A convenient method for identifying a small pulmonary nodule using a dyed swab and geometric mapping
Introduction
Various marking techniques have been developed because of the difficulty in finding small-sized peripheral lung lesions during video-assisted thoracic surgery. In particular, computed tomography (CT)—guided lung needle marking is useful for identifying pulmonary nodules. However, complications sometimes cause severe after-effects or death, such as pneumothorax, intrapulmonary hematoma, hemothorax, and air embolism (1-5). Therefore, we developed a new CT-guided marking method that only requires a mark to be made with a magic marker on the body surface—and no thoracocentesis—and we identify small pulmonary nodules using gentian violet solution (triphenylmethane; Pyoctanin®) dye during the surgery. Additionally, we use a geometrically modified technique to identify the difficult location of the pulmonary nodule. Our method is so safe and easy that we have been applying it to locate the skin incision and confirm the margin for segmentectomy and the nodule in the frozen section.
Methods
This technique was performed on 51 lesions in 50 patients (22 males and 28 females) from September 2013 to December 2015. This study was waived by the Institutional Review Board of Maebashi Red Cross Hospital because of non-invasive method.

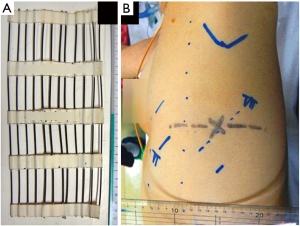
- Angiographic catheters were cut to about 15 cm in length, arranged in 12 rows 1 cm apart, and placed on the body surface as a marking device (Figure 3A). These materials did not produce a metal artifact;
- The patient was placed on the CT table, in the same manner as they would be positioned on the operating table, to draw a mark on the skin above the pulmonary nodule. A mark was placed with a magic marker on the body surface across a perpendicular line to the pulmonary nodule under CT guidance (Figure 3B);
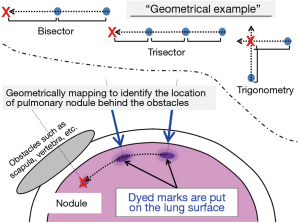
- We placed the mark on a bisected or trisected line when the nodule cannot be reached from the body surface (such as the apical portion, near the mediastinal and diaphragmatic surfaces, or behind the scapulae; Figure 4). We call this the “the geometrically modified technique”;
- The patient was intubated in the operating room with a double lumen endobronchial tube to allow unilateral ventilation. After administering general anesthesia, the patient was placed in the lateral position, so the marking site was exposed;
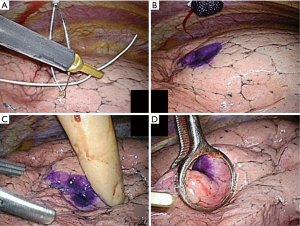
- A needle with a loop wire on the inner needle (Mini Loop Retractor II; Tyco Healthcare Japan, Tokyo, Japan) was placed on the marked skin. A thread with a small swab rinsed in 2% gentian violet solution was passed to the wire loop in the pleural space;
- The wire loop with the dye swab was taken out of the pleural space;
- The dye swab was put on the surface of the parietal pleura;
- Then, the lung was inflated and deflated, and dye marked the lung surface above the nodule by contacting with the dye swab;
- The nodule was confirmed by finger palpation through a port;
- The nodule was held using ring forceps, and a wedge resection was performed using a stapler.
Results
Mean patient age was 66.3 years (range: 37–97 years). Mean operating time was 145 min (range: 35–300 min), and mean blood loss was 14 g (range: 0–300 g).
The pulmonary nodules were primary lung cancer in 28, metastatic lung cancer in 15, and benign lung disease in 7 patients. The surgical procedure was a wedge resection in 24, lobectomy in 13, segmentectomy in 10, segmentectomy-segmentectomy in 2, and segmentectomy-wedge resection in 1 patient.
No complications were observed during the marking procedure. The nodules were solid in 29, ground-glass opacity in 13, and partially solid nodules in 9 patients. Mean nodule diameter was 10.9±5.5 mm (range: 2.8–22.6 mm), and mean error distance between the center of the nodule and the visceral pleura was 12.0±9.2 mm (range: 0–35.4 mm) as measured by CT.
