
Incidence, mortality and survival of pleural mesothelioma in Zurich between 1981 and 2019, Switzerland
Highlight box
Key findings
• In men, the incidence rate of malignant pleural mesothelioma peaked in 2002, while in women it is still increasing. Mortality rates were stable over time and net survival was poor in both men and women.
What is known and what is new?
• Developed countries begun to prohibit the use of asbestos after being proven to be harmful, but due to the long latency time between exposure and the development of disease, incidence was expected to further increase for years after the ban.
• This is the first publication presenting a comprehensive analysis of pleural mesothelioma epidemiology within a Swiss canton using high quality population-based data. Using the gold standard method by Pohar Perme, we provide the first net survival estimate for pleural mesothelioma.
What is the implication, and what should change now?
• By assessing the disease burden of asbestos exposure by incidence, mortality and survival of pleural mesothelioma, decision makers can be better informed and prioritize prevention and further research.
Introduction
Malignant pleural mesothelioma is a rare tumour of the mesothelial cells of the pleura. It is frequently diagnosed in a late cancer-stage, and patients have, on average, a life expectancy of less than one year after diagnosis (1). Over the last 20 years, therapy has improved as surgical treatment, chemo-, radio- and immunotherapies emerged, but pleural mesothelioma is still a clinical challenge, and prognosis is poor (1,2).
Mesothelioma is mainly caused by occupational asbestos exposure and rarely due to environmental exposures like residing in a house with asbestos in the ventilation system, living near an asbestos factory or having a family member who is exposed to asbestos at work (3). There is a long latency time of 20–40 years between exposure and diagnosis of the disease (1). Asbestos was widely used, in particular in the construction industry, due to its high insulating capacities and its resistance to heat and chemicals (4). While developed countries started to prohibit the use of asbestos after being proven to be harmful to health, developing countries increased its production and use (1). Based on that and the long latency time between exposure and diagnosis of the disease, mesothelioma incidence is not yet decreasing worldwide (5). In 2020, around 31,000 cases of mesothelioma were diagnosed and around 26,000 patients died of it worldwide (6). Asbestos-related diseases annually cause medical costs between US$ 2.4 and 3.9 billion worldwide (7).
Switzerland is one of the first countries that banned asbestos; in fact, the import and use have been prohibited since 1990. The peak in asbestos import and use was in 1975–1978 and, therefore, the highest mesothelioma incidence was expected to be after 2015 (8). Between 2001 and 2019, the absolute number of malignant pleural mesothelioma cases in men increased based on insurance and hospital data (9).
However, the peak in mesothelioma incidence and mortality can vary within the country due to heterogeneous exposure and treatment. In Zurich, there is the University Hospital’s Department of Thoracic Surgery that is renowned for its mesothelioma treatment and therefore treatment might be more advanced than in other regions. Indeed, surgeons of the University Hospital of Zurich in collaboration with others have improved the extrapleural pneumonectomy surgery and perioperative care, resulting in a substantial decrease of morbidity and mortality of the surgery and also better overall survival as part of multimodality therapy (10). However, trends in incidence, mortality and net survival of mesothelioma have never been assessed in the canton of Zurich.
The aim of the present study was to analyse incidence, mortality, and net survival of patients diagnosed with malignant pleural mesothelioma in the canton of Zurich, Switzerland. Moreover, the number of pleural mesothelioma recorded in the population-based cancer registry of the canton of Zurich was compared to the cases recognized by accident insurances. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-766/rc).
Methods
Cancer registry data
Incidence and survival were estimated using the population-based data of the cancer registry of the cantons of Zurich, Zug, Schaffhausen and Schwyz (not publicly available). However, only patients residing in the canton of Zurich at the time of diagnosis were considered, as this offers the longest time horizon since 1980. The quality of the cancer registry data was in general rated as good (11).
