Transoral endoscopic mediastinal surgery (TOEMS)—results of a first clinical study for scarless mediastinal lymph node biopsies
Introduction
Mediastinal lymphadenopathy is commonly found in various diseases. The most frequent cause for mediastinal lymphadenopathy is lung cancer. In a large retrospective study with 2,145 patients evaluated for mediastinal lymphadenopathy, 68.0% were diagnosed with lung cancer. Other reasons were metastatic disease other than from lung cancer (3.6%), lymphoma (2.4%), or benign diseases (26%) (1). Today, a number of different surgical and non-invasive procedures exist to assess mediastinal lymphadenopathy. Cervical mediastinoscopy was one of the earliest surgical procedures, which was introduced by Carlens in 1959 (2). At that time, the procedure was performed without video support, also known as conventional mediastinoscopy. In 1994 visualization by video technology was introduced, known as video-assisted mediastinoscopy (VAM). Meanwhile, a number of studies exists comparing conventional and VAM. Albeit handling and teaching seems to be better for VAM, no difference in the negative predictive value and in the accuracy for the detection of lymph node metastases from lung cancer was found as reported by a recent meta-analysis (3).
Conventional and VAM are usually applied to take lymph node biopsies. To perform a complete removal of mediastinal lymph nodes, two additional methods were developed. Whereas video-assisted mediastinal lymphadenectomy (VAMLA) is an extended procedure of VAM, it allows no access to the lymph nodes of the aortopulmonary window (4). Access to the aortopulmonary window is instead provided by transcervical extended mediastinal lymphadenectomy (TEMLA), which is performed as a mixture of open and mediastinoscopic surgery (5,6). Both methods have a much higher probability to detect mediastinal lymph node metastases compared to conventional mediastinoscopy or VAM (4,7,8). However, the extended procedures are accompanied with a higher rate of complications, which is the reason that their use is currently recommended only for experienced centres and clinical studies (9).
All surgical procedures described above gain access to the mediastinum through an incision at the anterior neck at the collar line. Especially younger patients might be disturbed by the remaining scar at a commonly visible site of the body. We, therefore, intended to develop a new surgical approach allowing a scarless access for mediastinal lymph node biopsies. Evidence for such a procedure came from head and neck surgeons who evolved a transoral endoscopic access route for resection of the thyroid some years ago (10-12). Based on these finding we established this access route for mediastinal lymph node biopsies. Our previous studies utilized human cadavers and living pigs; both models demonstrated the feasibility to access mediastinal lymph nodes via the new surgical approach (13). Unclear was, whether this procedure can be safely used in humans as well. We, therefore, conducted a clinical phase I trial in patients with unclear mediastinal lymphadenopathy which could not be diagnosed by priorly performed bronchoscopy.
Methods
Approval and registration of the clinical study
The phase I proof-of-concept study was approved by the ethics committee of the Berliner Ärztekammer, Berlin, Germany (Eth-02/10). Informed written consent was obtained from all patients. The study was registered at the German Clinical Trials Register (DRKS00009886).
Patient selection
Patients with unclear mediastinal lymphadenopathy confirmed by CT scan were selected. All patients underwent prior bronchoscopy which was unable to provide histologically proven diagnosis of mediastinal lymphadenopathy.
Surgical technique
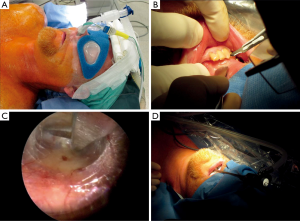
Patients were positioned in a supine position without reclination of the head. Transnasal intubation was performed using the endotracheal tube ENDOSID®, size 7–7.5, from ASID BONZ GmbH, Herrenberg, Germany (Figure 1A). Neuromonitoring for the recurrent laryngeal nerve was provided by inomed Medizintechnik GmbH (Teningen, Germany). After creating a sterile field in the mouth cavity using Octenisept® and at the anterior neck applying kodan Tinktur forte®, a sublingual sagittal mucosal incision, 10 mm in length, was placed between the papillae of the Wharton duct in the midline (Figure 1B). The muscles of the floor of the mouth (geniohyoid muscle, mylohyoid muscle, and anterior belly of the digastric muscle) were divided directly in the midline by Metzenbaum scissor to reach the plane beneath the superficial fascia of the neck and the platysma muscle. Subsequently, the ligaments which are fixed to the hyoid bone in the upper third were divided. Using optical scissors including 2.7 mm 0° Hopkins endoscope (KARL STORZ GmbH, Tuttlingen, Germany) the thyroid cartilage of the larynx was passed. Thereafter, the plane of the pretracheal strap muscles became visible (Figure 1C). Above the strap muscle, a working space was created followed by insertion of a 6 mm camera trocar of 200 mm length and with flap valve (KARL STORZ GmbH). Thereafter, CO2 was insufflated at 6.0 mmHg pressure (Figure 1D).