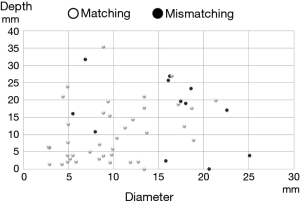
All lesions were identified by thoracoscopy. We confirmed the lesions by finger palpation through a surgical port. The stamped marking and finger palpation matched for almost all tumor lesions. The stamped marking was within about 1 cm from the lesion in all cases. The distribution of nodules according to depth, diameter, location, and matching is shown in Figures 5,6. Figure 5 shows marking-matching according to lobe. The matching rate was 77.8% in the right upper lobe, 75% in the right middle lobe, 84.6% in the right lower lobe, 84.6% in the left upper lobe, and 58.3% in the left lower lobe. Figure 6 shows that depth was not associated with diameter during marking-matching. Therefore, matching depended on the location of the pulmonary nodule.

No intra or postoperative mortality or morbidity was recorded.
Discussion
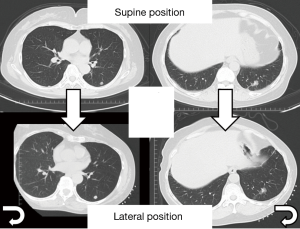
The nodules (lateral decubitus position) moved gravitationally during the operation because the patient’s position changed from supine. Additionally, the original location (lung inflated) of the nodule on the preoperative CT scan differed from that after the lung was deflated intraoperatively (Figure 7), which made it more difficult to identify small nodules. In addition, the small, impalpable ground-glass nodules were located deeply under the lung surface. Therefore, it was very important to mark the lesions preoperatively.
Various marking procedures have been used to localize nodules, such as intrathoracoscopic ultrasound (6-10), CT-guided coil injection (3), CT-guided localization of pulmonary nodules with a methylene blue injection (11), radioisotope marking under CT guidance and localization (12), colored collagen (13), vital dye (14-16), fluoroscopy (17,18) and percutaneous needle localization under CT guidance (4,5). These methods have several advantages and disadvantages (1). Although percutaneous CT-guided wire placement is a common technique (5) performed in many facilities, complications resulting from a visceral pleural puncture, such as pneumothorax, hemothorax, intrapulmonary hemorrhage, and an air embolism, have been reported (19). Marking techniques in which a contrast medium, such as barium sulfate, is injected via bronchoscopy have relatively fewer complications (17), but a thin bronchoscope and skilled practitioners are required. Therefore, these techniques are not available in all facilities. Additionally, a previously reported dye-stamp-marking method (14) cannot be applied to apical nodules or those on the mediastinal and diaphragmatic surfaces, or to the scapula; this is because they cannot be reached from the body surface. However, we modified the method using geometric coordinates of the pulmonary nodule. This method can be applied to all pulmonary nodules located near the pulmonary surface (Figure 4).
The advantages of our method are: (I) no risk for air embolism (2); (II) easy; (III) quick; (IV) non-invasive; (V) no need for hospitalization; and (VI) no need for last-minute marking before surgery. On the other hand, it is very difficult to localize deep impalpable pulmonary nodules that lie in the lung parenchyma. Nevertheless, conventional marking methods are difficult and risky to apply for deeper impalpable nodules.
Gentian violet solution is a blue dye and a potent antibacterial agent that is also commonly used for: (I) marking the skin for surgery and allergy testing; (II) treating Tinea infections (e.g., Athlete’s foot, jock itch, and ringworm); (III) treating Candida albicans and related infections (e.g., thrush and yeast infections); (IV) treating mouth ulcers; and (V) treating impetigo, primarily before antibiotics (but still useful for patients allergic to penicillin) (20). Gentian violet solution is highly viscous even at low concentrations.
We marked within 1 cm of the lesion in all cases to minimize the gap between the tumor and the mark because of the surgical position, marks on the body surface, and respiratory movements in the same position on the CT table as the patient is positioned in the operating room. Additionally, the matching rate was lower in the left lower lobe than that in the other lobes. No previous study has examined matching rate according to lesion location, probably because the left lower lobe is surrounded by dynamic organs, such as the diaphragm and heart, and moves with them.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was waived by the Institutional Review Board of Maebashi Red Cross Hospital because of non-invasive method and written informed consent was obtained from all patients.