Patients with a primary malignant pleural mesothelioma diagnosed between 1981 and 2019 were included using the morphology codes 9050/3, 9051/3, 9052/3 or 9053/3 and the topography code C38.4 of the third edition of the International Classification of Diseases for Oncology (ICD-O-3). The year 1980 was not considered because specific population data required for standardization is only available from 1981 onward. A cancer-stage analysis was performed for the period between 2003 and 2019 because the stages were not registered systematically prior to 2003. Cases for which the diagnosis was mentioned in death certificates only (DCO) were excluded. Due to the small sample (75 cases), peritoneal mesothelioma were excluded.
Stage of disease (I, II, III, IV or “unknown”) was defined using the TNM classification of malignant tumours (TNM). Version 6 of the classification was used for the incidence years 2003 to 2009, version 7 for 2010 to 2017 and version 8 for 2018 and 2019. The clinical node stage was used when the pathological node stage was missing, and vice versa. When the pathological metastasis stage was missing, the clinical one was used, if available. If the clinical metastasis stage was missing, it was assumed to be zero. If pathological and clinical node and tumour stage were missing, they were defined as missing. When available and no neoadjuvant therapy was conducted, the pathological TNM stage was considered, otherwise the clinical TNM stage.
For our analysis, year of diagnosis was categorised into three periods: 1981–1999, 2000–2009, and 2010–2019. Stages I and II as well as stages III and IV were combined. Age was categorized into three groups: below 65 years, between 65 and 74 years, and over 74 years.
Cause of death data
To assess mortality, the canton of Zurich’s cause-of-death statistics provided by the Swiss Federal Office of Statistics was used (12). It contains data of individuals residing in the canton of Zurich at the time of their death. Until 1994, the main cause of death was defined with the eighth revision of International Classification of Diseases (ICD-8) and thereafter with the tenth revision (ICD-10). The ICD-8 code 163.0 corresponds to pleural cancer, in most cases mesothelioma [see Schüler et al. (13)]. Thus, we included patients whose main cause of death was coded as 163.0 (ICD-8) and C450 (ICD-10). We considered the same time period (1981 to 2019) as for the cancer registry data.
Accident insurance data
In Switzerland, by law all employees are compulsory insured against occupational accidents and illnesses and around 96% of registered cases get recognized as occupational illness by the accident insurances (14). For the present study, the number of recognized pleural mesothelioma cases of individuals residing in the canton of Zurich at the time of reporting to the insurance was provided by the “Collecting Agency for Accident Insurance Statistics (SSUV)”. This data, available from 1986 to 2019, allowed to compare the number of incident cases based on cancer registry data with the number of cases recognized as occupational illness.
Statistical analyses
Time trends of absolute pleural mesothelioma cases in men and women based on cancer registry data [1981–2019] and insurance data [1986–2019] were visualized using quasi-poisson regression.
Age-standardized incidence and mortality rates per 100,000 person-years were calculated using midyear population estimates and the European Standard Population of 1976 (15,16). Time trends by sex were investigated using joinpoint regression analysis. We identified the so-called joinpoints where a statistically significant change in trend appeared and estimated the annual percentage change (APC) for each regression segment.
Net survival up to 3 years after diagnosis was estimated by sex, and for men by year of diagnosis, stage, age at diagnosis and morphology using the Pohar-Perme method (17). Population life tables of the canton of Zurich were provided by the National Agency for Cancer Registration.
Joinpoint regression analyses were performed in Joinpoint Regression Program Version 4.9.0.0 (March 2021 Statistical Research and Applications Branch, United States National Cancer Institute). All other analyses were performed using R Version 4.2.0 (2022 R Foundation for Statistical Computing).
