary oxygen saturation.
Table 2
| Parameter | ENB group (n=52) | FOB group (n=51) | Mean/median difference (95% CI) | P value |
|---|---|---|---|---|
| Lung collapse score (VAS) | 9.08 (1.36) | 8.24 (1.93) | 0.842 (0.186, 1.497) | 0.01* |
| Time for placement BB in the correct position (s) | 13.00 [10.00, 20.25] | 49.00 [35.00, 75.00] | −36 (−45, −30) | <0.001* |
| HR (bpm) | ||||
| Baseline | 72.72 (10.90) | 73.87 (10.88) | 2.316 (−1.942, 6.574) | 0.28 |
| T2 | 66.27 (10.59) | 68.31 (11.55) | −2.044 (−6.377, 2.288) | 0.35 |
| T2-baseline | −7.60 (13.06) | −3.24 (13.95) | −4.361 (−9.645, 0.924) | 0.23 |
| MAP (mmHg) | ||||
| Baseline | 101.90 (11.41) | 100.10 (12.44) | 1.806 (−2.863, 6.474) | 0.44 |
| T2 | 66.12 (10.84) | 65.90 (9.62) | 0.213 (−3.791, 4.218) | 0.92 |
| T2–baseline | −35.79 (15.60) | −34.20 (14.93) | −1.592 (−7.56, 4.375) | 0.30 |
| Ppeak (cmH2O) | ||||
| T1 | 14.90 (3.69) | 15.35 (3.13) | −0.449 (−1.786, 0.888) | 0.51 |
| T2 | 22.21 (5.57) | 23.10 (5.35) | −0.887 (−3.021, 1.248) | 0.41 |
| T2–T1 | 7.31 (2.45) | 7.75 (4.27) | −0.437 (−1.806, 0.931) | 0.52 |
| PaO2 (mmHg) | ||||
| Before one-lung ventilation | 321.46 (74.76) | 334.45 (68.24) | −12.989 (−40.959, 14.98) | 0.45 |
| One-lung ventilation for 10 min | 176.83 (114.13) | 163.04 (112.11) | 13.788 (−30.433, 58.009) | 0.54 |
| One-lung ventilation for 30 min | 235.94 (70.24) | 233.57 (72.50) | 2.374 (−25.537, 30.284) | 0.87 |
| PaCO2 (mmHg) | ||||
| Before one-lung ventilation | 44.15 (5.37) | 44.96 (5.61) | −0.807 (−2.953, 1.339) | 0.46 |
| One-lung ventilation for 10 min | 56.83 (7.29) | 59.65 (8.87) | −2.82 (−5.999, 0.359) | 0.08 |
| One-lung ventilation for 30 min | 57.40 (7.77) | 60.24 (8.69) | −2.831 (−6.057, 0.394) | 0.08 |
| Hemoglobin (g/L) | 124.37 (14.53) | 123.04 (16.47) | 1.326 (−4.749, 7.401) | 0.67 |
| White blood cells (×109/L) | 12.96 (4.06) | 12.54 (3.00) | 0.418 (−0.976, 1.813) | 0.55 |
| Platelets (×109/L) | 202.77 (52.41) | 192.65 (58.04) | 10.122 (−11.51, 31.755) | 0.36 |
| Neutrophils (%) | 87.97 (4.24) | 89.08 (3.88) | −1.105 (−2.695, 0.484) | 0.17 |
| C-reactive protein (mg/L) | 29.80 [15.20, 63.60] | 30.95 [15.68, 57.35] | −1.15 (−13.5, 23.42) | 0.68 |
| Hospitalization days (days) | 7.00 [5.00, 8.00] | 6.00 [5.00, 7.00] | 1 (−0.5, 2) | 0.08 |
| Total hospitalization expenses (RMB/thousands yuan) | 83.88 [74.49, 97.31] | 83.86 [76.39, 94.62] | 0.02 (−9.31, 8.37) | 0.63 |
Data are presented as mean (standard deviation) or median [P25, P75]. mean/median difference is shown with 95% confidence interval (CI). *, significant difference (P<0.05). Different display methods and statistical analysis are chosen based on data distributed types. ENB, electromagnetic navigation bronchoscopy; FOB, fiberoptic bronchoscopy; VAS, verbal analogue scale; BB, bronchial blocker; HR, heart rate; T2, after localization of bronchial blocker; T2-baseline, variation between baseline and after localization; T1, before localization of bronchial blocker; T2–T1, variation between before and after localization; MAP, mean arterial pressure; Ppeak, peak airway pressure; PaO2, arterial oxygen pressure; PaCO2, arterial carbon dioxide pressure.
