
Predictors of successful closure following open-window thoracostomy in patients with empyema: a single-center retrospective cohort study
Highlight box
Key findings
• The performance status (PS) before open-window thoracostomy (OTW) is an important factor affecting window closure.
What is known and what is new?
• OWT is an effective treatment for refractory empyema, aiming to save lives.
• When planning a treatment strategy after OWT, it is important to predict whether open-window closure is possible; this study revealed that the PS before OWT is an important factor affecting window closure.
What is the implication, and what should change now?
• We believe that informing patients preoperatively about the possibility that the window may not close after surgery will help them and their families be prepared for the challenges that follow such an occurrence.
Introduction
Empyema is a life-threatening infection that usually occurs after pneumonectomy or pneumonia, with a reported mortality rate of 10–30% (1,2). Appropriate drainage is the first step toward improving this infectious condition (3), and thoracentesis may be attempted during the acute phase (4). However, open drainage, including open-window thoracostomy (OWT), is an option for cases of uncontrollable infection and bronchopleural fistula (BPF).
OWT is an effective treatment for refractory empyema, with the aim of saving lives (5,6). The implementation and management of OWT require the intervention of a specialist institution. Additionally, an open window requires daily gauze changes, which can be a major hindrance to a patient’s life, especially if the patient is working. The distinctive foul odor from the wound can also cause the patient to become socially debilitated, and chronic chest pain and an open-window appearance can be sources of stress for the patient. Thus, the patient’s mental and physical suffering due to the open window is not minimal, and closure is desirable if infection control is possible.
There are cases in which performing an open-window procedure to save a patient’s life is unavoidable, and some patients are unable to undergo closure following an open-window procedure. When planning a treatment strategy after an open-window procedure, it is important to predict whether the open window can be closed before the procedure is performed. We believe that this prediction may contribute to a reduction in the length of hospital stay, avoidance of unnecessary procedures, improvement in patients’ quality of life, and alleviation of suffering.
The current study aimed to identify the factors related to open-window closure based on patients’ background factors before OWT. To the best of our knowledge, this study is one of the few evaluations (7,8) that have examined the identification of factors related to open-window closure based on patients’ background factors prior to OWT. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-2024-1941/rc).
Methods
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of the University of Occupational and Environmental Health, Japan (No. UOEHCRB20-109) and informed consent was obtained from all individual participants.
Study design and population
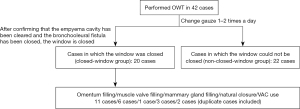
This observational retrospective cohort study was conducted at a single institution, the University of Occupational and Environmental Health, Japan, where 5,287 patients underwent thoracic surgery between April 2011 and March 2021. Of these, 42 consecutive patients (0.8%) underwent OWT for empyema. Data were retrospectively collected from medical and surgical records.
Surgical management of empyema
In our institution, the first step in empyema treatment is thoracentesis or debridement by video-assisted thoracoscopic surgery. However, because all patients had uncontrolled pleural infection, an open-window procedure was therefore performed.
The skin incision approach for the window procedure was determined based on the location of dead space in the chest cavity on preoperative Computed tomography images. This approach was selected to preserve as much muscle as possible. The median number of ribs cut during the window procedure was 3 (0–6), with three cases of lap windowing (wound protector placed between the ribs) without fracturing the ribs.
During the window period, the gauze was changed once or twice daily, depending on the condition of the chest cavity. Antibiotics were administered in some cases. The timing of window closure was determined based on a combination of clinical, institutional, and patient-centered considerations. Closure was typically performed when the chest cavity was adequately cleared of infection, healthy granulation tissue had formed, and any existing BPFs were resolved. These objective factors, which align with our institutional protocols, ensured that the surgical site was in optimal condition for closure, minimizing the risk of complications.
In addition to these clinical criteria, subjective factors also played a role in the decision-making process. Patients’ preferences, including their readiness to undergo closure and their expectations for recovery, were carefully considered. Quality of life factors, such as the effect of the open window on daily activities, physical discomfort, and psychosocial well-being, further informed the decision to proceed. This holistic approach ensured that closure decisions were tailored to the unique medical and personal circumstances of each patient.
Our institution’s basic policy for open-window closure depends on the patient’s general condition, the size of the thoracic cavity, the presence of fistulas, and infection control status.