Ethics
In accordance with the Swiss law on human research, approval from an ethics committee was not required because the data were anonymized. Cancer cases within the canton of Zurich were reported to the cancer registry through presumed consent and recording based on a directive from the Zurich Government Council in 1980, and the general registry approval by the Federal Commission of Experts for professional secrecy in medical research in 1995. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Results
Cancer registry patient and tumour characteristics
In total, 798 men and 108 women were diagnosed with a primary malignant pleural mesothelioma in the canton of Zurich between 1981 and 2019. Approximately one-third were below 65 years of age at diagnosis, one-third between 65 and 74 years, and the rest over 74 years (Table 1). However, over time, the mean age at diagnosis increased from 68 years in 1981 to 75 years in 2019 (standard deviation 11 and 10 years, respectively) (Figure S1). Most cases were diagnosed on the right pleura (42.4%) and had an epithelioid morphology (48%). Between 2003 and 2019, 17.7% were diagnosed with stage I or II, 28.0% with stage III or IV, whereas stage was unknown for 54.2% of patients.
Table 1
| Variables | Overall, n (%) | Men, n (%) | Women, n (%) |
|---|---|---|---|
| Age at diagnosis (years) | |||
| <65 | 280 (30.9) | 242 (30.3) | 38 (35.2) |
| 65–74 | 299 (33.0) | 273 (34.2) | 26 (24.1) |
| ≥75 | 327 (36.1) | 283 (35.5) | 44 (40.7) |
| Year of diagnosis | |||
| 1981–1999 | 290 (32.0) | 258 (32.3) | 32 (29.6) |
| 2000–2009 | 295 (32.6) | 261 (32.7) | 34 (31.5) |
| 2010–2019 | 321 (35.4) | 279 (35.0) | 42 (38.9) |
| Laterality | |||
| Midline tumor, not a paired site | 3 (0.3) | 2 (0.3) | 1 (0.9) |
| Right | 384 (42.4) | 341 (42.7) | 43 (39.8) |
| Left | 275 (30.4) | 244 (30.6) | 31 (28.7) |
| Bilateral | 11 (1.2) | 10 (1.3) | 1 (0.9) |
| Unknown | 233 (25.7) | 201 (25.2) | 32 (29.6) |
| Morphology | |||
| Not otherwise specified | 270 (29.8) | 235 (29.4) | 35 (32.4) |
| Fibrous | 47 (5.2) | 41 (5.1) | 6 (5.6) |
| Epithelioid | 435 (48.0) | 379 (47.5) | 56 (51.9) |
| Biphasic | 154 (17.0) | 143 (17.9) | 11 (10.2) |
| Stage* | |||
| I and II | 96 (17.7) | 88 (18.6) | 8 (11.4) |
| III and IV | 152 (28.0) | 133 (28.2) | 19 (27.1) |
| Unknown | 294 (54.2) | 251 (53.2) | 43 (61.4) |
*, cancer-stage analysis was performed for the period between 2003 and 2019 because the stages were not registered systematically prior to 2003.
Comparison of cancer registry data with insurance data
Among men, the absolute number of pleural mesotheliomas based on cancer registry data increased between 1981 and 2019. The number of cases in men based on accident insurance data followed this trend, but at a lower level. However, among men the number of cases in the two data sources was similar in 2016, 2017 and 2019 (Figure 1). Among women, the absolute number of pleural mesothelioma based on cancer registry data increased slightly over the study period, while the number of cases based on accident insurance data did not change over time.

Incidence and mortality rate trends
In men, the incidence rate was increasing from 1981 to 2002 {APC: 4.7 [95% confidence interval (CI): 2.6 to 6.8]} and then decreasing until 2019 [APC: −2.3, (95% CI: −4.2 to −0.3)], while in women it was increasing over the whole period [APC: 6.2 (95% CI: −1.3 to 14.4)], although on a lower level (Figure 2A). Mortality rates were stable in men and women with no joinpoints identified (Figure 2B, Table S1). In men until 1995, mortality rates were mostly higher than incidence rates.