Table 3
| Parameter | ENB group (n=52) | FOB group (n=51) | P value |
|---|---|---|---|
| Position frequency of BB (once/twice/thrice) | 51/1/0 | 45/5/1 | 0.13 |
| Displacement of BB when posture changing (no/yes) | 51/1 | 45/6 | 0.11 |
| The number of times the BB malpositioned intraoperatively (zero/once/twice) | 50/2/0 | 45/5/1 | 0.28 |
| The number of intraoperative repositioning of BB with FOB (zero/once/twice) | 48/4/0 | 40/10/1 | 0.12 |
| Postoperative pulmonary complications (yes/no) | 41/11 | 42/9 | 0.84 |
Data are presented as number of patients. ENB, electromagnetic navigation bronchoscopy; FOB, fiberoptic bronchoscopy; BB, bronchial blocker.
Immediately after pleural opening, the VAS score for the pulmonary isolation effect was higher in the ENB group than in the FOB group [9.08 (1.36) vs. 8.24 (1.93), P=0.01]. The time required for BB positioning was significantly shorter in the ENB group than in the FOB group [13.00 (10.00, 20.25) vs. 49.00 (35.00, 75.00), P<0.001]. The frequency of BB positioning, the incidence of BB displacement after body positional changes or during the procedure, and the frequency of intraoperative FOB use did not differ significantly between the two groups.
HR and MAP did not differ significantly between the two groups at baseline and T2, and the difference in HR and MAP values from the baseline to T2 were comparable between the two groups. The Ppeak values at T2 and T1 did not differ significantly between the two groups. Although arterial PaCO2 levels were lower in the ENB group than in the FOB group at 10 min [56.83 (7.29) vs. 59.65 (8.87)] and 30 min [57.40 (7.77) vs. 60.24 (8.69)] after OLV, these differences were not statistically significant.
Postoperative levels of hemoglobin, leukocytes, platelets, neutrophils, and CRP, as well as the incidence of postoperative pulmonary complications (pleural effusion, pulmonary atelectasis, or lung inflammation), total days of hospitalization, days in the intensive care unit, and total hospitalization costs, did not differ significantly between the two groups.
Discussion
The FOB is widely regarded as the “gold standard” for optimizing BB placement in thoracic surgeries (15). However, despite their experience, anesthesiologists cannot completely eliminate the risk of undetected BB displacement during OLV (16). To the best of our knowledge, this is the first study to analyze the use of ENB for BB placement. Our findings indicate that ENB-guided BB placement achieved superior lung isolation for OLV than FOB-guided BB placement. Specifically, the ENB group demonstrated significantly higher lung collapse scores than those in the FOB group (P=0.01). Additionally, while the number of BB positioning attempts, the incidence of BB displacement after body positional changes or during the procedure, and the frequency of FOB use for BB replacement were lower in the ENB group, these differences were not statistically significant. These results indicate that ENB improves the quality of BB-mediated lung isolation during OLV.
For over a decade, ENB has been extensively used for identifying fiducial markers in lung stereotactic body radiation therapy, marking the pleura during surgical resection, and assisting in the diagnosis of peripheral pulmonary lesions and mediastinal lymph nodes (17-19). By integrating preprocedural CT scans with real-time magnetic-based positioning, ENB generates three-dimensional virtual images of bronchial and lung structures, enabling precise targeting of peripheral pathological lesions <20 mm (14). In this study, we investigated the impact of the ENB system on enhancing lung isolation efficacy. Our findings show that lung collapse scores were significantly higher in the ENB group than in the FOB group [9.08 (1.36) vs. 8.24 (1.93)]. The ability of the ENB system to virtually visualize the bronchial tree facilitated real-time placement of the BB, thereby minimizing the risk of positioning the BB too close to the main or distal bronchi. Conversely, FOB relies on two-dimensional imaging, which may impair the clinical assessments of anesthesiologists and increase the likelihood of BB displacement. Furthermore, the average lung collapse scores in both study groups exceeded those previously documented (14). Several factors may contribute to this phenomenon. First, all BB placements were performed by the same experienced and skilled thoracic anesthesiologist, a strategy that minimized technique-based systematic errors between the two groups. Second, 30-s circuit disconnection was employed before BB balloon inflation, which is a feasible strategy for improving lung deflation (20). Third, BB cuff inflation and OLV were initiated before changing the body position for sequential thoracic surgeries. This contributed to better lung collapse effects and improved the overall scores for lung isolation. In two cases, the BB dislodged from the right main bronchus due to surgical manipulation during mediastinal lymphadenectomy; however, heterogeneity in the right upper bronchus outlet may have also increased the difficulty of BB placement in these two patients (21).
