Feeding after pancreaticoduodenectomy: enteral, or parenteral, that is the question
There is growing interest in the impact of nutritional status on patient’s outcome and in how this could be potentially modified through tailored nutritional support. Substantial evidence has been gathered in the surgical setting, where in association with a specific event and approach (elective surgical procedure)—the timing and the type of nutritional support are more likely to receive standardization than in other patient populations.
An interesting paper on this topic has recently appeared in the Annals of Surgery: “Early Enteral Versus Total Parenteral Nutrition in Patients Undergoing Pancreaticoduodenectomy: A Randomized Multicenter Controlled Trial (Nutri-DPC)” (1). This trial was designed to provide an answer to an apparent eternal dilemma: which is the best route of nutritional support after pancreaticoduodenectomy (PD)? Enteral or parenteral?
Particularly, the authors have compared nasojejunal early enteral nutrition (NJEEN) and total parenteral nutrition (TPN) and found that the former was associated with a higher rate of postoperative complications (77.5% vs. 64.4%, P=0.040). In the NJEEN group, they also observed a higher frequency of both overall (48.1% vs. 27.7%, P=0.012) and severe (grade B/C; 29.4% vs. 13.9%, P=0.007) postoperative pancreatic fistula (POPF), which clearly accounts for the difference in overall complications, and higher 90-day mortality (9.8% vs. 3.0%, P=0.049). Nonetheless, TPN was more successful in covering energy requirements. Therefore, based on the results of the Nutri-DPC trial, the answer to the aforementioned questions seems to be obvious: TPN should be preferred to NJEEN. However, it is still too early to say that TPN is better than EN.
The topic of nutritional support after PD deserves further discussion, as the space for research articles in scientific journals is frequently limited—and some issues have not been considered—and results of the Nutri-DPC trial are in clear contrast with available guidelines (2) and previous trials in the same area (3-6).
Indeed, the guidelines released by the European Society for Clinical Nutrition and Metabolism (ESPEN) generically address the patient undergoing any-type major abdominal surgery. Accordingly, tube feeding should be initiated within 24 h after surgery but it should be considered in patients in whom early oral nutrition cannot be initiated, with special regard to those with obvious undernutrition at the time of surgery, and in whom oral intake will be inadequate (<60%) for more than 10 days. Besides, tube feeding should be started with a low flow rate [e.g., 10–20 (max) mL/h] due to limited postoperative intestinal tolerance and, although it may take 5 to 7 days to reach the target intake, this is not considered harmful. Therefore, it is not surprising that in the Nutri-DPC trial TPN was more successful in covering energy requirements on postoperative day 5. However, it is worth highlighting that early EN has to be considered more for trophic and functional reasons than for avoiding a negative energy balance (7). Nonetheless, limited information is available on how the provision of EN was managed in this study.
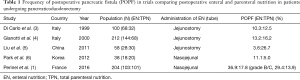
The design of clinical trials follows the “P.I.C.O.” principle according which a pre-defined patient population (“P”) is treated with a specific intervention (“I”) compared to another (“C”) with the aim to assess a potential effect on one or more outcomes (“O”). However, in respect to the issue of “intervention” other types of questions should be considered: what, how, where and when is it provided? Compared to most previous trials on the same topic (3-5), in the Nutri-DPC EN was delivered via a nasojejunal tube rather than using a needle catheter jejunostomy. Interestingly, the frequency of any-grade POPF in association with this feeding procedure was reported to be approximately 10% (Table 1), which is consistent with reviewed literature (8). In the trial conducted by Perinel et al. the incidence of POPF in the EN group was about 3-fold higher. There is also another small trial comparing TPN and NJEEN (6). Consistently with the Nutri-DPC trial, Park et al. found a 2-fold higher rate of POPF in the NJEEN group. However, the overall frequency POPF was similar to the studies using jejunostomy (6). A similar incidence of POPF (8.8%) has been reported by Rayes et al. in a RCT investigating the efficacy of postoperative synbiotic administration in reducing infections in patients receiving NJEEN after PD (9). The frequency of POPF reported in these two trials is consistent with the results (10.3%) of a recent systematic review of five feeding routes after PD (10). Therefore, two main questions arise from this picture: “Is a nasojejunal tube the appropriate route of feeding after DPC?” and “Are other factors and confounders (e.g., surgical approach and technique) likely responsible for a considerably high incidence of POPF in the NUTRI-DPC trial?” The latter is not an issue to be discussed in the present editorial. In respect to the former, it could be hypothesized that the presence of a nasojejunal tube is “mechanically” or “chemically” responsible for the leakage of the pancreatic anastomosis. Data suggest that the safety of nasojejunal tubes is lower compared to other routes of feeding due to a high risk of dislodgement (10,11). But also the infusion of enteral formula may contribute if not performed sufficiently far from the anastomosis. In many studies, as in the Nutri-DPC, the placement of a nasojejunal tube is not pertinently described but some authors have done this, clearly stating that the tip of the feeding tube has to be advanced for at least 30 cm after the anastomosis (11). Following this procedure the incidence of clinically relevant POPF is likely comparable to other studies (11%) (11). Besides, guidelines have recommended “when anastomoses of the proximal gastrointestinal tract have been performed deliver EN via a tube placed distally to the anastomosis” (2). This likely applies also to PD due to the need to realize during this operation a “critical” anastomosis.
