“Spiral stenting”—creating a subintimal neo-luminal helix around a massively calcified ostial chronic total occlusion of the right coronary artery in a patient with recurrent ventricular tachycardia
Case presentation
A 49 years old man presented with a non-ST-segment elevation myocardial infarction (NSTEMI) in March 2014. The patient’s medical history revealed an increased cardiovascular risk profile including the presence of arterial hypertension and dyslipidemia. Already in 2006 the patient received coronary artery bypass graft (CABG) surgery due to a coronary multi-vessel disease while exerting typical angina pectoris at low exercise levels according to Canadian Cardiovascular Society (CCS) class III. Coronary bypasses consisted of a left internal mammarian artery (LIMA) graft to the left anterior descending (LAD) coronary artery, a saphenous vein graft (SVG) to the obtuse marginal (OM) branch and a SVG to a diagonal branch. Additionally, past medical history consisted of end-stage renal failure due to glomerulonephritis [current glomerular filtration rate (GFR) 51 mL/min/m2], renal transplantation in 1999 and subsequent transplant failure in 2005. Afterwards the patient required regular renal replacement therapy and parathyroidectomy to avoid ongoing secondary hyperparathyroidism. In 2008 renal re-transplant was performed and finally lead to a constant improvement of GFR to 56 mL/min/m2.
Emergency coronary angiography showed diffuse coronary artery disease (CAD) with severe calcifications of all native coronary arteries. The right coronary artery (RCA) revealed a chronic total occlusion (CTO) initiating from the RCA ostium already. However, retrograde filling from septal collateral connections (CC) of the left coronary artery (LCA) was evident clearly (Figure 1). The LAD had a high-graded proximal stenosis, but was supplied by a patent LIMA graft with good distal run-off. The left circumflex (CX) coronary artery was occluded subtotally at the proximal part and was supplied by a highly degenerated and stenosed SVG supplying the OM branch.

The initial strategy was to treat the degenerated SVG to the OM branch. Three drug eluting stents (DES) (4.0/23 mm, 3.5/15 mm, 3.5/15 mm XIENCE) were implanted here with a good final result. Thereafter, the patient’s in-hospital course was complicated by subsequent worsening of heart failure [New York Heart Failure (NYHA) class IV, NT-proBNP 17,063 pg/mL] and re-current episodes of non-sustained ventricular tachycardias (ns-VTs). Left ventricular ejection fraction (LVEF) corresponded to 24% as assessed by trans-thoracic echocardiography. Due to optimal medical heart failure and antiarrhythmic treatment the patient could have been discharged without further complications. Additionally, transvenous implantation of an internal cardioverter defibrillator (ICD) was scheduled and performed in May 2015.
Unfortunately, the patient experienced re-hospitalization due to a recurrent episode of VTs being terminated adequately by multiple ICD shocks in July 2014. At this time, re-coronary angiography did not reveal further progress of multi-vessel coronary disease. Non-invasive myocardial viability testing by thallium scintigraphy and stress testing as well as positron emission tomography (PET) revealed preserved myocardial viability at the lateral and inferior site of the myocardium corresponding to the territory of supply of the RCA, possibly representing the origin of re-current ischemia-related VTs.
After discussing the patient’s medical history in a heart team in order to balance the advantages of percutaneous coronary intervention (PCI) versus a second redo of conventional CABG. Several reasons were considered: the LIMA graft to LAD was patent. A relevant stenosis of the right subclavian artery was evident and limited the use of the right mammarian artery as another arterial bypass. Further venous or arterial graft conduits were lacking due to previous CABG surgery and former hemodialysis at a radio-cephalic fistula. The EuroSCORE of the patient was 11.1%. Finally, decision was made to perform an interventional attempt to revascularize the CTO of the RCA before considering the patient for heart transplantation.