-
Filling procedures: used for large cavities or when the closure of persistent BPFs is mainly required. The most reliable and resistant to infection is omentum, but it cannot be used if there is a history of abdominal surgery. Muscle valves such as the vastus dorsi, pectoralis major, and rectus abdominis should be considered depending on their volume and the location of the cavity. In women, the use of mammary glands should also be considered. -
Vacuum-assisted closure (VAC): preferred for debilitated patients or those who cannot tolerate major surgical interventions. The advantage is that it does not break ribs. -
Spontaneous closure: this is an option when the cavity is very small, the granulation appears looks good, and there is no large fistula.
Closure was possible in 20 patients (closure group) but was not in 22 patients (non-closure group). The closure methods employed for closure were omentum filling in 11 patients, muscle flap filling in 6 patients, breast tissue filling in 1 patient, spontaneous closure in 3 patients, and VAC in 2 patients (Figure 1).
Statistical analysis
The patients were divided into closed-window and non-closed-window groups, and these two groups were compared. Categorical variables were compared using the chi-squared test (or Fisher’s exact test if n<10). The cut-off value for categorical variables was determined based on the receiver operating characteristic (ROC) curve.
The following patient background factors before OWT were compared between the two groups: sex, age, left/right, performance status (PS), presence of malignancy, diabetes mellitus, body mass index before fenestration, presence of fistula, serum albumin level, hemoglobin (Hb) level, amount of residual pleural space, number of days from onset of empyema to fenestration, window surgery, number of ribs resected, presence of methicillin-resistant Staphylococcus aureus infection, use of steroids, and smoking index. The selection criteria for the variables included in the initial univariate model were based on a priori clinical relevance. Inclusion in the multivariate model was based on statistical significance (P<0.2) in the univariate model. Owing to the limited sample size (n=42), the number of predictor variables was limited to 4–5 based on the “rule of 10 events per variable” for the multivariate regression model. Statistical significance was set at a P value of <0.05. Finally, a survival analysis was performed to better understand the outcomes of patients with an open window. Kaplan-Meier analysis was conducted to determine overall survival (defined as the time from the date of open-window surgery to the date of death or last follow-up). The log-rank test was used to evaluate differences in survival rates between the open-window and non-open-window groups. All analyses were performed using SPSS software version 24.0 for Mac (IBM Corp., Armonk, NY, USA).
Results
Patient characteristics
This study included 32 male and 10 female patients, with a right/left difference of 27/15 and an average age of 68.1 years (36–83 years). Overall, 32 patients had fistulas, whereas 10 did not. Twenty-two patients had pneumonia (three cases of aspergillosis and two cases of nontuberculous mycobacterial disease) as the underlying disease. Furthermore, 19 patients underwent surgery for lung cancer (lobectomy or more); among these 19 patients, lobectomy was performed on the right side in 16 cases. One patient underwent surgery for a malignant pleural mesothelioma (Table 1).
Table 1
| Characteristic | Value |
|---|---|
| Age at the time of open-window thoracostomy (years) | 68 [36–83]† |
| Sex | |
| Male | 32 |
| Female | 10 |
| Left/right | |
| Left | 15 |
| Right | 27 |
| Fistula | |
| Present | 32 |
| Absent | 10 |
| Underlying disease | |
| Pneumonia | 22 |
| Postoperative lung cancer | 19 |
| Malignant pleural mesothelioma | 1 |
| Bacteria that caused the infection | |
| MRSA | 11 |
| Corynebacterium | 8 |
| Staphylococcus | 5 |
| Pseudomonas | 4 |
| Aspergillus | 3 |
| Streptococcus | 3 |
| Others | 8 |
| Number of days from onset of empyema to open-window thoracostomy | |
| <1 week | 22 (on the same day in 8 cases) |
| ≥1 week to <1 month | 11 |
| ≥1 month to <3 months | 7 |
| ≥3 months | 2 |
| Number of ribs removed | 3 (0–6)‡ |
†, values are presented as average [range]; ‡, values are presented as median (range). MRSA, methicillin-resistant Staphylococcus aureus.
In 8 cases, OWT was performed on the same day as the onset of empyema. In these 8 cases, OWT was performed immediately because of the severity of infection, the rapid deterioration of the patient’s condition, or the presence of a large BPF. Less invasive options were deemed inadequate to control the infection effectively.
Direct comparison between the closed-window and non-closed-window groups
A direct comparison of patient background characteristics was made between cases in which window closure was possible (closed-window group) and those in which window closure was not possible (non-closed-window group). The data are summarized in Table 2.