Full table
Therefore, it is reasonable to argue that the Nutri-DPC trial does not challenge the advantages of postoperative enteral feeding but demonstrates the failure of delivering EN by a nasojejunal tube.
Nonetheless, another question may arise: is early EN indicated in all patients undergoing PD? ESPEN guidelines (2) recommend routine EN after major abdominal surgery, including PD, whereas American guidelines (12) do not, suggesting its use only in patients who are unlikely to meet their nutrient needs orally for a period of 7–10 days which is not necessarily the case after PD and something that could be anticipated. Indeed, perioperative support (before and early after surgery)—with EN being the first choice—in malnourished patients is recommended to improve several postoperative outcomes (2,12). However, specifically for PD, although EN appears to be safe and tolerated it did not reveal consistent advantages in terms of POPF, length of stay and infectious complications (13). A positive effect of EN has been shown only when enteral formula enriched with immune-nutrients are delivered (3,4). Accordingly, a study comparing EN (through jejunostomy), TPN and no support after PD in non-malnourished patients should be probably considered to clarify the importance of routine nutritional support and EN in absence of nutritional derangements.
Acknowledgements
None.
Footnote
Provenance: This is an invited Commentary commissioned by Ming Zhong (Associate Professor, Department of Critical Care Medicine, Zhongshan Hospital, Fudan University, Shanghai, China).
Conflicts of Interest: Dr. E Cereda has been a consultant and/or advisor to or has received speaker honoraria from Akern, Nutricia, and Wunder. The other authors have no conflicts of interest to declare.
References
- Perinel J, Mariette C, Dousset B, et al. Early Enteral Versus Total Parenteral Nutrition in Patients Undergoing Pancreaticoduodenectomy: A Randomized Multicenter Controlled Trial (Nutri-DPC). Ann Surg 2016;264:731-7. [Crossref] [PubMed]
- Weimann A, Braga M, Harsanyi L, et al. ESPEN Guidelines on Enteral Nutrition: Surgery including organ transplantation. Clin Nutr 2006;25:224-44. [Crossref] [PubMed]
- Di Carlo V, Gianotti L, Balzano G, et al. Complications of pancreatic surgery and the role of perioperative nutrition. Dig Surg 1999;16:320-6. [Crossref] [PubMed]
- Gianotti L, Braga M, Gentilini O, et al. Artificial nutrition after pancreaticoduodenectomy. Pancreas 2000;21:344-51. [Crossref] [PubMed]
- Liu C, Du Z, Lou C, et al. Enteral nutrition is superior to total parenteral nutrition for pancreatic cancer patients who underwent pancreaticoduodenectomy. Asia Pac J Clin Nutr 2011;20:154-60. [PubMed]
- Park JS, Chung HK, Hwang HK, et al. Postoperative nutritional effects of early enteral feeding compared with total parental nutrition in pancreaticoduodectomy patients: a prosepective, randomized study. J Korean Med Sci 2012;27:261-7. [Crossref] [PubMed]
- Jeejeebhoy KN. Enteral feeding. Curr Opin Clin Nutr Metab Care 2002;5:695-8. [Crossref] [PubMed]
- Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13. [Crossref] [PubMed]
- Rayes N, Seehofer D, Theruvath T, et al. Effect of enteral nutrition and synbiotics on bacterial infection rates after pylorus-preserving pancreatoduodenectomy: a randomized, double-blind trial. Ann Surg 2007;246:36-41. [Crossref] [PubMed]
- Gerritsen A, Besselink MG, Gouma DJ, et al. Systematic review of five feeding routes after pancreatoduodenectomy. Br J Surg 2013;100:589-98; discussion 599. [Crossref] [PubMed]
- Gerritsen A, Besselink MG, Cieslak KP, et al. Efficacy and complications of nasojejunal, jejunostomy and parenteral feeding after pancreaticoduodenectomy. J Gastrointest Surg 2012;16:1144-51; . [Crossref] [PubMed]
- ASPEN Board of Directors and the Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr 2002;26:1SA-138SA.
- Buscemi S, Damiano G, Palumbo VD, et al. Enteral nutrition in pancreaticoduodenectomy: a literature review. Nutrients 2015;7:3154-65. [Crossref] [PubMed]