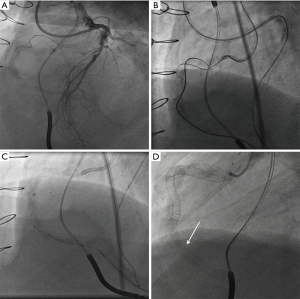
In September 2014 the CTO-procedure was performed using a bilateral femoral arterial access with two 7 French (F) introducer sheaths. A 7 F Amplatz left (AL) 1 and 7 F extra backup (EBU) 4.0 guiding catheter were used to intubate selectively the ostium of the RCA and LCA, respectively (Figure 1 and Figure 2A). Because of the presence of the long and extremely calcified CTO-lesion at the RCA aortic ostium with concomitant diseased distal segments, a retrograde interventional approach was chosen as the preferred PCI strategy. A Sion wire (ASAHI INTECC CO. Ltd., Nagoya, Japan) and a Corsair micro-catheter (ASAHI INTECC CO. Ltd., Aichi, Japan) were used to cross an intra-myocardial septal CC from the LAD to the RCA and was advanced through subintimal layers towards the distal CTO cap. However, the distal CTO cap could not be punctured retrogradely, at least not by a Confianza Pro 12 g wire (ASAHI INTECC CO. Ltd., Tokyo, Japan). Instead an Astato 20 g wire (ASAHI INTECC CO. Ltd., Aichi, Japan) was able to puncture the distal cap and was advanced by spiral-shaped subintimal tracking around the severely calcified native RCA starting at distal segment 2. However, even the stiffest wire was unable to exit into the aorta due to extreme ostial calcification. Therefore, antegrade puncture at the aorto-coronary ostium was successful using a Gaia 3rd (ASAHI INTECC CO. Ltd., Nagoya, Japan) supported within a Corsair micro-catheter (ASAHI INTECC CO. Ltd.) (Figure 2B). Afterwards entry into the subintimal space was achieved using an antegrade knuckled Pilot 200 wire (Abbott Vascular, North Chicago, Illinois, USA), which was created retrogradely before. Finally, a Sion Blue wire (ASAHI INTECC CO. Ltd., Aichi, Japan) was advanced within the micro-catheter to the distal segments of the RCA. In order to achieve a stable backup a 7 F GuideLiner (Vascular Solutions Inc., Minneapolis, MN, USA) was introduced during balloon dilatation within non-compliant (NC) balloon with increasing diameters 1.5 mm, compliant 2.5 and 3.5 mm (Figure 2C). In order to reduce the amount of contrast, injections were performed over the retrograde micro-catheter tip to guide final PCI. The overall implanted stent length was 132 mm (from distal to proximal): DES XIENCE Pro 2.75×38, 3.5×38, 3.5×38 and 4.0×18 mm (ostial). Due to stent recoil additional DES were implanted as a doubled layer (XIENCE Pro 4.5×38 mm proximally, 4.0×38 mm distally) (Figure 2D). Final post-dilation was performed using a Falcon Forte 5.0 (Invatec Technology Center GmbH, Frauenfeld, Switzerland) and a Thrombolysis in Myocardial Infarction (TIMI) flow grade 3 was achieved (Figures 3,4 and Figure 5A,B). Arterial access sites were closed with the Angio-SealTM vascular closure device (St. Jude Medical Inc., St. Paul, MN, USA). Overall procedural time lasted 240 min, fluoroscopic time was 132 min, cumulative radiation dose 26,197 uGym2 and the total amount of contrast was 150 mL. No peri-procedural or in-hospital complications occurred and the patient was discharged after 2 days of hospitalization.

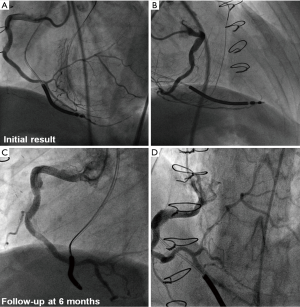
In April 2015 the patient presented back in a stable condition neither with further angina pectoris nor any subsequent episodes of ventricular arrhythmias. Invasive coronary angiography still revealed a patent RCA with regular TIMI 3 flow and the helical-shaped neo-luminal RCA as a result of “spiral stenting”. A small aneurysm at the proximal part of the RCA could be verified. (Figure 5C,D and Figures 6,7). Intravascular ultrasound (IVUS) examination showed no signs of relevant in-stent re-stenosis. There was a local proximal stent deformation due to compression by eccentric calcification with a sufficient calculated luminal area.


Discussion
To the best of our knowledge this case represents the first to describe the creation of a complete helical-shaped subintimal neo-lumen around a massively calcified and chronically total occluded coronary artery. A doubled stent layer had to be implanted due to significant recoil within the subintimal layer and increased burden of calcification.
