
Accuracy of lung structure constructed by three-dimensional image analysis with non-enhanced computed tomography
Highlight box
Key findings
• The three-dimensional (3D) images of the lungs based on non-enhanced computed tomography (CT) accurately depicted blood vessels and bronchus in specific lung lobes.
What is known and what is new?
• It has been reported that the 3D images based on contrast-enhanced CT depict lung structures relatively accurately.
• This study showed that the 3D images of the lungs based on non-enhanced CT showed that the right middle lobe and both lower lobes were correctly depicted.
What is the implication, and what should change now?
• This study showed that 3D images based on non-enhanced CT are accurate in specific lobes.
• Further technological advances are needed to depict blood vessels and bronchus in all lung lobes.
Introduction
Background
Multi-detector computed tomography (CT) can construct three-dimensional (3D) images, which are useful in various medical fields (1-3). In thoracic surgery, several studies have reported the superiority of video-assisted thoracic surgery (VATS) and robot-assisted thoracoscopic surgery (RATS), which are less invasive compared to thoracotomy, and the number of procedures performed is increasing (4-6). Although these techniques allow for a magnified view, a wide field of view is difficult to obtain, which may lead to anatomical misidentification. Segmentectomy is expected to increase in the future, as its utility has been demonstrated in several large randomized controlled trials (7,8). Segmentectomy requires more detailed anatomic awareness than lobectomy. Fluorescence visualization using indocyanine green is utilized worldwide for improved visualization of the intersegmental plane in segmentectomy (9,10). In this situation, it is important to understand the accurate anatomical features before surgery.
Rationale and knowledge gap
The importance of 3D images that allow detailed anatomical recognition has been reported by several studies (10-17). However, these studies used 3D images based on contrast-enhanced CT. Contrast agents are considered high-risk for patients with renal dysfunction and bronchial asthma (18,19). Further, contrast agent allergy can occur even in healthy individuals (20). If non-enhanced CT could produce clear 3D images, it would allow for safe surgery while reducing the burden on the patient. Moreover, the aging society worldwide has also increased the number of patients with limited renal function capacity.
Objective
The aim of this study was to investigate the accuracy of 3D images of the lungs constructed from non-enhanced CT using the latest image analysis systems. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1406/rc).
Methods
Patients
Of the patients who underwent lobectomy or segmentectomy at Nagoya University Hospital, 10 consecutive cases in each lung lobe were collected for a total of 50 cases between March and December 2022. The patients underwent both non-enhanced and contrast-enhanced CTs 2 months before surgery, and all the actual anatomical details were available on video during surgery. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Nagoya University Graduate School of Medicine (No. 2020-0525: February 8, 2021) and individual consent for this retrospective analysis was waived due to the retrospective nature.
Database
We used the following clinical and pathological characteristics in our database: age, sex, smoking history, pathological type, surgical approach, surgical procedure, operation time, intraoperative blood loss, 90-day mortality, postoperative complications based on the Clavien-Dindo classification, and description of postoperative adjuvant therapy. Postoperative complications that occurred within 90 days of surgery were recorded using the Clavien-Dindo system (21).
3D image construction
CT imaging was performed with a 64-channel multi-detector CT (Toshiba Medical Systems Corp., Tokyo, Japan) with a 1-mm thickness of the entire lung. All patients underwent non-enhanced CT followed by contrast-enhanced CT in the equilibrium phase after injecting the contrast agent. We used the Synapse Vincent System ver. 6.8 (Fujifilm Corporation, Tokyo, Japan) to obtain 3D images of the pulmonary vessels and the tracheobronchial tree. The system used the novel deep learning algorithm based on anatomical recognition and sequential recognition, not only differences in CT values, and automatically generated 3D images based on both the non-enhanced and contrast-enhanced CT images. The quality of all CT images was good enough to delineate the subsegmental branches. The generated images did not undergo any human modification.
