
Application and validation of a newly developed lung donor (LUNDON) acceptability score for lung transplantation: a retrospective cohort study
Highlight box
Key findings
• The development and application of the lung donor (LUNDON) score is practical and can be feasibly adapted to the Chinese context; it may have implications for the selection of lung donors.
What is known and what is new?
• The persistent scarcity of accessible donor organs can be attributed to the low rates of lung utilization. One of the primary factors causing the low rates of lung utilization has been considered to be the absence of widely accepted criteria for evaluating the quality of donor lungs. The relatively rigorous criteria usually lead to the failure of the utilization of numerous potential lung donors. Previous studies have demonstrated the use of nonideal donors or extended-criteria donors, some of which have provided adequate transplant outcomes.
• In this study, we applied the LUNDON model using data from a Chinese hospital, aiming to further assess and validate its accuracy and determine the feasibility of its application for different populations.
What is the implication, and what should change now?
• In the context of Chinese hospitals, it is practical to apply the LUNDON score to expand the potential donor pool and improve the efficiency of lung transplantation.
• Future research should examine other factors that influence lung acceptability and seek to confirm the robustness of the LUNDON score across various settings in larger, multicenter studies with more diverse and comprehensive datasets.
Introduction
Background
Lung transplantation, which stands at the forefront of medical advancement, offers an option for patients with end-stage lung diseases, including chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis, cystic fibrosis, and coronavirus disease 2019 (COVID-19) and its complications (1-4). Advanced stages of these diseases pose immense challenges to patients, severely compromising their quality of life. As conventional treatments are limited in their ability to address the advanced stages of these conditions, lung transplantation has emerged as a crucial intervention. Over the past several decades, this intricate procedure has evolved into a transformative therapeutic option, with significant progress being made in the field of organ transplantation (4).
Although remarkable strides have been made in the field of lung transplantation, there remain a number of challenges, one of which is organ shortage (3). The persistent scarcity of accessible donor organs can be attributed, at least in part, to the low rates of lung utilization. One of the primary factors causing the low rates of lung utilization has been reported to be the absence of widely accepted criteria for evaluating the quality of donor lungs (5).
Rationale and knowledge gap
An ideal donor is considered to be an individual aged 20 to 45 years with no smoking history, normal bronchoscopy findings, a clear chest X-ray, and a ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2:FiO2) exceeding 350 mmHg (6). However, these relatively rigorous criteria usually lead to the failure of the utilization of numerous potential lung donors. Previous studies have demonstrated the viability of nonideal donors or extended criteria donors, some of which demonstrated similar transplant outcomes to those from ideal donors (7-12). It is within this context that innovative predictive models become paramount in expanding the pool of potential available lungs and enhancing the efficiency and success of lung transplantation.
Previous studies have established some scoring systems to quantify the acceptability of donor lungs. Donor variables taken into account included age, smoking history, chest X-ray, secretions, bronchoscopy findings, pulmonary infection, diabetes, and PaO2:FiO2, among others (13-18). Recently, Heiden et al. identified several new donor factors and formulated a novel lung donor (LUNDON) acceptability score using data from the Scientific Registry for Transplant Recipients (SRTR) database, aiming to facilitate the standardization of the lung donor evaluation process and increase lung utilization rates (5). The model only took donor characteristics into account without considering recipient outcomes, which is a distinguishing feature separating it from many other previously developed models.
Objective
In this study, we applied the LUNDON predictive model using data from a Chinese hospital, aiming to further assess and validate its accuracy and investigate the feasibility of its application in different populations. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-2025-259/rc).
Methods
Data source
This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments and was approved by the Ethics Commission of Wuxi People’s Hospital (No. KY24076). The need for informed consent was waived by the Ethics Committee of Wuxi People’s Hospital due to the retrospective nature of this study. None of the transplant donors were from a vulnerable population, and all donors or next of kin freely provided written informed consent.
