
Tracheostomy in COVID-19 critically ill patients: a bibliometric and visual analysis
Highlight box
Key findings
• This bibliometric analysis examines publications on tracheostomy in critically ill coronavirus disease 2019 (COVID-19) patients (2020–2023). The study identifies prominent authors, organizations, and countries, with Michael J. Brenner and Luis Angel as key contributors. The most frequent keywords include “tracheostomy”, “COVID-19”, and “SARS-CoV-2”. The European Archives of Oto-Rhino-Laryngology was the leading journal. Co-authorship and citation analyses revealed major research clusters and trends.
What is known and what is new?
• Tracheostomy is a common procedure for COVID-19 patients on prolonged ventilation, but the timing and best practices remain unclear.
• This study is the first bibliometric analysis of the field, providing insights into research patterns, collaborations, and emerging themes. It highlights the lack of standardized guidelines and the need for further research.
What is the implication, and what should change now?
• The findings underscore the need for clear clinical guidelines on tracheostomy in COVID-19 patients. Future research should focus on improving procedural safety, refining protocols, and addressing gaps in the literature. Enhanced interdisciplinary collaboration and global knowledge exchange are essential to improving patient care and clinical outcomes.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has emerged as a profound global health crisis, challenging healthcare systems worldwide with its unparalleled transmissibility and rapid spread (1-3). As the pandemic unfolded, a significant proportion of infected individuals exhibited mild to moderate symptoms. However, the sheer volume of cases quickly overwhelmed healthcare facilities, leading to a marked increase in patients requiring admission to intensive care units (ICUs) (2). For those experiencing severe manifestations of COVID-19, treatment often necessitated prolonged intubation and invasive mechanical ventilation, resulting in extended ICU stays and escalated sedation requirements (2).
In the context of critical care, tracheostomy has become a common and essential intervention for patients requiring prolonged mechanical ventilation (4-6). This surgical procedure, noted for its relative tolerance compared to endotracheal intubation, offers several potential benefits, including a reduction in the duration of mechanical ventilation and an expedited discharge from the ICU. By facilitating easier weaning from ventilatory support, tracheostomy may also enhance the overall availability of ICU beds, which became a pressing concern during the pandemic (7,8). The significant challenges associated with weaning patients off mechanical ventilation have led to increased reliance on tracheostomy as a vital component of critical care management for those severely affected by COVID-19 (5).
Given the critical role of tracheostomy in the care of these patients, the medical community has engaged in extensive discussions regarding the timing and indications for this intervention. Numerous scientific publications have emerged, contributing to an ongoing debate about best practices in this area. To navigate this complex landscape and assess the body of literature effectively, bibliometric analysis serves as a valuable tool, allowing researchers to quantitatively and qualitatively evaluate the existing publications related to this subject.
Bibliometrics employs statistical methodologies to analyze scholarly outputs, revealing trends, patterns, and gaps in research (9). This systematic approach not only illuminates the current state of the literature but also provides direction for future investigations (10). To the best of our knowledge, this study represents the first bibliometric examination of publications concerning tracheostomy in critically ill COVID-19 patients. By analyzing this body of work, we aim to offer a comprehensive quantitative assessment of its impact in the scientific community and provide insights to guide future research endeavors in this crucial area.
Methods
The global literature pertaining to tracheostomy in critically ill COVID-19 patients, published from 2020 to 2023, was systematically scanned in the Scopus database. To mitigate potential biases stemming from frequent database updates, the literature retrieval and data extraction were conducted on a single day, January 29, 2023. No constraints were imposed regarding language or data category. Search terms employed to identify relevant publications included “Tracheostomy” AND “COVID-19” OR “SARS-CoV-2” OR “2019-nCoV”. Data extraction was independently performed by two reviewers (R.M. and S.T.), encompassing details such as title, authors, journal, publication year, affiliations, language, keywords, paper type, abstract, citation count, among others. Discrepancies were resolved through consensus or, if necessary, by consulting a second pair of reviewers (A.R. and M.V.). Data were exported in CSV format for analysis. VOSviewer (version 1.6.18) was utilized for analyzing co-authorship, co-occurrence, citation patterns, bibliographic associations, and co-citations. In this study, VOSviewer parameters included a fractional count method and exclusion of documents with numerous authors (where the maximum number of authors per document was set at 25). Two standard weight attributes were applied: the links attribute and the total link strength attribute, indicating, respectively, the number of links of an article to other articles and the total link strength of an article to other articles. Since this was an exclusively bibliometric analysis, no statistical analysis of the collected data was performed.