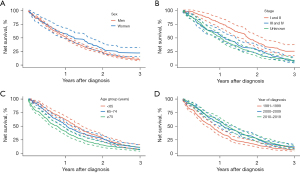
Net survival
Men with pleural mesothelioma had poorer net survival than women. One-year net survival was 51.6% (95% CI: 48.1% to 55.4%) for men and 57.8% (95% CI: 48.8% to 68.4%) for women, while three-year net survival was 9.7% (95% CI: 7.8% to 12.2%) and 22.1% (95% CI: 15.3% to 32.1%), respectively (Figure 3A, Table S2). In men, subgroup analyses revealed differences in net survival depending on stage, age and year of diagnosis. First, men with stage I or II pleural mesothelioma had a better net survival after three years than men with stage III or IV [25.4% (95% CI: 17.2% to 37.5%) and 7.4% (95% CI: 3.9% to 13.8%), respectively] (Figure 3B). Second, one year after diagnosis men below age of 65 years experienced a better net survival than men between 65 and 74 years or over 74 years, while three years after diagnosis all age groups had quite similar net survival [11.3% (95% CI: 7.9% to 16.1%), 11.1% (95% CI: 7.8% to 15.8%) and 6.9% (95% CI: 4.2% to 11.5%), respectively] (Figure 3C). Third, one year after diagnosis men diagnosed between 2010 and 2019 or 2000 and 2009 had a better net survival than men diagnosed between 1981 and 1999 but the difference narrowed at three years after diagnosis [10.1% (95% CI: 6.8% to 15.0%), 12.1% (95% CI: 8.7% to 17.1%) and 6.6% (95% CI: 4.0% to 10.7%), respectively] (Figure 3D). The improved one-year survival over time is likely due to advancements in treatment like multimodality therapy. In women, due to the small number of cases, no subgroup analysis was conducted.
Discussion
In men, the incidence rate of malignant pleural mesothelioma has been increasing until 2002 and then decreasing, while in women it has been increasing over the whole period. The gap between the number of pleural mesotheliomas recognized by the accident insurance and the number of diagnosed cases registered in the cancer registry has narrowed in more recent years. Mortality rates were stable over time and net survival was poor in men and women, although slightly higher in women.
Comparison with other studies
Incidence and mortality
The number of pleural mesotheliomas among men, recognized by accident insurances, has equalled the count documented by the cancer registry in 2016, 2017 and 2019, indicating a recent increase in cases that were reported to and recognized by the accident insurances. This trend was also observed by another study examining various data sources of malignant pleural mesothelioma in Switzerland. They noted an alignment in the figures between accident insurers and cause of death statistics from 2001 to 2019 (9).
In line with other studies, we found lower incidence rate of mesothelioma in women than in men (5,18-20). Historical differences in occupational asbestos exposure explain that disparity between the sexes (5). Although the incidence in women has increased over the whole period (average APC 6.2, 95% CI: −1.3 to 14.4), it is not statistically significant. This rise might be due to non-occupational asbestos exposure which based on an Australian study (21) affects men and women nearly equally, unlike occupational exposure, which affects only 1% of women. To prevent further increases in women, measures targeting non-occupational asbestos exposure are crucial.