After CO2 insufflation, the mucosa in the vestibule of mouth was incised bilaterally 1 cm lateral to the buccal fold at the level of the canine teeth for a length of 5–10 mm (Figure 2A). Care was taken not to injure the mental nerve. The same trocars as described above were directed bilaterally below the platysma muscle into the infra-laryngeal working area (Figure 2B).
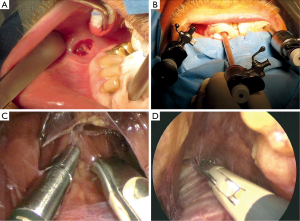
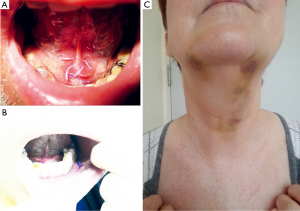
With both working trocars in place, strap muscles in the midline were divided and the thyroid gland became visible. If necessary, the isthmus of the thyroid gland was divided in the midline using a harmonic scalpel (Ultracision®, Ethicon Endo-surgery, Norderstedt, Germany) to avoid the risk unnecessary bleeding (Figure 2C). Below the thyroid gland the trachea was identified and followed down to the mediastinum where the innominate artery (brachiocephalic trunk) became visible. The next steps were similar to normal mediastinoscopy including the visualization of the azygos vein and the pulmonary artery followed by lymph node biopsies (Figure 2D). At the end of the procedure, sub-lingual incision and the incisions at the vestibule of the mouth were closed with absorbable sutures (Figure 3A,B).
Postoperative monitoring
Clinical assessment was performed daily. It was started at the day of operation. To determine the level of pain, sensation disturbance, swallowing dysfunction and subcutaneous emphysema, a score from 1 to 10 was used with 10 defined as very high. The clinical examination also included a careful inspection of the mouth cavity.
Results
Demographics
From August 2010 to January 2013 ten patients were recruited to the study. The distribution between sexes was equal. The median age was 50±13 years.
Surgical outcomes
All operations were carried out as cooperation between the head and neck surgeon (T Wilhelm) and two thoracic surgeons (W Klemm, A Nemat). Transoral endoscopic mediastinal surgery (TOEMS) was accomplished in eight patients. Two patients had to be converted to VAM. The reason was the occurrence of a tension pneumothorax in one patient at the right site which was caused by an inappropriate pressure for CO2 insufflation. The situation was cleared by insertion of a chest tube intraoperatively. The second conversion to VAM was due to a prolonged duration for the operation. There was an agreement to convert to VAM when the time for achieving the mediastinum extended 2 hours. The one case which had to be converted due to time limitation was caused by difficulties in surgical preparation reaching a wrong layer at pretracheal musculature. Counting for all accomplished TOEMS, the time to perform this operation was 159±22 min (mean ± SD). On average, two lymph node stations were reached through TOEMS procedure (in two patients one station, in five patients two lymph node stations, in one patient three stations). Most frequently gained lymph node station was 4R (seven patients) followed by 2R (three patients) and 4L (two patients).
Postoperative assessments
In the postoperative course permanent palsy of the right recurrent laryngeal nerve was noticed in one patient which was assessed as the second severe adverse event (SAE). Minor complaints were swelling, subcutaneous emphysema and hematomas at the anterior neck (Figure 3C). All of them cleared away within a few days spontaneously.
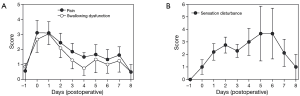
To further assess the postoperative course, pain, swallowing dysfunction and sensation disturbance were monitored on a daily base. Pain and swallowing dysfunction reached the highest level at the first postoperative day. After day 1, both parameters declined correspondingly (Figure 4A). In contrast, sensation disturbance which is caused by temporary paralysis of the mental nerve peaked at postoperative days 5–6 and declined thereafter (Figure 4B).