Additionally, the positioning time was significantly shorter in the ENB group than that in the FOB group [13.00 (10.00, 20.25) vs. 49.00 (35.00, 75.00), P<0.001]. During ENB localization, the operator completed registration by maneuvering the guidewire to reach the main bilateral bronchus and trachea before initiating virtual navigation. This process increased airway secretions, which blurred the field of view during the sequential period of BB positioning with FOB. Thus, drainage of secretions in the airway may have extended the BB positioning time in the FOB group, especially in patients with chronic pulmonary inflammatory diseases. In contrast, airway secretions did not affect BB positioning in the ENB group. Once the guidewire was tightly fixed close to the BB cuff, the anesthesiologist advanced the wire-guided BB using the virtual map of the bronchial tree. It was reported that the success rate of ENB localization exceeded 90% after practicing for more than 12 times for locating peripheral lung lesions (22). Obviously, using ENB to place a BB is much easier since BB was positioned at the midpoint of the main bronchus. In this trial, after systemic training of utilizing ENB, we found that the shortest time required for BB positioning in the ENB group was only 6 s, which was almost impossible to achieve using FOB. Therefore, ENB-guided BB placement is a faster and more convenient method for lung isolation than FOB-guided BB placement.
In this study, the HR and MAP did not differ significantly between the two groups at the baseline and T2. Although the arterial PaO2 and PaCO2 did not differ significantly between the two groups after OLV, the carbon dioxide pressure remained relatively high in both groups, possibly due to local atelectasis caused by BB navigation. Despite this, the SPO2 in both groups remained at 100% during ENB (23). Further investigation is needed to clarify the effect of ENB on perioperative carbon dioxide exchange. Furthermore, using the same guidewire for BB positioning during the procedure incurred no extra fees. Postoperative blood tests, CRP levels, total days of hospitalization, and total hospitalization costs did not differ between the ENB and FOB groups. These results indicate that differences in lung collapse scores between the two BB placement methods did not translate into significant changes in postoperative blood cell analysis or systemic inflammatory markers.
There are several limitations in this clinical study. First, we included only patients who underwent ENB-guided lesion biopsy and sequential elective thoracic surgery. Second, during ENB-guided localization, the wire-guided bronchoscope occupied two-thirds of the tracheal tube, which may have led to insufficient ventilation. Subsequent BB positioning and instant cuff inflation may have affected lung collapse effectiveness. Additionally, we used the lung collapse score as the primary outcome. Although the scoring surgeon was blinded to the interventions used for BB positioning, their subjective evaluations may have introduced some systemic bias.
Conclusions
In conclusion, ENB-guided BB positioning is an efficient method for lung isolation. Compared to conventional FOB-guided BB placement, ENB-guided BB placement demonstrates a superior and more rapid effect on lung collapse.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1516/rc
Trial Protocol: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1516/tp
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1516/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1516/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1516/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Ninth People’s Hospital of Shanghai Jiao Tong University School of Medicine Ethics Committee (approval No. SH9H-2023-T250-2) and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huybrechts I, Tuna T, Szegedi LL. Lung separation in adult thoracic anesthesia. Saudi J Anaesth 2021;15:272-9. [Crossref] [PubMed]
- Collins SR, Titus BJ, Campos JH, et al. Lung Isolation in the Patient With a Difficult Airway. Anesth Analg 2018;126:1968-78. [Crossref] [PubMed]