The Nordic countries Denmark, Norway and Sweden took earlier measures than Switzerland by banning all or almost all asbestos products between 1984 and 1986. Finland followed shortly after in 1992 (22-24). The age-standardized incidence trends for men in these countries are similar to our findings. In Denmark, the highest incidence of malignant pleural mesothelioma in men was observed in 1997, in Norway in 2003, in Sweden in the early 1990s and in Finland in 2006 (25). Contrary to these countries, we found higher incidence and mortality rates, but the Nordic countries also observed regional differences. As expected, in Denmark, Norway and Finland mortality trends in men followed the incidence trends (25). Trends in pleural mesothelioma mortality are expected to mirror the trends in incidence over the same period because most patients have a short expected survival time following diagnosis (i.e., survival is poor). The Nordic countries observed this pattern, but the difference between incidence and mortality varied over time (25). In contrast, in the canton of Zurich, the mortality rate in men did not follow the incidence rate, but remained stable. While in men the stable mortality rate during the increase in incidence rate may be due to improved survival (see Figure 3D net survival by year of diagnosis), the stable mortality rate during the decrease in incidence rate cannot be explained by survival, however, migration and changes in the coding of death might play a role. In Switzerland, there were many foreign construction workers potentially exposed to asbestos and they might have returned to their country of origin before diagnosis and came back after diagnosis due to the high-quality treatment. After diagnosis it is unlikely that patients moved away due to high quality treatments available in Zurich and short survival times. Furthermore, until 1994 the ICD-8 code used for the death statistics included not only pleural mesothelioma but also other malignant cancers of the pleura. Mortality trends are based on death certificates that are rarely validated against any clinical or pathological information (26). This might also account for the higher mortality rates compared to incidence rates in men for the majority of years before 1995. An Italian study by Montanaro et al. (27) also emphasized that changes in the coding of death over time could have a substantial impact on mesothelioma mortality trends. However, they reported that between 1980–1986, the cancer registry of Zurich observed a good concordance between pathological diagnosis and death certification, since the 20% false positives offset each other (27). Anyway, the time trends reported in the present study need to be interpreted with caution as the number of cases was small.
The most recent European standardized incidence rates for Europe are published by the RAREcarenet Study for the years 2000 to 2007 (28). Based on that study, which overall included 94 European population-based cancer registries, the European standardized age-adjusted incidence rate per 100,000 person-years for mesothelioma of pleural and pericardium was 2.65 for men and 0.45 for women. Of note only 1–2% of mesothelioma originate from the pericardium (29). However, in men the incidence rate of mesothelioma of pleural and pericardium in Europe is lower than the rate of pleural alone that we computed for the canton of Zurich, while in women the incidence rates are similar. This is not surprising as the incidence rate of pleural mesothelioma in the canton of Zurich was observed to be among the highest in Switzerland between 1996–2015 (30). Asbestos is found in certain rocks in Switzerland, but large-scale extractions occurred only in the canton of Graubünden between 1907 and 1911 (31,32). The asbestos ban in 1990 prevented new imports and usage in Switzerland. However, about 500,000 tons introduced earlier are still present, mainly in buildings as only a small portion has been removed. Approximately two-thirds of residential buildings in Switzerland were built before 1990 and therefore potentially contain asbestos, posing risk to workers during maintenance, renovation, and demolition if not handled properly (31). The canton of Zurich is the most populous canton of Switzerland.
Of note, the incidence peak can vary by age and other factors. Australia, with one of the highest age-standardised incidence rates, reached its overall peak in the 2000s but shows variations by age, gender, and tumour location. For instance, the peak for men aged 75 years or older and for women was expected around 2020 (21,33).
Survival
In accordance with other studies, we observed better survival in women than in men (5,18-20). This might be due to lower exposure to asbestos, the protective effects of oestrogen and/or beneficial clinical characteristics (5). For instance, a retrospective study with 24 women in Northern Jutland, Denmark, observed that almost half of women with malignant pleural mesothelioma were exposed to asbestos at home through their husbands or sons and only 12.5% were primarily exposed to asbestos (34). Indeed also other studies show that women are mainly exposed to asbestos through environmental and domestic sources (35,36). Environmental exposure can result from living near an asbestos-emitting site or in an area contaminated by airborne asbestos due to heavy asbestos industry. Often multiple sources of exposure such as environmental and domestic (living with an asbestos worker) occur (35). Visonà et al. (37) found higher concentrations of inorganic fibers, asbestos fibers and asbestos bodies in women with environmental and domestic exposures compared to those with only environmental exposure. Kitamura et al. (38) observed a dose-dependent increase in mesothelioma death risk associated with neighbourhood exposure. The morphology of mesothelioma is also known to have an impact on survival. In the present study, the frequency of epithelioid morphology is similar for women and men but in women, mesothelioma with epithelioid morphology responds better to treatment leading to higher survival (39).