Histological outcomes
Histological evaluation of the lymph node biopsies taken by TOEMS revealed sarcoidosis in four patients and no pathological abnormalities in four cases. Importantly, histological examination clearly presented lymph node tissue in the biopsies taken from all patients who underwent TOEMS.
Discussion
TOEMS which use a transoral access route for mediastinal lymph node biopsies was evaluated in a clinical phase I study. When analyzing the trial, the most clear advantage of TOEMS is the absent of a visible scar after the operation. In contrast, all other invasive procedures for mediastinal lymph node biopsies produce apparent scars at the anterior neck. Application of scar-reducing or scarless operations seems to be a modern trend which is mostly preferred by young and educated patients (14,15). Moreover, patients with a negative body image tended to receive no scar surgery and were willing to accept increased surgical risks and higher costs to improve the cosmetic outcome (16). There is also evidence that less invasive surgery increases both the body image and cosmesis which was shown in a randomized controlled trial comparing laparoscopic single-port versus three-port appendectomy (17). Currently, similar trends for reducing the extent of surgical trauma are observed in thoracic surgery where thoracoscopic lobectomy using the single-port procedure was recently introduced (18,19). Moreover, natural orifice transluminal endoscopic surgery (NOTES) was evaluated by different groups to develop new access routes for thoracic surgery. Using canine and pig models, we and others applied NOTES for both transoral and transesophageal mediastinoscopy as well as for thoracoscopic lung biopsies (13,20,21). However, except TOEMS none of the new access routes for thoracic surgery has been examined for their feasibility in clinical studies so far.
Whether the transoral access for mediastinal lymph node biopsies used by TOEMS has other advantages than a scarless operation is unclear yet. It has to be considered that an operating time of nearly 160 minutes seems to be quite long. In comparison, the median time for VAMLA at our institution (ELK Berlin Chest Hospital) in 2014–2015 was 88±27 min (mean ± SD, n=55). However, despite having some practice from cadaver studies (13), the prolonged time to perform TOEMS was mainly due to the normal uncertainty accompanied with the introduction of a new surgical method and will be certainly reduced in the future. A second important issue for the assessment of TOEMS refers to the complication rate of the new procedure. Two SAEs were realized during the clinical study. One tension pneumothorax was determined, an event which was described before (22) but which is only rarely seen during mediastinoscopy since there is use of pressure-insufflated gas. The second major complication was a permanent palsy of the right recurrent laryngeal nerve. For normal mediastinoscopy, the frequency of clinically relevant palsy of the recurrent nerve was demonstrated in large retrospective series to be less than 1%. However, when using pre- and postoperative laryngoscopy for the determination of palsy of the recurrent nerve, the rate of this complication was increased up to 6.5% (23,24). In TOEMS we realized one patient with a postoperative palsy of the right laryngeal nerve. This complication is not very common, since mostly the left recurrent laryngeal nerve is affected after mediastinoscopy (25). Therefore, the determined palsy of the right laryngeal nerve after TOEMS was most likely a problem of anatomical preparation and should be considered with caution in future studies.
Summarizing our results, TOEMS based on NOTES was shown for the first time to be a feasible and safe transoral approach for mediastinal lymph node biopsies in patients with unknown mediastinal lymphadenopathy. The main advantage of the new procedure is a surgical approach which leaves no scars. Further trials are needed to evaluate whether TOEMS is equivalent to VAM in respect to morbidity as well as in regard to the negative predictive value and accuracy for the detection of mediastinal lymph node metastases.
Acknowledgements
The study was supported by the KARL STORZ GmbH (Tuttlingen, Germany) supplying surgical instruments and by inomed Medizintechnik GmbH (Teningen, Germany) who provided the equipment for monitoring the recurrent laryngeal nerve.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The phase I proof-of-concept study was approved by the ethics committee of the Berliner Ärztekammer, Berlin, Germany (Eth-02/10). Informed written consent was obtained from all patients. The study was registered at the German Clinical Trials Register (DRKS00009886).