We retrospectively reviewed a cohort of patients who underwent lung transplantation in Wuxi People’s Hospital, Jiangsu Province, China, between January 1, 2018 and December 31, 2022. According to Heiden et al.’s study (5), exclusion criteria were donation after circulatory death (DCD), age <16 years, and donors without a chest X-ray performed. In addition, donor lungs undergoing ex vivo lung perfusion (EVLP) were also excluded from the dataset of Heiden et al.’s study. Therefore, our study adopted the same exclusion criteria as Heiden et al.’s and those with missing information were also excluded, yielding a total of 553 lung donors with 9 donor factors in Heiden et al.’s predictive model who were included in the study. All the data were collected and checked by three researchers (Y Huang, C.C., L.C.), and the authors had no access to information that could identify individual participants during or after data collection. The clinical data were accessed on June 19, 2024, for research purposes.
This study will retrospectively apply the LUNDON score to the data of Wuxi People’s Hospital that meet the inclusion and exclusion criteria to evaluate the distribution trend of the LUNDON score. We will compare the ISHLT standard and the LUNDON scoring model to further verify the practicability, feasibility, and robustness of the LUNDON scoring. We will also analyze the post-transplantation prognosis of eligible recipients to reveal the value of the LUNDON score in predicting prognosis.
The limited single-center sample size, restricted follow-up period, and potential variables not included in the study may all carry the risk of bias.
Study outcomes
Donor LUNDON score
Lung acceptance was considered to be the acquisition of at least one lung from a donor, but whether a single or double allograft was procured was not distinguished. The final model developed by Heiden et al. to predict lung acceptability, which contained 9 donor factors including age, maximum creatinine, PaO2:FiO2 ratio, mechanism of death by asphyxiation or drowning, significant smoking history (>20 pack-years), previous history of myocardial infarction (MI), chest X-ray appearance, blood stream infection, and the occurrence of cardiac arrest, was applied (5).
Heiden et al. established an integer-based score in which higher scores correspond to an increased likelihood of lung acceptance. The corresponding points for different donor factors are shown in Table 1 (5). Additionally, they transformed the integer-based score into a predicted probability of lung acceptance to enhance the clinical utility of the scoring system and developed a user-friendly and web-based tool (i.e., the LUNDON acceptability score), which can be accessed online (https://sites.wustl.edu/lundon) (5).
Table 1
| Donor factor | Points |
|---|---|
| Age | |
| 15–24 years | 7 |
| 25–34 years | 7 |
| 35–44 years | 6 |
| 45–54 years | 4 |
| ≥55 years | 0 |
| Creatinine | |
| ≤3 mg/dL | 1 |
| >3 mg/dL | 0 |
| PaO2:FiO2 ratio | |
| <300 mmHg | 0 |
| ≥300, <350 mmHg | 3 |
| ≥350 mmHg | 10 |
| Mechanism of death (by asphyxiation or drowning) | |
| Yes | 0 |
| No | 1 |
| Smoking history | |
| ≥20 pack-years | 0 |
| <20 pack-years | 4 |
| Unknown | 3 |
| Previous myocardial infarction | |
| Yes | 0 |
| No | 2 |
| Unknown | 0 |
| Cardiac arrest | |
| Yes | 0 |
| No | 1 |
| Chest X-ray | |
| Normal | 3 |
| Abnormal | 0 |
| Bloodstream infection | |
| Yes | 0 |
| No | 1 |
FiO2, fraction of inspired oxygen; PaO2, arterial partial pressure of oxygen.
We applied both the integer-based score and the LUNDON score to evaluate this newly developed model. Furthermore, donor acceptability was also assessed according to the International Society for Heart and Lung Transplantation (ISHLT) standard donor criteria (19). In our analysis, an ideal standard criteria donor was defined as an age less than 55 years, a limited smoking history (<20 pack-years), normal chest X-ray findings, normal bronchoscopy findings, absence of organisms on sputum stain, and a PaO2:FiO2 ratio greater than 350 mmHg. To compare the sensitivity between the standard criteria and the proposed model, we investigated the acceptance rate using both criteria. The same theoretical cutoff value adopted in Heiden et al.’s study was also used (5). This approach facilitated a direct comparison between the ISHLT standard criteria and the newly developed model. In this study, the PaO2:FiO2 ratio was based on the latest arterial blood gas analysis performed following donor lung maintenance. Abnormal chest radiograph findings were characterized by the presence of pulmonary infiltrates, lung infection, atelectasis, or pulmonary contusion. Purulent secretions were defined as the presence of thick, yellow or green mucus observed during bronchoscopy.