However, the one-year net survival in the present study surpassed the relative survival reported in other studies (19,20,40). Conversely, the three-year net survival for men aligned with findings from other studies, while in women, it exceeded the rates observed in other studies (40). Consistent with trends observed in Nordic countries, one year survival in men improved over time (25,40). In the RAREcarenet Study, for Europe one-year relative survival of mesothelioma of pleura and pericardium was estimated to be 39% for men and 42% for women and three-year relative survival to be 8% for men and 12% for women (28). This indicates that in the canton of Zurich, one-year survival was higher than in Europe. However, the three-year survival rate among men in the canton of Zurich was similar to that of Europe, whereas among women, it was higher than the European rate. To our knowledge, we provide the first net survival estimates for pleural mesothelioma using the method by Perme (17). Therefore, comparability with other studies that used relative survival methods such as Ederer and Hakulinen is limited. Furthermore, the number of women diagnosed with pleural mesothelioma included in the study was very small and therefore their results need to be interpreted with caution.
Conclusions
The early national ban of asbestos in Switzerland seems to have been effective based on the incidence and mortality estimates we calculated for pleural mesothelioma in the canton of Zurich. However, even though the malignant pleural mesothelioma incidence rate is decreasing in recent years, it is still on a high level compared to other countries and survival remains poor. People can still get exposed to asbestos despite the ban. Therefore, awareness and prevention of asbestos exposure should be enhanced, and further research is needed to improve diagnosis and expand treatment options, in order to prolong the survival of pleural mesothelioma patients.
Acknowledgments
The authors thank Matthias Lorez from the National Agency for Cancer Registration for providing the population life tables of the canton of Zurich and Stefan Scholz from the Collecting Agency for Accident Insurance Statistics for providing the accident insurance data.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-766/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-766/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-766/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-766/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Cancer cases in the Canton of Zurich are registered with presumed consent and registration based on a decision by the Zurich Government Council from 1980 and the general registry approval by the Federal Commission of Experts for professional secrecy in medical research from 1995. All data were used anonymously in this analysis, and no approval from the Ethical Committee of the Canton of Zurich was necessary. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Disclaimer: At the time of publication, Dr. Karavasiloglou is an European Food Safety Authority (EFSA) staff member. At the time of preparation of this work, Dr. Karavasiloglou was affiliated with the University of Zurich and the University Hospital Zurich. The views expressed in this publication are those of the authors and should not be interpreted as representing the official position of the European Food Safety Authority (EFSA). Therefore, the present article is published under the sole responsibility of the authors, and may not be considered as an EFSA scientific output. EFSA cannot be held accountable for any errors or inaccuracies that may appear.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schumann SO, Kocher G, Minervini F. Epidemiology, diagnosis and treatment of the malignant pleural mesothelioma, a narrative review of literature. J Thorac Dis 2021;13:2510-23. [Crossref] [PubMed]