Table 2
| Characteristic | Closed-window group (n=20) | Non-closed window group (n=22) | P value* |
|---|---|---|---|
| Sex | 0.57 | ||
| Male | 15 | 17 | |
| Female | 5 | 5 | |
| PS | 0.005 | ||
| 0/1 | 16 | 8 | |
| 2/3/4 | 4 | 14 | |
| Left/right | 0.41 | ||
| Left | 8 | 7 | |
| Right | 12 | 15 | |
| Fistula | 0.10 | ||
| Present | 13 | 19 | |
| Absent | 7 | 3 | |
| Malignant tumor | 0.11 | ||
| Present | 7 | 13 | |
| Absent | 13 | 9 | |
| Diabetes | 0.43 | ||
| Present | 4 | 6 | |
| Absent | 16 | 16 | |
| Use of steroids | 0.62 | ||
| Present | 3 | 3 | |
| Absent | 17 | 19 | |
| MRSA | 0.43 | ||
| Present | 6 | 5 | |
| Absent | 14 | 17 | |
| Age (years) | 0.10 | ||
| <70 | 14 | 10 | |
| ≥70 | 6 | 12 | |
| BMI (kg/m2) | 0.26 | ||
| <18.5, ≥25 | 8 | 12 | |
| ≥18.5, <25 | 12 | 10 | |
| Albumin (g/dL) | 0.38 | ||
| <2.5 | 9 | 12 | |
| ≥2.5 | 11 | 10 | |
| Hb (g/dL) | 0.13 | ||
| <9.0 | 4 | 9 | |
| ≥9.0 | 16 | 13 | |
| Number of ribs removed | 0.46 | ||
| <3 | 6 | 8 | |
| ≥3 | 14 | 14 | |
| Brinkman index | 0.37 | ||
| <500 | 8 | 11 | |
| ≥500 | 12 | 11 | |
| Number of days until open-window thoracostomy | 0.51 | ||
| <8 days | 10 | 12 | |
| ≥8 days | 10 | 10 | |
| Amount of residual lung | 0.17 | ||
| <0.5 | 7 | 12 | |
| ≥0.5 | 13 | 10 | |
*, Chi-squared test and Fisher’s exact test are used for statistical analysis. BMI, body mass index; Hb, hemoglobin; MRSA, methicillin-resistant Staphylococcus aureus; PS, performance status.
Eight patients with PS0–1 did not achieve window closure; five had advanced malignancies, and three had persistent BPFs or advanced infections. Conversely, four cases with PS2 or higher closure, two of which achieved closure by less invasive methods such as VAC therapy or spontaneous closure. Three patients had fistulas, but none of them had undergone pneumonectomy for their underlying disease and there was little space in the thoracic cavity.
Fistula-related empyema had a lower closure success rate (43%) compared to non-fistula-related empyema (70%). Of the 32 cases with fistulas, 19 were identified as postoperative BPFs resulting from prior thoracic surgeries such as pneumonectomy, lobectomy, or segmentectomy. The remaining 13 patients experienced air leakage from bronchioles that were exposed owing to the destruction of lung tissue.
Next, we reanalyzed the data by dividing the cases into two major subgroups: infection-related cases and tumor-related cases.
Initial surgical procedures
The initial surgical procedures for each subgroup were as follows:
- Tumor-related cases (20 cases):
-
Closed-window group (7 cases): pneumonectomy (1 case), lobectomy (6 cases); -
Non-closed-window group (13 cases): pneumonectomy (3 cases), Lobectomy (10 cases).
-
- Infection-related cases (22 cases):
-
Closed-window group (13 cases): pneumonectomy (1 case), lobectomy (1 case), segmentectomy (1 case), partial resection (1 case), no resection (9 cases); -
Non-closed-window group (9 cases): pneumonectomy (2 cases), segmentectomy (1 case), no resection (6 cases).
-
Note: All non-malignant cases were associated with pneumonia or other infections, highlighting the distinction between tumor-related and infection-related etiologies.
Results of subgroup analysis
A comparison of closure success rates between the tumor and infection groups revealed a consistent difference:
-
Infection group: higher closure success rate (59%); -
Tumor group: lower closure success rate (35%); -
Chi-squared test results: the difference between the two groups did not reach statistical significance (P=0.11), likely due to sample size limitations and reduced statistical power.
Clinical implications
Despite not achieving statistical significance, this difference is clinically meaningful. The lower success rate in the tumor group can be attributed to complications commonly associated with malignancies, such as advanced tumor progression and BPFs. These findings underscore the importance of careful patient selection and tailored management strategies in tumor-related cases.
Search for predictors of successful closure before OWT
Nine variables were considered in the univariate analysis. The results are presented in Table 3.