Postoperative outcomes of recipients
To further evaluate the capacity of the LUNDON score model, we investigated the association between the score and postoperative recipient outcomes. Based on the LUNDON score, donors were divided into two groups: high (>60%) (n=316) and low (≤60%) (n=237) LUNDON score groups. Postoperative outcomes of recipients were compared between the two groups, which included duration of mechanical ventilation and extracorporeal membrane oxygenation (ECMO), length of intensive care unit (ICU) and hospital stay, occurrence of primary graft dysfunction, prevalence of acute rejection, postoperative complications [infection, anastomotic issues, arrhythmia, heart failure (HF), thrombosis, posttransplant lymphoproliferative disorder (PTLD), psychological issues, and liver or kidney injury], perioperative mortality, and 1-year survival.
Statistical analysis
Continuous data are reported as the mean ± standard deviation (SD) or median and interquartile range, and categorical data are reported as counts and percentages. Given the nonnormal distribution of the continuous data, the Mann-Whitney test was performed to compare early posttransplant recipient outcomes between the low and high LUNDON score groups. The Pearson Chi-squared test and Fisher’s exact test were conducted to compare the distribution of categorical variables. Kaplan-Meier survival analysis was performed for 1-year recipient survival across the low and high LUNDON score groups. A two-sided P value of less than 0.05 was considered statistically significant. All analyses were performed with SPSS 25 software (IBM Corp., Armonk, NY, USA).
Informed consent for human organ donation
The organs used in this study were procured in compliance with the relevant laws and regulations. When the organ procurement organization (OPO) identified a potential donor who met the donation criteria and had expressed a willingness to donate, this was promptly reported to the provincial management authority, and the information was registered on the China Human Organ Donation Case Reporting and Management System.
After receiving the information about a potential donor submitted by the OPO, the provincial management authority selected at least two coordinators to witness the donation process according to the assignment principles and made the assignment through the case reporting system. The coordinators verified the potential donor’s basic identity information, medical records, condition details, donation intent, and key family relationships.
Upon confirming the information of the potential donor, the coordinators informed the primary relatives of the potential donor about the principles of organ donation, emphasizing that it was voluntary and unpaid. They also explained the relevant legal and policy framework for organ donation. Subsequently, they witnessed the joint signing of the Relative Confirmation Registration Form for Human Organ Donation by all present primary relatives and the responsible representative from the OPO.
Results
Characteristics of donors
A total of 553 donors whose lungs were utilized for transplantation were included in the study, and all the demographic and clinical characteristics are presented in Table 2. The mean age of the donors was 41±11.2 years. There were 456 males, who accounted for the majority of the included donors (82.5%). The average BMI of the donors was 23.5±3.4 kg/m2, which was within the normal range. The mean PaO2:FiO2 of the study population was around 427.6±85.8 mmHg. The most common cause of death was cerebrovascular disease (n=311, 56.2%), followed by brain trauma (n=195, 35.3%), hypoxia or cardiac arrest (n=21, 3.8%), and central nervous system (CNS) tumors (n=6, 1.1%). Additionally, only 26 donors reported a significant smoking history of more than 20 pack-years, and 11 donors had a previous history of MI.
Table 2
| Characteristic | Value |
|---|---|
| Age (years) | 41±11.2 |
| Gender | |
| Male | 456 (82.5) |
| Female | 97 (17.5) |
| Weight (kg) | 67±13.5 |
| Height (cm) | 168±10.1 |
| BMI (kg/m2) | 23.5±3.4 |
| PaO2/FiO2 ratio (mmHg) | 427.6±85.8 |
| Cause of death | |
| Brain trauma | 195 (35.3) |
| Cerebrovascular disease | 311 (56.2) |
| Hypoxia/cardiac arrest | 21 (3.8) |
| CNS tumor | 6 (1.1) |
| Others | 20 (3.6) |
| Smoking history (>20 pack-years) | |
| No | 448 (81) |
| Unknown | 79 (14.3) |
| Yes | 26 (4.7) |
| MI history | |
| No | 542 (98.0) |
| Yes | 11 (2.0) |
| Chest X-ray | |
| Abnormal | 252 (45.6) |
| Normal | 301 (54.4) |
| Specimen culture (+) | |
| Blood culture | 9 (1.6) |
| Sputum culture | 122 (22.1) |
Data are presented as mean ± standard deviation or number (percentage). BMI, body mass index; CNS, central nervous system; FiO2, fraction of inspired oxygen; MI, myocardial infarction; PaO2, arterial partial pressure of oxygen.