- Opitz I. Management of malignant pleural mesothelioma-The European experience. J Thorac Dis 2014;6:S238-52. [PubMed]
- Järvholm B, Burdorf A. Asbestos and disease - a public health success story? Scand J Work Environ Health 2024;50:53-60. [Crossref] [PubMed]
- Thives LP, Ghisi E, Thives Júnior JJ, et al. Is asbestos still a problem in the world? A current review. J Environ Manage 2022;319:115716. [Crossref] [PubMed]
- Alpert N, van Gerwen M, Taioli E. Epidemiology of mesothelioma in the 21(st) century in Europe and the United States, 40 years after restricted/banned asbestos use. Transl Lung Cancer Res 2020;9:S28-38. [Crossref] [PubMed]
- The Global Cancer Observatory. Mesothelioma fact sheet (Internet). International Agency for Research on Caner. World Health Organization; 2020 Dec (cited 2023 Aug 11). Available online: https://gco.iarc.fr/today/data/factsheets/cancers/18-Mesothelioma-fact-sheet.pdf
- Allen LP, Baez J, Stern MEC, et al. Trends and the Economic Effect of Asbestos Bans and Decline in Asbestos Consumption and Production Worldwide. Int J Environ Res Public Health 2018;15:531. [Crossref] [PubMed]
- Jost M, Pletscher C. Berufskrankheiten (Internet). Suva Abteilung Arbeitsmedizin; 2013 Mar (cited 2023 Aug 18). Available online: https://www.ressourcenplus.ch/wp-content/uploads/sites/177/2020/06/factsheet-berufskrankheiten_suva.pdf
- Beeler PE, Meier SL, Bopp M, Dressel H. Datenquellen zur Häufigkeit des malignen Pleuramesothelioms in der Schweiz seit 2001. ASU Arbeitsmedizin Sozialmedizin Umweltmed 2021;2021:567-73. [Crossref]
- Bueno R, Opitz I, Mesothelioma Taskforce IASLC. Surgery in Malignant Pleural Mesothelioma. J Thorac Oncol 2018;13:1638-54. [Crossref] [PubMed]
- Wanner M, Matthes KL, Korol D, et al. Indicators of Data Quality at the Cancer Registry Zurich and Zug in Switzerland. Biomed Res Int 2018;2018:7656197. [Crossref] [PubMed]
- Swiss federal office of statistics. Specific causes of death (Internet). (cited 2023 Aug 16). Available online: https://www.bfs.admin.ch/bfs/en/home/statistics/health/state-health/mortality-causes-death/specific.html
- Schüler G, Bopp M. Atlas der Krebsmortalität in der Schweiz 1970-1990. Band D. Birkhäuser Verlag; 1997.
- Statistik der Unfallversicherung UVG. Schlüsselzahlen (Internet). 2021 (cited 2023 Aug 16). Available online: https://www.unfallstatistik.ch/d/einf/schluesselzahlen_d.htm
- Boyle P, Parkin DM. Cancer registration: principles and methods. Statistical methods for registries. IARC Sci Publ 1991;126-58. [PubMed]
- Waterhouse J, Correa P, Muir C, et al. Cancer Incidence in Five Continents Volume III (Internet). Lyon: IARC Scientific Publication No. 15; 1976 (cited 2023 Aug 16). Available online: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Scientific-Publications/Cancer-Incidence-In-Five-Continents-Volume-III-1976
- Perme MP, Stare J, Estève J. On estimation in relative survival. Biometrics 2012;68:113-20. [Crossref] [PubMed]
- Sirri E, Kieschke J, Vohmann C, et al. Survival of malignant mesothelioma and other rare thoracic cancers in Germany and the United States: A population-based study. Int J Cancer 2020;147:1548-58. [Crossref] [PubMed]
- Soeberg MJ, Creighton N, Currow DC, et al. Patterns in the incidence, mortality and survival of malignant pleural and peritoneal mesothelioma, New South Wales, 1972-2009. Aust N Z J Public Health 2016;40:255-62. [Crossref] [PubMed]
- Mak V, Davies E, Putcha V, et al. The epidemiology and treatment of mesothelioma in South East England 1985-2002. Thorax 2008;63:160-6. [Crossref] [PubMed]
- Soeberg M, Vallance DA, Keena V, et al. Australia's Ongoing Legacy of Asbestos: Significant Challenges Remain Even after the Complete Banning of Asbestos Almost Fifteen Years Ago. Int J Environ Res Public Health 2018;15:384. [Crossref] [PubMed]