Analysis
First, we compared the non-enhanced CT-based and contrast-enhanced CT-based 3D images to validate their differences. Second, we evaluated accuracy by comparing these images to the actual surgical findings. Two surgeons (O.N. and T.F.C.Y.) interpreted the 3D images of the pulmonary artery (PA), pulmonary vein (PV), and bronchus (Br) branching patterns. Two other surgeons (T.K. and S.N.) evaluated the actual intraoperative video of anatomical findings postoperatively. In comparing non-contrast CT-based and contrast-enhanced CT-based 3D images, we evaluated PA, PV, and Br greater than 2 mm in diameter. Further, in surgical findings, we decided that PA, PV, and Br require evaluation up to the segmental-level. The cases that could not be identified to segmental level, such as Br in lobectomy, were evaluated at the lobar-level. We counted the number of branches that matched PA, PV, and Br.
Results
The patient characteristics are shown in Table S1. The median age was 74 years, and 35 patients (70%) were male. Further, 47 patients (94%) had primary lung cancer, the most frequently performed surgical approach was RATS, and 47 patients (94%) underwent lobectomy. The median operative time was 171 minutes, and the median intraoperative blood loss was 11 mL. No postoperative complications were reported with grade ≥3 and 90-day mortality.
Figure 1 shows the representative images in which 3D images based on non-enhanced CT and those based on contrast-enhanced CT were well matched, whereas Figure 2 shows unmatched representative images. Compared to contrast-enhanced CT, 3D images based on non-enhanced CT were equally distinct, with clearly recognizable structures. Table 1 compares the coincidence and discrepancy rates between non-enhanced and contrast-enhanced CT-based 3D images when divided into the right and left lungs. The coincidence rate in the right lung was 70%, and that in the left lung was 65%, which was almost equal. As shown in Figure 2, all cases of discrepancy were either due to the PA or PV being incorrectly depicted on the other, whereas the Br was consistent in all cases.
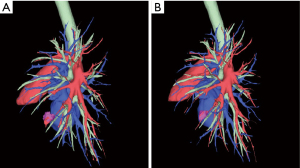
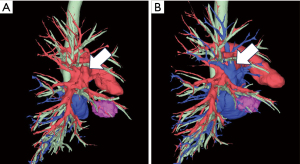
Table 1
| Location | N | Coincidence, n [%] | Discrepancy, n [%] |
|---|---|---|---|
| Right lung | 30 | 21 [70] | 9 [30] |
| Left lung | 20 | 13 [65] | 7 [35] |
3D, three-dimensional; CT, computed tomography.
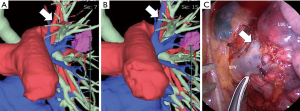
Next, we compared the actual surgical findings with the non-enhanced and contrast-enhanced CT-based 3D images to evaluate accuracy. Figure 3A-3C shows the representative images in which 3D findings based on non-enhanced CT and those based on contrast-enhanced CT were both consistent with the intraoperative findings. Conversely, Figure 3D-3F shows the representative images in which 3D findings based on non-enhanced CT and those based on contrast CT did not match the intraoperative findings. Furthermore, Figure 4 shows representative images in which 3D findings based on non-enhanced CT were inconsistent, whereas those based on contrast CT were consistent with the intraoperative findings. The number of coincidence branches between 3D imaging based on non-enhanced CT and surgical findings in each lobe.

In each case, we counted the number of PA, PV, and Br that could be confirmed by surgical findings. For example, in one case of right upper lobectomy, if the surgical findings showed the pulmonary trunk, A2b, V1, central vein, and right upper lobe Br, we counted PA: n=2, PV: n=2, Br: n=1. Also, we counted the number of branches that matched the 3D images based on non-enhanced CT and the surgical findings. The number of branches actually present in the surgical findings (total branches) and the number of branches correctly depicted in the non-enhanced CT-based 3D images (coincidence branches) were calculated as the sum of ten cases in each lobe (Table 2). In the right middle, right lower, and left lower lobe, PA, PV, and Br were correctly delineated in all cases. Conversely, in the right upper lobe, the coincidence rate for the PA was 97%, and that for PV was 74%, indicating the incorrect delineation of PV in many cases. In the left upper lobe of the lungs, the coincidence rate for PA was 100%, while that for PV was low at 87%.