Distribution of the LUNDON acceptability score
According to an integer-based score developed in Heiden et al.’s study (5), the distribution of the LUNDON acceptability score was determined (Figure 1). As reported in the previous Heiden et al.’s study (5), the maximum value of this score is 30, with higher scores indicating greater acceptability of the lungs.
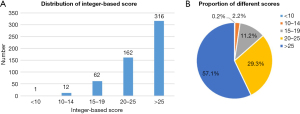
Overall, the integer-based score of the donors ranged from 9 to 30. Applying the online scoring tool developed by Heiden et al., the predicted probability of donor lung acceptance ranged from about 6.0% to 95.3%. Over 86% of the lung donors had an integer-based score of more than 20 (similar to the online LUNDON score of about 25%). Among them, nearly 60% (n=316) obtained a score of more than 25, which corresponded to a LUNDON acceptability score of 60%, while only around 2.5% (n=13) of the donors had a score of lower than 15.
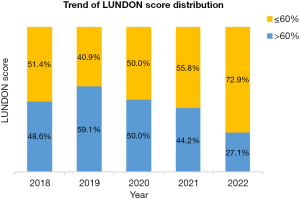
The trend of LUNDON score distribution of cases from 2018 to 2022
Based on the year of transplant, the trend of score distribution from 2018 to 2022 was determined (Figure 2). It was clear that donors with a lower LUNDON score were increasingly adopted during the study period. In 2018, donors with a LUNDON score higher than 60 accounted for nearly half of all utilized donors. From 2019 to 2022, there was a downward trend for the higher score group donors, declining from about 60% to 27.1%. In contrast, the number of utilized donor lungs in the lower score group rose from 40.9% in 2019 to 72.9% in 2022.
Lung acceptance evaluation under the standard ISHLT criteria and the LUNDON score model
To further assess this novel LUNDON acceptability score, lung acceptance rates under the standard ISHLT criteria and the LUNDON scoring system were compared, and consistent findings were found (Table 3). According to the ISHLT guidelines for lung donation, 31.5% of the utilized donors satisfied the standard criteria. With a LUNDON score cutoff of 25% (i.e., a 25% probability that lungs would be accepted), 80.3% of donor lungs were accepted, which was similar to the sensitivity of 87.5% in Heiden et al.’s study (5). Raising the cutoff value to 60% (i.e., a 60% probability that lungs would be accepted) yielded a similar proportion of donors meeting the criteria (57.1%), which was also similar to the sensitivity of the model in Heiden et al.’s study (5).
Table 3
| Criteria | Number | Acceptance rate (%) | Sensitivity in Heiden et al.’s study (5) (%) |
|---|---|---|---|
| ISHLT standard criteria | 174 | 31.5 | 31.8 |
| LUNDON score >25%† | 444 | 80.3 | 87.5 |
| LUNDON score >60%‡ | 316 | 57.1 | 50.6 |
†, corresponds to an integer score of approximately 20; ‡, corresponds to an integer score of approximately 25. ISHLT, International Society for Heart and Lung Transplantation; LUNDON, lung donor.
Postoperative recipient outcomes
Table 4 shows the early posttransplant outcomes of recipients across the low (n=237) and high (n=316) LUNDON score groups. There were no statistically significant differences in duration of postoperative mechanical ventilation and ECMO, length of ICU, or hospital stay between both groups. The prevalence of primary graft dysfunction of the low score group was 35.4%, while it was 28.7% in the high score group (P=0.13). The occurrence of arrhythmia differed significantly among the postoperative complications, with 33.3% of recipients experiencing arrhythmia in the low score group and 23.7% in the high score group (P=0.03). However, no significant differences were observed for other postoperative complications. Of note, the perioperative mortality of recipients who received lungs from donors with a LUNDON score lower than or equal to 60% was approximately 21.7%, and donors with a LUNDON score higher than 60% were associated with a recipient mortality of approximately 15.0% (P=0.04).