Results
From the Scopus database, a total of 1,268 records focusing on tracheostomy in critically ill COVID-19 patients were identified. Following independent screening by two reviewers, 359 papers were ultimately included in the analysis. These comprised 207 (57.7%) original research articles, 31 (8.6%) review articles, 12 (3.3%) editorials, and 109 (30.4%) other types of publications, such as letters or conference papers. Among these, 46 (12.8%) papers were published in 2022, 162 (45.1%) were published in 2021, and the remaining 151 (42.1%) were published in 2020. The vast majority of publications (n=344, 95.8%) were written in English language, while the remaining were distributed across various languages: Chinese (n=3), French (n=3), German (n=2), Russian (n=2), Hungarian (n=1), Japanese (n=1), Korean (n=1), Slovenian (n=1), and Swedish (n=1). Furthermore, nearly all papers were accessible via open access.
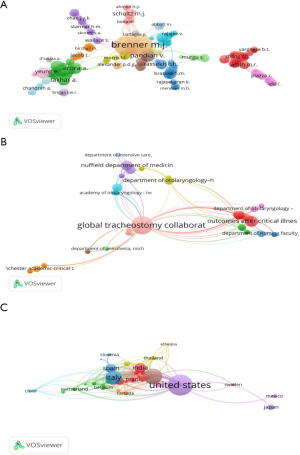
Bibliometric analysis of the co-authorship
A total of 1,849 authors contributed to the publication of papers on the topic of tracheostomy in critically ill COVID-19 patients. Michael J. Brenner, affiliated with the University of Michigan (USA), emerged as the most prolific author, with 23 published papers. His primary collaborator was Brendan A. McGrath from the University of Manchester (UK). The link attribute between them was 95, and their total link strength attribute was 23.
Our analysis further revealed that 1,195 organizations have contributed to these publications, although only 9 of them had more than 2 publications. The Global Tracheostomy Collaborative (USA) stands out with 13 related papers, garnering 56 citations. Their link attribute was 89, with a total link strength attribute of 13.
Furthermore, 77 countries have participated in publishing related papers, with 23 of them contributing at least 5 publications. The USA led in activity with 117 published papers. Its main partners included the UK and Italy. The link attribute between them was 37, with a total link strength attribute of 40.
The bibliometric analysis of co-authorship is showed in Figure 1.
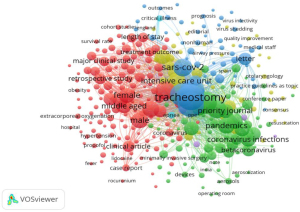
Bibliometric analysis of the co-occurrence
Keywords provided by authors of the paper that appeared more than 5 times in the Scopus database were included in the final analysis. Out of the 1,677 keywords, 326 met this threshold. Among these, the most frequently recurring keyword was “tracheostomy”, which appeared 336 times, with a link attribute of 325 and a total link strength attribute of 333. Following closely were “human” and “COVID-19”, occurring 303 and 261 times, respectively (Figure 2).
Bibliometric analysis of the citations
Table 1 lists the top 10 most cited papers on the topic of tracheostomy in critically ill COVID-19 patients. The mean citation count for these papers was 97.6, ranging from 56 to 212. The review titled “Tracheostomy in the COVID-19 era: global and multidisciplinary guidance” by McGrath BA et al. (published in Lancet Respir Med 2020) emerged as the most cited paper, cited 212 times.