- Fonseca AS, Jørgensen AK, Larsen BX, et al. Historical Asbestos Measurements in Denmark-A National Database. Int J Environ Res Public Health 2022;19:643. [Crossref] [PubMed]
- European Forum, Eurogip. Asbestos-related occupational diseases in Europe (Internet). 2006 Apr (cited 2024 Jan 19). Available online: https://www.eurogip.fr/images/publications/EUROGIP-24E-AsbestosOccDiseases.pdf
- Kazan-Allen L. International Ban Asbestos Secretariat. 2023 (cited 2024 Jan 19). Chronology of Asbestos Bans and Restrictions. Available online: http://www.ibasecretariat.org/chron_ban_list.php
- Hemminki K, Försti A, Chen T, et al. Incidence, mortality and survival in malignant pleural mesothelioma before and after asbestos in Denmark, Finland, Norway and Sweden. BMC Cancer 2021;21:1189. [Crossref] [PubMed]
- Ellis L, Woods LM, Estève J, et al. Cancer incidence, survival and mortality: explaining the concepts. Int J Cancer 2014;135:1774-82. [Crossref] [PubMed]
- Montanaro F, Bray F, Gennaro V, et al. Pleural mesothelioma incidence in Europe: evidence of some deceleration in the increasing trends. Cancer Causes Control 2003;14:791-803. [Crossref] [PubMed]
- National Cancer Institute of Italy. RARECAREnet Study - Online Analysis (Internet). (cited 2023 Dec 15). Available online: http://rarecarenet.istitutotumori.mi.it
- Bridda A, Padoan I, Mencarelli R, et al. Peritoneal mesothelioma: a review. MedGenMed 2007;9:32. [PubMed]
- Locher BN, Barresi F, Kuhn BK, et al. Occupations and geographical distribution of mesothelioma in Switzerland 1989–2018 – record linkage of an asbestos-exposed population with the Swiss National Cohort. Swiss Med Wkly 2022;152:w30164. [Crossref] [PubMed]
- Federal Coordination Commission for Occupational Safety. Asbest Gefährlicher Baustoff. Luzern: Federal Coordination Commission for Occupational Safety FCOS; 2023 Apr. (EKAS Mitteilungsblatt). Report No.: 96.
- Federal Office of Public Health. Asbest (Internet). (cited 2024 Jul 14). Available online: https://www.bag.admin.ch/bag/de/home/gesund-leben/umwelt-und-gesundheit/chemikalien/chemikalien-a-z/asbest.html
- Soeberg MJ, Leigh J, Driscoll T, et al. Incidence and survival trends for malignant pleural and peritoneal mesothelioma, Australia, 1982-2009. Occup Environ Med 2016;73:187-94. [Crossref] [PubMed]
- Langhoff MD, Kragh-Thomsen MB, Stanislaus S, et al. Almost half of women with malignant mesothelioma were exposed to asbestos at home through their husbands or sons. Dan Med J 2014;61:A4902. [PubMed]
- Tlotleng N, Sidwell Wilson K, Naicker N, et al. The significance of non-occupational asbestos exposure in women with mesothelioma. Respirol Case Rep 2018;7:e00386. [Crossref] [PubMed]
- Panou V, Vyberg M, Meristoudis C, et al. Non-occupational exposure to asbestos is the main cause of malignant mesothelioma in women in North Jutland, Denmark. Scand J Work Environ Health 2019;45:82-9. [Crossref] [PubMed]
- Visonà SD, Capella S, Borrelli P, et al. Asbestos burden in lungs of non-occupationally exposed women from Broni (Pavia, Italy): a postmortem SEM-EDS study. J Thorac Dis 2023;15:6555-69. [Crossref] [PubMed]
- Kitamura Y, Zha L, Liu R, et al. Association of mesothelioma deaths with neighborhood asbestos exposure due to a large-scale asbestos-cement plant. Cancer Sci 2023;114:2973-85. [Crossref] [PubMed]
- Lapidot M, Mazzola E, Bueno R. Prolonged survival and novel prognostic factors in women with pleural mesothelioma treated with extended pleurectomy decortication. Transl Lung Cancer Res 2024;13:811-20. [Crossref] [PubMed]
- Helland Å, Solberg S, Brustugun OT. Incidence and survival of malignant pleural mesothelioma in norway: a population-based study of 1686 cases. J Thorac Oncol 2012;7:1858-61. [Crossref] [PubMed]