Table 4
| Variables | LUNDON ≤60% (n=237) | LUNDON >60% (n=316) | P value |
|---|---|---|---|
| Mechanical ventilation (hours) | 48 [35–202] | 48 [24–116] | 0.06 |
| Postoperative ECMO (hours) | 23 [17–69] | 22 [13–46] | 0.06 |
| ICU stay (hours) | 120 [66–237] | 108 [72–230] | 0.42 |
| Hospital stay (days) | 33 [19–54] | 35 [20–52] | 0.71 |
| PGD (%) | 35.4 | 28.7 | 0.13 |
| Acute rejection (%) | 1.0 | 0.8 | >0.99† |
| Postoperative complications (%) | |||
| Infection | 80.8 | 82.7 | 0.60 |
| Anastomotic stricture | 9.3 | 4.7 | 0.06 |
| Anastomotic leakage | 4.6 | 3.5 | 0.56 |
| Arrhythmia | 33.3 | 23.7 | 0.03* |
| Heart failure | 21.8 | 19.1 | 0.49 |
| Thrombosis | 3.1 | 1.2 | 0.19† |
| PTLD | 0.5 | 0 | 0.43† |
| Psychological issues | 18.1 | 16.5 | 0.66 |
| Kidney injury | 31.1 | 25.7 | 0.21 |
| Liver injury | 26.9 | 21.7 | 0.20 |
| Perioperative mortality (%) | 21.7 | 15.0 | 0.04* |
Data are presented as median [interquartile range] if not otherwise specified. †, Fisher’s exact test; *, statistically significant difference. ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; LUNDON, lung donor; PGD, primary graft dysfunction; PTLD, posttransplant lymphoproliferative disorders.
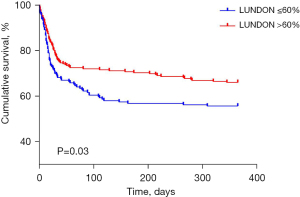
Figure 3 presents the 1-year survival estimate of recipients. The survival of recipients receiving donor organs with low or high LUNDON score differed significantly (P=0.03). The survival rate at 1 year after transplantation was 66.1% for the high score group and 55.7% for the low score group.
Discussion
Key findings
The application of the newly developed LUNDON acceptability score, as outlined in the study conducted by Heiden et al. (5), demonstrated value for addressing the persistent challenge of organ shortage in lung transplantation. In our study, we sought to validate and extend the utility of this predictive model within the context of a Chinese hospital setting. Our findings provide valuable insights into the practicability and feasibility of this scoring system, shedding light on its potential impact on lung donor selection.
Strengths and limitations
The LUNDON score, transformed from the integer-based score, was established to enhance the clinical utility of the scoring system to predict the probability of lung acceptance. According to Heiden et al.’s study, the score could be interpreted as follows: (I) a LUNDON score lower than 10% (integer-based score lower than 25) indicates a low likelihood of acceptance, but reversible lung pathology must be ruled out; (II) a LUNDON score ranging from 10% to 60% (integer-based score ranging from 15 to 25) indicates low-to-moderate likelihood of acceptance, but further donor and recipient characteristics assessment is needed; and (III) a LUNDON score higher than 60% (integer-based score higher than 25) indicates a high likelihood of acceptance, and attention should be paid to maintaining adequate pulmonary protection (5). In our study, more than 86% of the donors whose lungs were utilized for lung transplantation had an integer-based score of more than 20 (corresponding to an online LUNDON score of about 25%). Among them, 316 donors (57.1%) had a score of more than 25, which corresponded to a LUNDON acceptability score of 60%. These findings do suggest that a relatively high LUNDON score would have a higher probability of lung acceptance and successful transplantation, which, to some extent, demonstrates the accuracy of the model. Notably, approximately 2.5% (n=13) of the donors had a score of lower than 15, suggesting that a low LUNDON score does not necessarily indicate no possibility for lung utilization.