- Zheng X, Zhang C, Lian S, et al. Extraluminal bronchial blocker placement using both nostrils for lung isolation in a patient with limited mouth opening: A CARE-compliant case report. Medicine (Baltimore) 2020;99:e21521. [Crossref] [PubMed]
- Muñoz-Largacha JA, Litle VR, Fernando HC. Navigation bronchoscopy for diagnosis and small nodule location. J Thorac Dis 2017;9:S98-S103. [Crossref] [PubMed]
- Li Y, Chen W, Xie F, et al. Novel electromagnetic navigation bronchoscopy system for the diagnosis of peripheral pulmonary nodules: a prospective, multicentre study. Thorax 2023;78:1197-205. [Crossref] [PubMed]
- Mehta AC, Hood KL, Schwarz Y, et al. The Evolutional History of Electromagnetic Navigation Bronchoscopy: State of the Art. Chest 2018;154:935-47. [Crossref] [PubMed]
- Wang K, Zhang Y, Xue M, et al. V7 ENB-guided thoracoscopic sublobectomy for stage IA synchronous multiple primary lung cancer. Thorac Cancer 2022;13:3467-76. [Crossref] [PubMed]
- Jeong JH, Park H, Choi CM, et al. Preoperative electromagnetic navigation bronchoscopy-guided one-stage multiple-dye localization for resection of subsolid nodules: A single-center pilot study. Thorac Cancer 2022;13:466-73. [Crossref] [PubMed]
- Shoni M, Rodriguez G. Intraoperative Anesthetic Management of the Thoracic Patient. Thorac Surg Clin 2020;30:279-91. [Crossref] [PubMed]
- Palaczynski P, Misiolek H, Szarpak L, et al. Systematic Review and Meta-Analysis of Efficiency and Safety of Double-Lumen Tube and Bronchial Blocker for One-Lung Ventilation. J Clin Med 2023;12:1877. [Crossref] [PubMed]
- Campos JH, Hallam EA, Van Natta T, et al. Devices for lung isolation used by anesthesiologists with limited thoracic experience: comparison of double-lumen endotracheal tube, Univent torque control blocker, and Arndt wire-guided endobronchial blocker. Anesthesiology 2006;104:261-6, discussion 5A. [Crossref] [PubMed]
- Langiano N, Fiorelli S, Deana C, et al. Airway management in anesthesia for thoracic surgery: a “real life” observational study. J Thorac Dis 2019;11:3257-69. [Crossref] [PubMed]
- Carassiti M, Mattei A, Pizzo CM, et al. Bronchial blockers under pressure: in vitro model and ex vivo model. Br J Anaesth 2016;117:i92-6. [Crossref] [PubMed]
- Yoo JY, Kim DH, Choi H, et al. Disconnection technique with a bronchial blocker for improving lung deflation: a comparison with a double-lumen tube and bronchial blocker without disconnection. J Cardiothorac Vasc Anesth 2014;28:904-7. [Crossref] [PubMed]
- Amin N, Tarwade P, Shetmahajan M, et al. A randomized trial to assess the utility of preintubation adult fiberoptic bronchoscope assessment in patients for thoracic surgery requiring one-lung ventilation. Ann Card Anaesth 2016;19:251-5. [Crossref] [PubMed]
- Shum S, Moreno Garijo J, Tomlinson G, et al. A Clinical Comparison of 2 Bronchial Blockers Versus Double-Lumen Tubes for One-Lung Ventilation. J Cardiothorac Vasc Anesth 2023;37:2577-83. [Crossref] [PubMed]
- Stowe H, Ogake S, Sharma S, et al. Improved respiratory motion tracking through a novel fiducial marker placement guidance system during electromagnetic navigational bronchoscopy (ENB). Radiat Oncol 2019;14:124. [Crossref] [PubMed]
- Zheng X, Cao L, Zhang Y, et al. A Novel Electromagnetic Navigation Bronchoscopy System for the Diagnosis of Peripheral Pulmonary Nodules: A Randomized Clinical Trial. Ann Am Thorac Soc 2022;19:1730-9. [Crossref] [PubMed]
- Taton O, Bondue B, Gevenois PA, et al. Diagnostic Yield of Combined Pulmonary Cryobiopsies and Electromagnetic Navigation in Small Pulmonary Nodules. Pulm Med 2018;2018:6032974. [Crossref] [PubMed]
- Zhao D, Yang N. Comparison of the effect between bronchial blocker and double-lumen endotracheal tube on pre-thoracotomy lung collapse in thoracoscopic surgery. China J Endosc 2022;28:14-20.
- Lu Y, Xu D, Liu Z, et al. The use of bronchial blockers in patients with aberrant tracheobronchial anatomy: a case report. Ann Transl Med 2021;9:1268. [Crossref] [PubMed]
- Shi J, He J, He J, et al. Electromagnetic navigation-guided preoperative localization: the learning curve analysis. J Thorac Dis 2021;13:4339-48. [Crossref] [PubMed]
- Pritchett MA, Lau K, Skibo S, et al. Anesthesia considerations to reduce motion and atelectasis during advanced guided bronchoscopy. BMC Pulm Med 2021;21:240. [Crossref] [PubMed]