Table 2
| Location | PA | PV | Br | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CB | TB | % (CB/TB) | CB | TB | % (CB/TB) | CB | TB | % (CB/TB) | |||
| Right upper lobe | 31 | 32 | 97 | 17 | 23 | 74 | 10 | 10 | 100 | ||
| Right middle lobe | 18 | 18 | 100 | 10 | 10 | 100 | 10 | 10 | 100 | ||
| Right lower lobe | 20 | 20 | 100 | 20 | 20 | 100 | 11 | 11 | 100 | ||
| Left upper lobe | 46 | 46 | 100 | 26 | 30 | 87 | 10 | 10 | 100 | ||
| Left lower lobe | 22 | 22 | 100 | 20 | 20 | 100 | 12 | 12 | 100 | ||
3D, three-dimensional; CT, computed tomography; PA, pulmonary artery; PV, pulmonary vein; Br, bronchus; CB, coincidence branches; TB, total branches.
Similarly, Table 3 shows the coincidence branches of 3D images based on contrast-enhanced CT in each lobe. In the right middle, right lower, and left lower lobes, the 3D images matched the surgical findings in all cases. In the right upper lobe, the coincidence rate for the PA was 97%, and that for PV was 87%. Also, in the left upper lobe, the coincidence rate for the PA was 100%, and that for PV was 97%.
Table 3
| Location | PA | PV | Br | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CB | TB | % (CB/TB) | CB | TB | % (CB/TB) | CB | TB | % (CB/TB) | |||
| Right upper lobe | 31 | 32 | 97 | 20 | 23 | 87 | 10 | 10 | 100 | ||
| Right middle lobe | 18 | 18 | 100 | 10 | 10 | 100 | 10 | 10 | 100 | ||
| Right lower lobe | 20 | 20 | 100 | 20 | 20 | 100 | 11 | 11 | 100 | ||
| Left upper lobe | 46 | 46 | 100 | 29 | 30 | 97 | 10 | 10 | 100 | ||
| Left lower lobe | 22 | 22 | 100 | 20 | 20 | 100 | 12 | 12 | 100 | ||
3D, three-dimensional; CT, computed tomography; PA, pulmonary artery; PV, pulmonary vein; Br, bronchus; CB, coincidence branches; TB, total branches.
Table 4 shows the details of cases in which the 3D images did not match the surgical findings. All cases with poor delineation on contrast-enhanced CT were also poorly delineated on non-contrast CT. PA was poorly delineated in only one case, whereas PV was poorly delineated in all cases. The pattern of poor visualization was similar, with PV misidentified as PA.
Table 4
| Case | Location | Non-enhanced CT | Enhanced CT |
|---|---|---|---|
| 1 | RUL | V1, V2 poor drawing | Coincidence |
| 2 | RUL | V1 poor drawing | V1 poor drawing |
| 3 | RUL | V2 poor drawing | Coincidence |
| 4 | RUL | V2 poor drawing | V2 poor drawing |
| 5 | RUL | A2b, V2 poor drawing | A2b, V2 poor drawing |
| 6 | LUL | V1 poor drawing | Coincidence |
| 7 | LUL | V1 poor drawing | Coincidence |
| 8 | LUL | V1 poor drawing | V1 poor drawing |
| 9 | LUL | V2 poor drawing | Coincidence |
3D, three-dimensional; CT, computed tomography; RUL, right upper lobe; LUL, left upper lobe.
Discussion
This study showed that 3D images based on non-enhanced CT are accurate in specific lobe. There have been previous reports on the usefulness of 3D images based on non-enhanced CT in a limited number of cases (22,23). However, to our knowledge, this study is the first report to analyze each lung lobe separately and to show that the results are different for each.