The percentage of recipients who received donor organs with a LUNDON score lower than 60% increased from 2019 to 2022, reaching 72.9% in 2022. This means that lung donors with a low LUNDON score were increasingly adopted during the study period. Moreover, we found that the low-score group still had a 1-year survival rate of more than 50%. A similar result was also identified in Heiden et al.’s study (5). In a previous study, donor lungs that did not satisfy these stringent criteria were nonetheless used, and successful outcomes of lung transplantation were observed (6). The study conducted by Choi et al. also examined older donor lung allografts in the donor pool (8). Donor lungs that did not meet the exact standard criteria could also be utilized in clinical scenarios and benefit patients with end-stage pulmonary diseases; this suggests that it is possible for a greater number of potential donor lungs to be utilized, thus mitigating the challenging situation of organ shortage.
Comparison with similar studies
Under different cutoff values of the model, the proportion of the lung donors meeting the criteria remained at similar values to the sensitivity of the model, which further validated the practicability and feasibility of the scoring system. Comparison of the LUNDON score with the ISHLT standard criteria also confirmed the robustness of the predictive model. At a cutoff value of 25% for the LUNDON score, 80.3% of the utilized donor organs were considered acceptable, a result that demonstrated concordance with the corresponding sensitivity in Heiden et al.’s study. This heightened sensitivity at a lower cutoff suggests that the LUNDON score captures a broader spectrum of acceptable donors. Compared with the ISHLT standard, the LUNDON score significantly increased the lung acceptance rate, potentially expanding the pool of potential lungs. The balance between sensitivity and specificity, determined through evaluating varying cutoff values, warrants careful consideration in the context of optimizing lung donor selection protocols.
Interpretation of findings
In our study, the division of donors into high (>60%) and low (≤60%) LUNDON score groups allowed for further evaluation of the predictive capacity of the novel scoring system beyond the assessment of donor lung acceptability. The analysis of the posttransplant outcomes of recipients revealed, to some extent, the prognostic value of the LUNDON score. Notably, the perioperative mortality showed statistically significant differences, with recipients of organs from donors with lower LUNDON scores having higher mortality rates compared to recipients of organs from those with higher scores. This suggests that the LUNDON score may have prognostic value in predicting the short-term survival of lung transplant recipients, emphasizing its potential role in refining donor selection criteria. Furthermore, the 1-year survival estimate demonstrated a significant difference between the low and high LUNDON score groups, with a higher survival rate observed in the recipients of organs from donors with higher LUNDON scores. This underscores this novel model’s possible value in predicting the long-term impact on recipient outcomes and supports its relevance beyond the immediate posttransplant period. Therefore, we believe that this newly developed scoring system may provide benefit in predicting short- and long-term outcomes after transplantation.
Implications and actions needed
Although our study contributes valuable insights into the novel model’s utility, it is essential to acknowledge certain limitations. First, the sample size of our study was limited, which might raise concerns regarding the capacity of our study to validate the model. Second, we also reported recipient findings with the aim to broaden the practical applications of the novel scoring system, but the follow-up period for survival analysis after transplantation was restricted. A short 1-year follow-up was used due to considerations of the available resources and the need for timely results. Longer follow-up periods are typically preferred to capture more extended survival patterns and potential events. Third, the protocols, practices, and patient demographics at our designated hospital may not fully represent the broader spectrum of lung transplantation scenarios. Fourth, the LUNDON score is a scoring result based on Western population data and has good applicability to the Western population, but its applicability to people of all races and regions in the world is still unclear. Therefore, future research should examine the additional factors influencing lung acceptability and seek to confirm the robustness of the LUNDON score across various settings in larger, multicenter studies with more diverse and comprehensive datasets.
Conclusions
Our study validated the practicability of the newly developed model, establishing the application value of the LUNDON acceptability score in the Chinese healthcare context. The validation of this predictive model, coupled with insights into temporal trends of lung donor selection, offers a more nuanced understanding of lung donor evaluation. In the dynamic landscape of lung transplantation, the LUNDON score has emerged as a promising tool that may revolutionize and optimize the allocation of limited organ resources. This novel model may be applied to a diversity of populations, aiding in the expansion of the lung donor pool and enhancing the efficiency and success of lung transplantation.