Table 3
| Factors | OR | 95% CI | P value |
|---|---|---|---|
| PS 0/1 | 7.0 | 1.729–28.336 | 0.006 |
| No fistula | 3.41 | 0.74–15.68 | 0.12 |
| Age <70 years | 2.8 | 0.78–9.99 | 0.11 |
| Hb level ≥9.0 g/dL | 2.77 | 0.69–11.08 | 0.15 |
| No malignant tumor | 2.68 | 0.77–9.38 | 0.12 |
| Amount of residual lung >0.5 | 2.229 | 0.642–7.735 | 0.21 |
| 18.5 < BMI <25 (kg/m2) | 1.8 | 0.528–6.137 | 0.35 |
| No diabetes | 1.5 | 0.355–6.347 | 0.58 |
| Alb ≥2.5 g/dL | 1.467 | 0.434–4.951 | 0.54 |
Alb, albumin; BMI, body mass index; CI, confidence interval; Hb, hemoglobin; OR, odds ratio; PS, performance status.
The strong factors influencing window closure were “no malignant tumor” [odds ratio (OR): 2.68, 95% confidence interval (CI): 0.77–9.38, P=0.12], “no fistula” (OR: 3.41, 95% CI: 0.74–15.68, P=0.12), “age <70 years” (OR: 2.8, 95% CI: 0.78–9.99, P=0.11), and “Hb level ≥9.0 g/dL” (OR: 2.77, 95% CI: 0.69–11.08, P=0.15), with a significant difference observed for “PS 0/1” (OR: 7.0, 95% CI: 1.729–28.336, P=0.006).
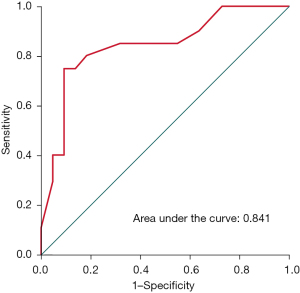
When multivariate logistic regression analysis was performed for the five items of “no malignant tumor”, “no fistula”, “age <70 years”, “Hb level ≥9.0 g/dL”, and “PS 0/1”, the ROC curve analysis for these predictive models indicated an area under the curve of 0.841 (Table 4, Figure 2).
Table 4
| Factors | OR | 95% CI | P value |
|---|---|---|---|
| PS 0/1 | 9.689 | 1.739–53.981 | 0.01 |
| No fistula | 1.787 | 0.293–10.898 | 0.53 |
| Age <70 years | 3.511 | 0.725–17 | 0.12 |
| Hb level ≥9.0 g/dL | 3.876 | 0.677–22.181 | 0.13 |
| No malignant tumor | 3.235 | 0.626–16.72 | 0.16 |
CI, confidence interval; Hb, hemoglobin; OR, odds ratio; PS, performance status.
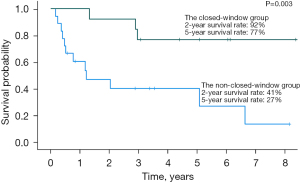
Prognostic analysis
The median follow-up duration was 35 months. Among 20 patients who underwent closure, none developed empyema or experienced bronchial stump fistula recurrence. The 5-year survival rates were 77% in the closed-window group and 27% in the non-closed-window group (Figure 3).
Discussion
When planning a treatment strategy after OWT, it is important to predict whether window closure is possible before window opening. The current study revealed that the PS before OWT is an important factor affecting window closure.
Empyema control relies on strategies that reduce bacteria and eliminate infections. Although surgical debridement is an effective initial procedure, OWT should be considered if the infection is not controlled after debridement. However, because OWT is one of the most invasive treatments, it is desirable to close the open window as soon as possible to improve both the quality of life and prognosis.
This retrospective study showed that the PS before OWT was involved in determining whether the open window could be closed. We believe that informing patients and their families before OWT about the possibility that OWT cannot be closed in patients with poor PS will provide them with some idea of what to expect. To the best of our knowledge, this study is one of the few evaluations attempting to identify patient background factors related to OWT closure before fenestration.
Hato et al. reported that lung cancer as an underlying disease was a statistically significant predictor of difficulty in closing the window (7). Massera et al. reported that lung cancer recurrence was the most common cause of difficulty in closing the window (8). In our study, the presence of malignant tumors as an underlying disease was a strong factor for the difficulty in closing the window; however, no significant difference was observed.
In addition, although it did not reach statistical significance, it was also suggested that the possibility of OWT closure was increased for “no fistula”, “age <70 years”, and “Hb level ≥9.0 g/dL”. The area under the curve for the prediction model for the five items of “no malignant tumor”, “no fistula”, “age <70 years”, “Hb level ≥9.0 g/dL”, and “PS 0/1” is 0.841, so we think that these five items can be used as a rough guide to the likelihood of closure before window opening.