References
- Sortini D, Feo C, Maravegias K, et al. Intrathoracoscopic localization techniques. Review of literature. Surg Endosc 2006;20:1341-7. [Crossref] [PubMed]
- Kamiyoshihara M, Sakata K, Ishikawa S, et al. Cerebral arterial air embolism following CT-guided lung needle marking. Report of a case. J Cardiovasc Surg (Torino) 2001;42:699-700. [PubMed]
- Asamura H, Kondo H, Naruke T, et al. Computed tomography-guided coil injection and thoracoscopic pulmonary resection under roentgenographic fluoroscopy. Ann Thorac Surg 1994;58:1542-4. [Crossref] [PubMed]
- Plunkett MB, Peterson MS, Landreneau RJ, et al. Peripheral pulmonary nodules: preoperative percutaneous needle localization with CT guidance. Radiology 1992;185:274-6. [Crossref] [PubMed]
- Ciriaco P, Negri G, Puglisi A, et al. Video-assisted thoracoscopic surgery for pulmonary nodules: rationale for preoperative computed tomography-guided hookwire localization. Eur J Cardiothorac Surg 2004;25:429-33. [Crossref] [PubMed]
- Shennib H, Bret P. Intraoperative transthoracic ultrasonographic localization of occult lung lesions. Ann Thorac Surg 1993;55:767-9. [Crossref] [PubMed]
- Santambrogio R, Montorsi M, Bianchi P, et al. Intraoperative ultrasound during thoracoscopic procedures for solitary pulmonary nodules. Ann Thorac Surg 1999;68:218-22. [Crossref] [PubMed]
- Sortini A, Carrella G, Sortini D, et al. Single pulmonary nodules: localization with intrathoracoscopic ultrasound -- a prospective study. Eur J Cardiothorac Surg 2002;22:440-2. [Crossref] [PubMed]
- Gow KW, Saad DF, Koontz C, et al. Minimally invasive thoracoscopic ultrasound for localization of pulmonary nodules in children. J Pediatr Surg 2008;43:2315-22. [Crossref] [PubMed]
- Kondo R, Yoshida K, Hamanaka K, et al. Intraoperative ultrasonographic localization of pulmonary ground-glass opacities. J Thorac Cardiovasc Surg 2009;138:837-42. [Crossref] [PubMed]
- Wicky S, Mayor B, Cuttat JF, et al. CT-guided localizations of pulmonary nodules with methylene blue injections for thoracoscopic resections. Chest 1994;106:1326-8. [Crossref] [PubMed]
- Sugi K, Kaneda Y, Hirasawa K, et al. Radioisotope marking under CT guidance and localization using a handheld gamma probe for small or indistinct pulmonary lesions. Chest 2003;124:155-8. [Crossref] [PubMed]
- Nomori H, Horio H. Colored collagen is a long-lasting point marker for small pulmonary nodules in thoracoscopic operations. Ann Thorac Surg 1996;61:1070-3. [Crossref] [PubMed]
- Kawada M, Okubo T, Poudel S, et al. A new marking technique for peripheral lung nodules avoiding pleural puncture: the intrathoracic stamping method. Interact Cardiovasc Thorac Surg 2013;16:381-3. [Crossref] [PubMed]
- Vandoni RE, Cuttat JF, Wicky S, et al. CT-guided methylene-blue labelling before thoracoscopic resection of pulmonary nodules. Eur J Cardiothorac Surg 1998;14:265-70. [Crossref] [PubMed]
- Willekes L, Boutros C, Goldfarb MA. VATS intraoperative tattooing to facilitate solitary pulmonary nodule resection. J Cardiothorac Surg 2008;3:13. [Crossref] [PubMed]
- Okumura T, Kondo H, Suzuki K, et al. Fluoroscopy-assisted thoracoscopic surgery after computed tomography-guided bronchoscopic barium marking. Ann Thorac Surg 2001;71:439-42. [Crossref] [PubMed]
- Moon SW, Wang YP, Jo KH, et al. Fluoroscopy-aided thoracoscopic resection of pulmonary nodule localized with contrast media. Ann Thorac Surg 1999;68:1815-20. [Crossref] [PubMed]
- Sakiyama S, Kondo K, Matsuoka H, et al. Fatal air embolism during computed tomography-guided pulmonary marking with a hook-type marker. J Thorac Cardiovasc Surg 2003;126:1207-9. [Crossref] [PubMed]
- Saji M, Taguchi S, Uchiyama K, et al. Efficacy of gentian violet in the eradication of methicillin-resistant Staphylococcus aureus from skin lesions. J Hosp Infect 1995;31:225-8. [Crossref] [PubMed]