Acknowledgments
We would like to thank all participants in this study for their considerable efforts.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-2025-259/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-2025-259/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-2025-259/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-2025-259/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments and was approved by the Ethics Committee of Wuxi People’s Hospital (No. KY24076). The need for informed consent was waived by the Ethics Commission of Wuxi People’s Hospital due to the retrospective nature of this study. None of the transplant donors were from a vulnerable population, and all donors or next of kin freely provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chambers DC, Perch M, Zuckermann A, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-eighth adult lung transplantation report - 2021; Focus on recipient characteristics. J Heart Lung Transplant 2021;40:1060-72. [Crossref] [PubMed]
- Valapour M, Lehr CJ, Schladt DP, et al. OPTN/SRTR 2021 Annual Data Report: Lung. Am J Transplant 2023;23:S379-442. [Crossref] [PubMed]
- Kotloff RM, Thabut G. Lung transplantation. Am J Respir Crit Care Med 2011;184:159-71. [Crossref] [PubMed]
- Christie JD, Van Raemdonck D, Fisher AJ. Lung Transplantation. N Engl J Med 2024;391:1822-36. [Crossref] [PubMed]
- Heiden BT, Yang Z, Bai YZ, et al. Development and validation of the lung donor (LUNDON) acceptability score for pulmonary transplantation. Am J Transplant 2023;23:540-8. [Crossref] [PubMed]
- Chaney J, Suzuki Y, Cantu E 3rd, et al. Lung donor selection criteria. J Thorac Dis 2014;6:1032-8. [Crossref] [PubMed]
- Sundaresan S, Semenkovich J, Ochoa L, et al. Successful outcome of lung transplantation is not compromised by the use of marginal donor lungs. J Thorac Cardiovasc Surg 1995;109:1075-9; discussion 1079-80. [Crossref] [PubMed]
- Choi AY, Jawitz OK, Raman V, et al. Predictors of Older Donor Lung Use: Are We Too Good at Saying No? Ann Thorac Surg 2020;110:1683-90. [Crossref] [PubMed]
- Mulligan MJ, Sanchez PG, Evans CF, et al. The use of extended criteria donors decreases one-year survival in high-risk lung recipients: A review of the United Network of Organ Sharing Database. J Thorac Cardiovasc Surg 2016;152:891-898.e2. [Crossref] [PubMed]
- Hayes D Jr, Black SM, Tobias JD, et al. Influence of donor and recipient age in lung transplantation. J Heart Lung Transplant 2015;34:43-9. [Crossref] [PubMed]
- Shigemura N, Toyoda Y, Bhama JK, et al. Donor smoking history and age in lung transplantation: a revisit. Transplantation 2013;95:513-8. [Crossref] [PubMed]
- Grimm JC, Valero V 3rd, Magruder JT, et al. A novel risk score that incorporates recipient and donor variables to predict 1-year mortality in the current era of lung transplantation. J Heart Lung Transplant 2015;34:1449-54. [Crossref] [PubMed]
- Smits JM, van der Bij W, Van Raemdonck D, et al. Defining an extended criteria donor lung: an empirical approach based on the Eurotransplant experience. Transpl Int 2011;24:393-400. [Crossref] [PubMed]
- Ehrsam JP, Held U, Opitz I, et al. A new lung donor score to predict short and long-term survival in lung transplantation. J Thorac Dis 2020;12:5485-94. [Crossref] [PubMed]
- Schwarz S, Rahimi N, Kifjak D, et al. Comparison of donor scores in bilateral lung transplantation-A large single-center analysis. Am J Transplant 2021;21:2132-44. [Crossref] [PubMed]
- Reul RM, Loor G, Garcha PS, et al. Allograft discard risk index for lung transplantation. J Heart Lung Transplant 2021;40:1658-67. [Crossref] [PubMed]
- Oto T, Levvey BJ, Whitford H, et al. Feasibility and utility of a lung donor score: correlation with early post-transplant outcomes. Ann Thorac Surg 2007;83:257-63. [Crossref] [PubMed]
- Di Y, Fu R, Xiang Z, et al. Comparison of Prognosis for Lung Transplantation between Older and Younger Donors: A Systematic Review and Meta-Analysis Based on Cohort Studies. Ann Thorac Cardiovasc Surg 2024;30:24-00092. [Crossref] [PubMed]
- Copeland H, Hayanga JWA, Neyrinck A, et al. Donor heart and lung procurement: A consensus statement. J Heart Lung Transplant 2020;39:501-17. [Crossref] [PubMed]