References
- Lemaire A, Nikolic I, Petersen T, et al. Nine-year single center experience with cervical mediastinoscopy: complications and false negative rate. Ann Thorac Surg 2006;82:1185-9; discussion 1189-90. [Crossref] [PubMed]
- Carlens E. Mediastinoscopy: a method for inspection and tissue biopsy in the superior mediastinum. Dis Chest 1959;36:343-52. [Crossref] [PubMed]
- Zakkar M, Tan C, Hunt I. Is video mediastinoscopy a safer and more effective procedure than conventional mediastinoscopy? Interact Cardiovasc Thorac Surg 2012;14:81-4. [Crossref] [PubMed]
- Leschber G, Holinka G, Linder A. Video-assisted mediastinoscopic lymphadenectomy (VAMLA)--a method for systematic mediastinal lymphnode dissection. Eur J Cardiothorac Surg 2003;24:192-5. [Crossref] [PubMed]
- Specht G. Expanded mediastinoscopy. Thoraxchir Vask Chir 1965;13:401-7. [PubMed]
- Ginsberg RJ, Rice TW, Goldberg M, et al. Extended cervical mediastinoscopy. A single staging procedure for bronchogenic carcinoma of the left upper lobe. J Thorac Cardiovasc Surg 1987;94:673-8. [PubMed]
- Hürtgen M, Friedel G, Toomes H, et al. Radical video-assisted mediastinoscopic lymphadenectomy (VAMLA)--technique and first results. Eur J Cardiothorac Surg 2002;21:348-51. [Crossref] [PubMed]
- Zielinski M, Szlubowski A, Kołodziej M, et al. Comparison of endobronchial ultrasound and/or endoesophageal ultrasound with transcervical extended mediastinal lymphadenectomy for staging and restaging of non-small-cell lung cancer. J Thorac Oncol 2013;8:630-6. [Crossref] [PubMed]
- De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
- Wilhelm T, Harlaar JJ, Kerver A, et al. Surgical anatomy of the floor of the oral cavity and the cervical spaces as a rationale for trans-oral, minimal-invasive endoscopic surgical procedures: results of anatomical studies. Eur Arch Otorhinolaryngol 2010;267:1285-90. [Crossref] [PubMed]
- Wilhelm T, Benhidjeb T. Transoral endoscopic neck surgery: feasibility and safety in a porcine model based on the example of thymectomy. Surg Endosc 2011;25:1741-6. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Wilhelm T, Klemm W, Leschber G, et al. Development of a new trans-oral endoscopic approach for mediastinal surgery based on 'natural orifice surgery': preclinical studies on surgical technique, feasibility, and safety. Eur J Cardiothorac Surg 2011;39:1001-8. [Crossref] [PubMed]
- Bucher P, Pugin F, Ostermann S, et al. Population perception of surgical safety and body image trauma: a plea for scarless surgery? Surg Endosc 2011;25:408-15. [Crossref] [PubMed]
- Li W, Xu H, Wang ZK, et al. Natural Orifice Translumenal Endoscopic Surgery (NOTES): patients' perceptions and attitudes. Dig Dis Sci 2011;56:2415-22. [Crossref] [PubMed]
- Lamadé W, Friedrich C, Ulmer C, et al. Impact of body image on patients' attitude towards conventional, minimal invasive, and natural orifice surgery. Langenbecks Arch Surg 2011;396:331-6. [Crossref] [PubMed]
- SCARLESS Study Group, Ahmed I, Cook JA, et al. Single port/incision laparoscopic surgery compared with standard three-port laparoscopic surgery for appendicectomy: a randomized controlled trial. Surg Endosc 2015;29:77-85. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i48-53. [PubMed]
- Gee DW, Willingham FF, Lauwers GY, et al. Natural orifice transesophageal mediastinoscopy and thoracoscopy: a survival series in swine. Surg Endosc 2008;22:2117-22. [Crossref] [PubMed]
- Yang C, Chu Y, Wu YC, et al. The lateral decubitus position improves transoral endoscopic access to the posterior aspects of the thorax. Surg Endosc 2012;26:2988-92. [Crossref] [PubMed]
- Furgang FA, Saidman LJ. Bilateral tension pneumothorax associated with mediastinoscopy. J Thorac Cardiovasc Surg 1972;63:329-33. [PubMed]
- Widström A. Palsy of the recurrent nerve following mediastinoscopy. Chest 1975;67:365-6. [Crossref] [PubMed]
- Walles T, Friedel G, Stegherr T, et al. Learning mediastinoscopy: the need for education, experience and modern techniques--interdependency of the applied technique and surgeon's training level. Interact Cardiovasc Thorac Surg 2013;16:450-4. [Crossref] [PubMed]
- Benouaich V, Marcheix B, Carfagna L, et al. Anatomical bases of left recurrent nerve lesions during mediastinoscopy. Surg Radiol Anat 2009;31:295-9. [Crossref] [PubMed]