Although success rates of PCI in CTOs may reach at least 90% in experienced CTO centres (6), several limiting and challenging factors do exist: on the one hand patients with CABG reveal more requirements to the interventional cardiologist, because these patients reveal a more complex coronary anatomy. On the other hand they reveal extreme and long-standing coronary calcification. Coronary arteries may be diseased and affected completely by CTOs along the main course of the artery (7). In these cases, subintimal tracking becomes necessary in order to reach a successful revascularization.
Naturally, subintimal tracking is intended to be kept as short as even possible. It has been described recently that long distances of subintimally implanted coronary stents reveal an increased rate of re-occlusion (8). In contrast, the presented patient showed a satisfactory angiographic result after 6 months of follow-up. The main reason for this finding may be most likely the valuable coronary flow TIMI 3 within the dominant RCA.
It appears noteworthy that our patient suffered from recurrent VTs being terminated adequately by ICD shocks prior to successful revascularization of the CTO of the RCA. Nombela-Franco et al. were able to demonstrate that patients with CTOs experience even more ICD shocks compared to patients with two- or three-vessel CAD without a CTO (9). Furthermore, it was shown that interventional ablation therapy of VTs in patients with coronary CTOs do reveal a significantly higher rate of recurrent VTs thereafter compared to patients with CAD without an additional CTO (10). Based on these considerations the successful PCI of the CTO of the RCA in our patient might have been of prognostic relevance, because no further ventricular arrhythmias had been occurred at 6 months after the CTO intervention.
Conclusions
Contemporary tools and techniques for PCI of CTOs combined with second generation DES do allow effective and durable revascularization of most complex and extremely calcified CTO lesions. The PCI of CTOs represents a technically feasible treatment alternative besides surgical revascularization and might reduce mortality in patients with ischemia-related VTs.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Kambis Mashayekhi, Zivile Valuckiene, Hans Neuser, et al. Coronary angiogram with dual contrast injection showing a long and extremely calcified CTO-lesion at the aortic ostium of the RCA with concomitant diseased distal segments for which a retrograde interventional approach was chosen as the preferred PCI strategy. Asvide 2016;3:463. Available online: http://www.asvide.com/articles/1237
- Kambis Mashayekhi, Zivile Valuckiene, Hans Neuser, et al. Coronary angiograms in left anterior oblique position showing the initial result after complex retrograde CTO-PCI with a patent RCA with regular TIMI 3 flow and the helical-shaped neo-luminal right coronary artery as a result of “spiral stenting”. Asvide 2016;3:464. Available online: http://www.asvide.com/articles/1238
- Kambis Mashayekhi, Zivile Valuckiene, Hans Neuser, et al. Coronary angiograms in anterior posterior cranial position showing the initial result after complex retrograde CTO-PCI with a patent RCA with regular TIMI 3 flow and the helical-shaped neo-luminal right coronary artery as a result of “spiral stenting”. Asvide 2016;3:465. Available online: http://www.asvide.com/articles/1239
- Kambis Mashayekhi, Zivile Valuckiene, Hans Neuser, et al. Coronary angiograms in left anterior oblique position at 6 months of follow-up. Asvide 2016;3:466. Available online: http://www.asvide.com/articles/1240
- Kambis Mashayekhi, Zivile Valuckiene, Hans Neuser, et al. Coronary angiograms in anterior posterior cranial position at 6 months of follow-up. Asvide 2016;3:467. Available online: http://www.asvide.com/articles/1241
- EuroCTO-Club. European Registry on Chronic Total Occlusions (ERCTO), 2015. Available online: http://www.ercto.org/
- Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv 2011;4:213-21. [Crossref] [PubMed]
- Carlino M, Figini F, Ruparelia N, et al. Predictors of restenosis following contemporary subintimal tracking and reentry technique: The importance of final TIMI flow grade. Catheter Cardiovasc Interv 2016;87:884-92. [Crossref] [PubMed]
- Nombela-Franco L, Mitroi CD, Fernández-Lozano I, et al. Ventricular arrhythmias among implantable cardioverter-defibrillator recipients for primary prevention: impact of chronic total coronary occlusion (VACTO Primary Study). Circ Arrhythm Electrophysiol 2012;5:147-54. [Crossref] [PubMed]
- Di Marco A, Paglino G, Oloriz T, et al. Impact of a chronic total occlusion in an infarct-related artery on the long-term outcome of ventricular tachycardia ablation. J Cardiovasc Electrophysiol 2015;26:532-9. [Crossref] [PubMed]