Table 1
| Rank | Title | Journal | Paper type | Publication year |
|---|---|---|---|---|
| 1 | Tracheostomy in the COVID-19 era: global and multidisciplinary guidance (11) | Lancet Respir Med | Review | 2020 |
| 2 | Surgical Considerations for Tracheostomy During the COVID-19 Pandemic: Lessons Learned From the Severe Acute Respiratory Syndrome Outbreak (12) | JAMA Otolaryngol Head Neck Surg | Short survey | 2020 |
| 3 | Novel Percutaneous Tracheostomy for Critically Ill Patients With COVID-19 (13) | Ann Thorac Surg | Original article | 2020 |
| 4 | Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic (14) | Eur Arch Otorhinolaryngol | Review | 2020 |
| 5 | Recommendations from the CSO-HNS taskforce on performance of tracheotomy during the COVID-19 pandemic (15) | J Otolaryngol Head Neck Surg | Review | 2020 |
| 6 | CORONA-steps for tracheotomy in COVID-19 patients: A staff-safe method for airway management (16) | Oral Oncol | Editorial | 2020 |
| 7 | Outcomes After Tracheostomy in COVID-19 Patients (17) | Ann Surg | Original article | 2020 |
| 8 | Performing tracheostomy during the Covid-19 pandemic: guidance and recommendations from the Critical Care and Acute Care Surgery Committees of the American Association for the Surgery of Trauma (18) | Trauma Surg Acute Care Open | Original article | 2020 |
| 9 | Tracheostomy during SARS-CoV-2 pandemic: Recommendations from the New York Head and Neck Society (19) | Head Neck | Conference paper | 2020 |
| 10 | Tracheostomy protocols during COVID-19 pandemic (20) | Head Neck | Conference paper | 2020 |
CORONA, covering yourself, operating room setting, opening the trachea and nursing and airway management; COVID-19, coronavirus disease 2019; CSO, Canadian Society of Otolaryngology; HNS, Head & Neck Surgery; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
One hundred thirty-five journals have contributed to the publication of papers about tracheostomy in COVID-19, with 18 of them publishing at least five papers. A total of 133 papers were published in the top 10 active journals, accounting for 37% of the publications in the Scopus database. The European Archives of Oto-Rhino-Laryngology emerged as the journal with the most published and cited papers.
Luis Angel from New York University Langone Health was identified as the most cited author, with 197 citations. The links attribute and total link strength attribute were 497 and 677, respectively.
The Amandela ENT Head and Neck Centre of Singapore and the National University Hospital of Singapore were the most cited organizations, with 165 citations each. Both organizations had a links attribute and total link strength attribute of 172 and 173, respectively.
The most cited countries were the USA, UK, and Italy, cited 1,444, 883, and 791 times, respectively. The USA had a links attribute of 41 and a total link strength attribute of 944.
The bibliometric analysis of citations is depicted in Figure 3.

Bibliometric analysis of the bibliographic coupling and co-citation
In Figure 4, the bibliographic coupling maps of documents and sources are presented. The analysis yielded 12 clusters from the bibliographic coupling of documents. Cluster 1, highlighted in red, was the most prevalent, encompassing 93 items, with the most cited paper being McGrath BA et al.’s “Tracheostomy in the COVID-19 era: global and multidisciplinary guidance”, published in Lancet Respir Med 2020.
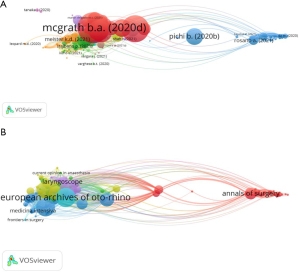
Similarly, six clusters emerged from the bibliographic coupling of sources, with Cluster 6, depicted in light blue, being the most represented, comprising 4 items, among which the European Archives of Oto-Rhino-Laryngology stood out as the journal with the most published and cited papers.
Figure 5 displays the co-citation maps of cited references, cited sources, and cited authors. The bibliometric analysis revealed 6,274 cited references, with only 53 of these being cited at least 5 times. The paper “Safe tracheostomy for patients with severe acute respiratory syndrome” by Wei et al., published in Laryngoscope in 2003 (21) and situated in the red cluster, emerged as the most cited reference, with 18 citations.

In terms of sources’ co-citation analysis, 1,330 sources were cited, with 160 of them being cited at least 5 times. JAMA, located in the light blue cluster, emerged as the most cited source, with 322 citations.
Out of 6,726 cited authors, 646 were cited over 5 times. Brenner MJ, situated in the purple cluster, emerged as the most cited author, with 155 citations.