In this study, we compared non-enhanced CT-based 3D images with contrast-enhanced CT-based 3D images. Among the cases in which both 3D images were matched, there were cases in which both were incorrectly delineated. Therefore, we compared these 3D images with the actual surgical findings to evaluate accuracy. The coincidence rates between 3D images based on non-enhanced CT and surgical findings in the right middle, right lower, and left lower lobes were high at 100%, while the coincidence rate for pulmonary vessels in the right upper and left upper lobes was low. Because Synapse Vincent uses anatomical recognition and sequential recognition, it is presumed that the pulmonary vessels can be accurately depicted in cases which their running is clearly different. Therefore, in the right middle and bilateral lower lobes of the lungs, PA and PV are nearly orthogonal to each other, which may have contributed to their accurate classification. However, in the bilateral upper lobes, the running of PA and PV are similar, possibly contributing to their misidentification. In a comparison of 3D images based on contrast-enhanced CT and intraoperative findings, the left upper lobe of the lung had a high coincidence rate of 90%, while that of the right upper lobe was 70%. Poor delineation of the right upper lobe of the lung on contrast-enhanced CT was also reported by Hagiwara (12). The right upper lobe of the lung is probably a systemically difficult structure to delineate, even when based on contrast-enhanced CT.
All poor delineation cases in this study were due to the misidentification of PV as PA. In other words, vessels were correctly recognized and depicted as blood vessels even in images based on non-enhanced CT, and the image quality was not inferior to that of contrast-enhanced CT. From the surgeon’s point of view, the misrecognition was evident and easily modifiable. In this software, manual modification is possible; therefore, the 3D imaging based on non-enhanced CT is considered sufficiently available for clinical use, and will become more useful with increased accuracy after eliminating the need for human modification.
The limitations of this study were its retrospective nature, inducing bias, and small sample size. Because this study showed that 3D images based on non-contrast CT might be useful, prospective, larger scale studies are needed for properly evaluating this 3D software.
Conclusions
3D images based on non-contrast CT have the potential to accurately depict lung blood vessels and bronchi. However, further technological advances are needed to depict lung structures correctly in all lung lobes.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1406/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1406/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1406/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-1406/coif). All authors report Fujifilm provided software to create 3D images. T.F.C.Y., Y.K., and S.N. conducted sponsored research with Fujifilm in this study. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Nagoya University Graduate School of Medicine (No. 2020-0525: February 8, 2021) and individual consent for this retrospective analysis was waived due to the retrospective nature.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yamanaka J, Saito S, Iimuro Y, et al. The impact of 3-D virtual hepatectomy simulation in living-donor liver transplantation. J Hepatobiliary Pancreat Surg 2006;13:363-9. [Crossref] [PubMed]
- Mochizuki K, Takatsuki M, Soyama A, et al. The usefulness of a high-speed 3D-image analysis system in pediatric living donor liver transplantation. Ann Transplant 2012;17:31-4. [Crossref] [PubMed]
- Olaiya OR, Nadeem I, Horner NS, et al. Templating in shoulder arthroplasty - A comparison of 2D CT to 3D CT planning software: A systematic review. Shoulder Elbow 2020;12:303-14. [Crossref] [PubMed]