Sziklavari et al. demonstrated the usefulness of VAC, particularly in debilitated patients (9). Based on our results, we cannot actively recommend open-window surgery for patients with poor PS. VAC is considered because it is possible that patients with PS defects cannot close their windows.
Hato et al. also showed in a univariate analysis of 35 patients that successful window closure was associated with mortality (7). This result is similar to that of our report.
Nonetheless, the optimal technique for closing a window and sealing the chest cavity remains controversial. The closure technique is often performed by opening the chest with a muscle or omental pedicle flap. The use of a muscle flap is one of the most common and acceptable procedures for window closure. A review by Kleeven et al. showed that pedicle flaps are preferable for window closure after window creation (10). In our cases, the omentum and muscle flaps were used as pedicle flaps, meaning that their original blood supply was preserved during the transfer to fill the thoracic cavity. We believe that the good outcomes in our cases were partly attributable to the use of pedicle flaps, which demonstrates the feasibility of our procedure.
This study has several limitations. First, this cohort study was conducted at a single institution and included only a small number of participants. We acknowledge the relatively small sample size, which reduces the power to detect statistically significant effects for certain predictors. In alignment with the commonly cited rule of requiring 10 events per predictor variable (EPV), we limited our multivariate logistic regression model to 5 predictors to ensure statistical robustness. However, subgroup analyses (e.g., dividing cases into malignant and infectious disease groups) further reduced the sample size in each group, which could affect the reliability of the results. Second, although some variables were included in the analysis, unmeasured confounders (e.g., other comorbid conditions) may have affected successful closure. Third, as this was a retrospective study of surgical cases, the patients included in the analysis were carefully selected, and our sample may not represent a cross-section of all patients with OWT.
Despite these limitations, our findings are consistent with previous studies, reinforcing their validity. In future research, the number of samples should be increased, and the predictive model should be further validated by considering various confounding factors and conducting subgroup-specific analyses to gain more detailed insights.
Conclusions
This study revealed that the PS before OWT is an important factor affecting window closure. Preoperatively informing patients with poor PS regarding the possibility of the window not closing after surgery, will give patients and their families a better chance to prepare themselves for such an outcome.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-2024-1941/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-2024-1941/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-2024-1941/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-2024-1941/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of the University of Occupational and Environmental Health, Japan (No. UOEHCRB20-109) and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Markatis E, Perlepe G, Afthinos A, et al. Mortality Among Hospitalized Patients With Pleural Effusions. A Multicenter, Observational, Prospective Study. Front Med (Lausanne) 2022;9:828783. [Crossref] [PubMed]
- Bobbio A, Bouam S, Frenkiel J, et al. Epidemiology and prognostic factors of pleural empyema. Thorax 2021;76:1117-23. [Crossref] [PubMed]
- Ricciardi S, Giovanniello D, Carleo F, et al. Which Surgery for Stage II-III Empyema Patients? Observational Single-Center Cohort Study of 719 Consecutive Patients. J Clin Med 2022;12:136. [Crossref] [PubMed]
- Clagett OT, Geraci JE. A procedure for the management of postpneumonectomy empyema. J Thorac Cardiovasc Surg 1963;45:141-5. [Crossref] [PubMed]
- Reyes KG, Mason DP, Murthy SC, et al. Open window thoracostomy: modern update of an ancient operation. Thorac Cardiovasc Surg 2010;58:220-4. [Crossref] [PubMed]
- Molnar TF. Current surgical treatment of thoracic empyema in adults. Eur J Cardiothorac Surg 2007;32:422-30. [Crossref] [PubMed]
- Hato T, Suzuki S, Harada M, et al. Comprehensive treatment approach is necessary for the closure of open window thoracostomy: an institutional review of 35 cases. Surg Today 2014;44:443-8. [Crossref] [PubMed]
- Massera F, Robustellini M, Pona CD, et al. Predictors of successful closure of open window thoracostomy for postpneumonectomy empyema. Ann Thorac Surg 2006;82:288-92. [Crossref] [PubMed]
- Sziklavari Z, Hammoudeh S, Petrone AM, et al. Outcomes of Vacuum-Assisted Closure in Patients with Empyema Thoracis: A 10-Year Experience. Ann Thorac Surg 2025;119:1206-12. [Crossref] [PubMed]
- Kleeven A, van der Hel SRP, Jonis YMJ, et al. Chest wall reconstruction after the Clagett procedure and other types of open-window thoracostomy: a narrative review. J Thorac Dis 2023;15:7063-76. [Crossref] [PubMed]