Discussion
Timing and indications for performing tracheostomy in COVID-19 critically ill patients has been a subject of considerable interest in the literature, as evidenced by the findings of this bibliometric and visual analysis.
Three hundred and fifty-nine publications on this subject indexed in the Scopus database were meticulously examined.
Numerous authors have contributed to the corpus of literature on this topic. Brenner MJ emerged as the most prolific author, boasting 23 published papers, including the most cited paper (7). On the other hand, Angel L garnered the highest number of citations, solidifying his position as the most cited author.
A multitude of organizations have contributed to the publication of related papers. The Global Tracheostomy Collaborative emerged as the most active organization in terms of the number of publications. Conversely, in terms of citations, the Amandela ENT Head and Neck Centre of Singapore and the National University Hospital of Singapore were the most active organizations.
Seventy-seven countries have contributed papers on tracheostomy in COVID-19, with the USA leading with 117 published papers and also being the most cited country.
The keyword “Tracheostomy” emerged as the most frequent, strongly associated with “human”, “COVID-19”, and “SARS-CoV-2”.
One hundred thirty-five journals have published papers on tracheostomy in COVID-19, with the European Archives of Oto-Rhino-Laryngology being the most prolific and cited.
The co-citation analysis revealed 6,274 cited references, with the paper “Safe tracheostomy for patients with severe acute respiratory syndrome” by Wei et al., published in Laryngoscope in 2003 (21), emerging as the most cited reference.
In the co-citation analysis of sources, 1,330 sources were cited, with JAMA being the most cited source. Brenner MJ was identified as the most cited author among the 6,726 cited authors.
Many of the most cited publications have concentrated on technical considerations, offering recommendations and guidelines (11-20), as well as examining the timing and outcomes of tracheotomy in critically ill COVID-19 patients (22-25). Given that tracheotomy is an aerosol-generating procedure posing a significant risk of infection transmission to medical practitioners (26), several other articles have emphasized precautions to enhance safety and efficiency for healthcare workers (27,28). These publications suggest performing surgical and percutaneous tracheostomies with modified techniques to minimize aerosol generation and ensure personnel safety (29,30).
This study presents an inaugural, objective, and visually rich analysis of publications related to tracheostomy in critically ill COVID-19 patients, serving as a valuable resource for researchers invested in this area. The discussion aims to contextualize and interpret key findings, considering their implications for research, clinical practice, and future directions in airway management.
One notable aspect of the research is the predominance of English-language publications, which underscores the importance of language accessibility in disseminating research findings globally. However, the inclusion of works in other languages highlights the need for multilingual approaches to foster inclusivity and diversity in scholarly communication.
The collaborative nature of this research is further illustrated by contributions from authors across various countries, including China, the USA, Germany, and France, reflecting the global engagement in this critical area of study.
Moreover, the use of visual analysis methods, such as co-authorship networks and bibliographic pairing maps, provides insightful visual representations of collaboration patterns and knowledge structures within the literature. These visualizations enhance our understanding of relationships among authors, publications, and concepts, facilitating the identification of research clusters and influential nodes within the network. The insights derived from this bibliometric and visual analysis offer substantial value to a wide range of stakeholders, including researchers, clinicians, and policymakers engaged in airway management, particularly in the context of critically ill COVID-19 patients. By identifying key trends, emerging themes, and seminal works, the analysis provides a comprehensive understanding of the evolving body of literature on tracheostomy during the pandemic. For researchers, this information can serve as a critical foundation for shaping future study designs, ensuring that research efforts are aligned with current knowledge gaps and the most pressing clinical questions. Clinicians can leverage these insights to guide evidence-based decision-making, particularly when evaluating the risks and benefits of tracheostomy in COVID-19 patients, optimizing patient care, and refining treatment protocols. The identification of influential works and citation patterns also allows clinicians to stay informed about the latest advancements and evidence, ensuring that their practices are rooted in the most current and relevant research. Moreover, the analysis underscores the importance of interdisciplinary collaboration in addressing the multifaceted challenges posed by COVID-19. By revealing the interconnectedness of different research domains—such as critical care, respiratory medicine, and infectious diseases—this study highlights opportunities for cross-disciplinary partnerships that could lead to more holistic and innovative solutions. In this way, the bibliometric findings not only contribute to the academic discourse but also offer practical guidance for enhancing clinical outcomes and shaping policy decisions in the ongoing management of airway interventions in COVID-19 patients.