- Wang BY, Huang JY, Lin CH, et al. Thoracoscopic Lobectomy Produces Long-Term Survival Similar to That with Open Lobectomy in Cases of Non-Small Cell Lung Carcinoma: A Propensity-Matched Analysis Using a Population-Based Cancer Registry. J Thorac Oncol 2016;11:1326-34. [Crossref] [PubMed]
- Zhang Y, Chen C, Hu J, et al. Early outcomes of robotic versus thoracoscopic segmentectomy for early-stage lung cancer: A multi-institutional propensity score-matched analysis. J Thorac Cardiovasc Surg 2020;160:1363-72. [Crossref] [PubMed]
- Chen-Yoshikawa TF, Fukui T, Nakamura S, et al. Current trends in thoracic surgery. Nagoya J Med Sci 2020;82:161-74. [PubMed]
- Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022;399:1607-17. [Crossref] [PubMed]
- Altorki N, Wang X, Kozono D, et al. Lobar or Sublobar Resection for Peripheral Stage IA Non-Small-Cell Lung Cancer. N Engl J Med 2023;388:489-98. [Crossref] [PubMed]
- Nakamura S, Goto M, Chen-Yoshikawa TF. Fluorescence-guided thoracic surgery. J Vis Surg 2021;7:18. [Crossref]
- Ng CS, Ong BH, Chao YK, et al. Use of Indocyanine Green Fluorescence Imaging in Thoracic and Esophageal Surgery. Ann Thorac Surg 2023;115:1068-76. [Crossref] [PubMed]
- Saji H, Inoue T, Kato Y, et al. Virtual segmentectomy based on high-quality three-dimensional lung modelling from computed tomography images. Interact Cardiovasc Thorac Surg 2013;17:227-32. [Crossref] [PubMed]
- Hagiwara M, Shimada Y, Kato Y, et al. High-quality 3-dimensional image simulation for pulmonary lobectomy and segmentectomy: results of preoperative assessment of pulmonary vessels and short-term surgical outcomes in consecutive patients undergoing video-assisted thoracic surgery†. Eur J Cardiothorac Surg 2014;46:e120-6. [Crossref] [PubMed]
- Sekine Y, Itoh T, Toyoda T, et al. Precise Anatomical Sublobar Resection Using a 3D Medical Image Analyzer and Fluorescence-Guided Surgery With Transbronchial Instillation of Indocyanine Green. Semin Thorac Cardiovasc Surg 2019;31:595-602. [Crossref] [PubMed]
- Sardari Nia P, Olsthoorn JR, Heuts S, et al. Interactive 3D Reconstruction of Pulmonary Anatomy for Preoperative Planning, Virtual Simulation, and Intraoperative Guiding in Video-Assisted Thoracoscopic Lung Surgery. Innovations (Phila) 2019;14:17-26. [Crossref] [PubMed]
- Chen-Yoshikawa TF, Date H. Update on three-dimensional image reconstruction for preoperative simulation in thoracic surgery. J Thorac Dis 2016;8:S295-301. [PubMed]
- Sarsam M, Glorion M, de Wolf J, et al. The role of three-dimensional reconstructions in understanding the intersegmental plane: an anatomical study of segment 6. Eur J Cardiothorac Surg 2020;58:763-7. [Crossref] [PubMed]
- Tokuno J, Chen-Yoshikawa TF, Nakao M, et al. Resection Process Map: A novel dynamic simulation system for pulmonary resection. J Thorac Cardiovasc Surg 2020;159:1130-8. [Crossref] [PubMed]
- Parfrey PS, Griffiths SM, Barrett BJ, et al. Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both. A prospective controlled study. N Engl J Med 1989;320:143-9. [Crossref] [PubMed]
- Beckett KR, Moriarity AK, Langer JM. Safe Use of Contrast Media: What the Radiologist Needs to Know. Radiographics 2015;35:1738-50. [Crossref] [PubMed]
- Turner PJ, Jerschow E, Umasunthar T, et al. Fatal Anaphylaxis: Mortality Rate and Risk Factors. J Allergy Clin Immunol Pract 2017;5:1169-78. [Crossref] [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Nakao M, Omura K, Hashimoto K, et al. Three-dimensional image simulation for lung segmentectomy from unenhanced computed tomography data. Gen Thorac Cardiovasc Surg 2022;70:312-4. [Crossref] [PubMed]
- Nakazawa S, Hanawa R, Nagashima T, et al. Segmentectomy Guided by 3-Dimensional Images Reconstructed From Nonenhanced Computed Tomographic Data. Ann Thorac Surg 2021;111:e301-4. [Crossref] [PubMed]