While this research offers significant insights, it is essential to acknowledge its limitations. Firstly, the analysis does not encompass all possible search databases, potentially restricting the scope of the findings. Secondly, there may be instances of duplicate authorship or authors holding honorary or part-time positions at multiple organizations, which could affect data accuracy.
Despite this we are convinced that this comprehensive analysis serves as a reference for advancing understanding and practice in the field of tracheostomy for critically ill COVID-19 patients, paving the way for future research endeavors and improved clinical outcomes.
Conclusions
Tracheostomy is a frequently employed procedure in critically ill patients, yet the absence of clinical guidelines delineating best practices is notable (31,32). This lack of standardized approach was particularly conspicuous during the COVID-19 pandemic. A bibliometric analysis of the literature on tracheostomy in COVID-19 offers a comprehensive overview of the existing literature on the subject.
By synthesizing quantitative data and visualizing network structures, this study contributes to a understanding research trends, collaboration models and knowledge dissemination in this clinical area, facilitating evidence-based practice and guiding future research efforts.
Acknowledgments
None.
Footnote
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-2024-1949/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-2024-1949/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kowalski LP, Sanabria A, Ridge JA, et al. COVID-19 pandemic: Effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck 2020;42:1259-67. [Crossref] [PubMed]
- Tonetti T, Grasselli G, Zanella A, et al. Use of critical care resources during the first 2 weeks (February 24-March 8, 2020) of the Covid-19 outbreak in Italy. Ann Intensive Care 2020;10:133. [Crossref] [PubMed]
- Vena A, Giacobbe DR, Di Biagio A, et al. Clinical characteristics, management and in-hospital mortality of patients with coronavirus disease 2019 in Genoa, Italy. Clin Microbiol Infect 2020;26:1537-44. [Crossref] [PubMed]
- Merola R, Iacovazzo C, Troise S, et al. Timing of Tracheostomy in ICU Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Life (Basel) 2024;14:1165. [Crossref] [PubMed]
- Vargas M, Sutherasan Y, Antonelli M, et al. Tracheostomy procedures in the intensive care unit: an international survey. Crit Care 2015;19:291. [Crossref] [PubMed]
- Piombino P, Troise S, Vargas M, et al. A systematic review of the literature on the role of tracheostomy in COVID-19 patients. Eur Rev Med Pharmacol Sci 2020;24:12558-74. [Crossref] [PubMed]
- Merola R, Vargas M, Sanfilippo F, et al. Tracheostomy Practice in the Italian Intensive Care Units: A Point-Prevalence Survey. Medicina (Kaunas) 2025;61:87. [Crossref] [PubMed]
- Cheung NH, Napolitano LM. Tracheostomy: epidemiology, indications, timing, technique, and outcomes. Respir Care 2014;59:895-919. [Crossref] [PubMed]
- Chen C, Dubin R, Kim MC. Emerging trends and new developments in regenerative medicine: a scientometric update (2000 - 2014). Expert Opin Biol Ther 2014;14:1295-317. [Crossref] [PubMed]
- Merola R, Mancino D, Vargas M. Videolaryngoscopy versus direct laryngoscopy: a bibliometric analysis. Br J Anaesth 2024;132:166-8. [Crossref] [PubMed]
- McGrath BA, Brenner MJ, Warrillow SJ, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med 2020;8:717-25. [Crossref] [PubMed]
- Tay JK, Khoo ML, Loh WS. Surgical Considerations for Tracheostomy During the COVID-19 Pandemic: Lessons Learned From the Severe Acute Respiratory Syndrome Outbreak. JAMA Otolaryngol Head Neck Surg 2020;146:517-8. [Crossref] [PubMed]
- Angel L, Kon ZN, Chang SH, et al. Novel Percutaneous Tracheostomy for Critically Ill Patients With COVID-19. Ann Thorac Surg 2020;110:1006-11. [Crossref] [PubMed]
- Takhar A, Walker A, Tricklebank S, et al. Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol 2020;277:2173-84. [Crossref] [PubMed]
- Sommer DD, Engels PT, Weitzel EK, et al. Recommendations from the CSO-HNS taskforce on performance of tracheotomy during the COVID-19 pandemic. J Otolaryngol Head Neck Surg 2020;49:23. [Crossref] [PubMed]
- Ferreli F, Gaino F, Cecconi M, et al. CORONA-steps for tracheotomy in COVID-19 patients: A staff-safe method for airway management. Oral Oncol 2020;105:104728. [Crossref] [PubMed]
- Chao TN, Harbison SP, Braslow BM, et al. Outcomes After Tracheostomy in COVID-19 Patients. Ann Surg 2020;272:e181-6. [Crossref] [PubMed]
- Michetti CP, Burlew CC, Bulger EM, et al. Performing tracheostomy during the Covid-19 pandemic: guidance and recommendations from the Critical Care and Acute Care Surgery Committees of the American Association for the Surgery of Trauma. Trauma Surg Acute Care Open 2020;5:e000482. [Crossref] [PubMed]
- Miles BA, Schiff B, Ganly I, et al. Tracheostomy during SARS-CoV-2 pandemic: Recommendations from the New York Head and Neck Society. Head Neck 2020;42:1282-90. [Crossref] [PubMed]
- Heyd CP, Desiato VM, Nguyen SA, et al. Tracheostomy protocols during COVID-19 pandemic. Head Neck 2020;42:1297-302. [Crossref] [PubMed]
- Wei WI, Tuen HH, Ng RW, et al. Safe tracheostomy for patients with severe acute respiratory syndrome. Laryngoscope 2003;113:1777-9. [Crossref] [PubMed]
- Battaglini D, Missale F, Schiavetti I, et al. Tracheostomy Timing and Outcome in Severe COVID-19: The WeanTrach Multicenter Study. J Clin Med 2021;10:2651. [Crossref] [PubMed]
- Queen Elizabeth Hospital Birmingham COVID-19 airway team. Safety and 30-day outcomes of tracheostomy for COVID-19: a prospective observational cohort study. Br J Anaesth 2020;125:872-9. [Crossref] [PubMed]
- Schultz MJ, Teng MS, Brenner MJ. Timing of Tracheostomy for Patients With COVID-19 in the ICU-Setting Precedent in Unprecedented Times. JAMA Otolaryngol Head Neck Surg 2020;146:887-8. [Crossref] [PubMed]
- Martin-Villares C, Perez Molina-Ramirez C, Bartolome-Benito M, et al. Outcome of 1890 tracheostomies for critical COVID-19 patients: a national cohort study in Spain. Eur Arch Otorhinolaryngol 2021;278:1605-12. [Crossref] [PubMed]
- Givi B, Schiff BA, Chinn SB, et al. Safety Recommendations for Evaluation and Surgery of the Head and Neck During the COVID-19 Pandemic. JAMA Otolaryngol Head Neck Surg 2020;146:579-84. [Crossref] [PubMed]
- Vargas M, Servillo G. Improving staff safety during tracheostomy in COVID-19 patients. Head Neck 2020;42:1278-9. [Crossref] [PubMed]
- Vargas M, Servillo G. Three-step checklist for tracheostomy in critically ill COVID-19 patients. Crit Care 2020;24:316. [Crossref] [PubMed]
- Portugal LG, Adams DR, Baroody FM, et al. A Surgical Safety Checklist for Performing Tracheotomy in Patients with Coronavirus Disease 19. Otolaryngol Head Neck Surg 2020;163:42-6. [Crossref] [PubMed]
- Vargas M, Russo G, Iacovazzo C, et al. Modified percutaneous tracheostomy in COVID-19 critically ill patients. Head Neck 2020;42:1363-6. [Crossref] [PubMed]
- Merola R, Troise S, Palumbo D, et al. Airway management in patients undergoing maxillofacial surgery: State of art review. J Stomatol Oral Maxillofac Surg 2025;126:102044. [Crossref] [PubMed]
- Vargas M, Pelosi P, Servillo G. Percutaneous tracheostomy: it's time for a shared approach! Crit Care 2014;18:448. [Crossref] [PubMed]


