Completeness of revascularization in multivessel coronary artery disease
Multivessel coronary artery disease (CAD) is frequently encountered in clinical practice among patients with both stable and unstable presentations (1). The question of whether such patients should undergo complete (CR) versus incomplete (IR) revascularization continues to be debated (1-3). This issue was originally recognized and described among patients undergoing coronary artery bypass graft (CABG) surgery, where it was observed that CR conferred both a survival and symptomatic benefit in comparison to IR (3), with CR consequently achieving the stature of a surgical mantra and accepted as a truism (4).
Despite a wealth of studies exploring whether the goal the revascularization should be CR, numerous questions exist at the present time (Figure 1). These dilemmas arise not only from clinical studies with conflicting results, but also because our understanding of how we define CAD has evolved over time with a shift towards pursuing functional CR, in which ischemic-causing lesions undergo coronary revascularization [CABG, percutaneous coronary intervention (PCI) or hybrid] and non-ischemic lesions are treated with optimal medical therapy (5-7).
In a single-center, prospective, observational, cohort study of consecutive patients with multivessel CAD undergoing PCI with drug-eluting stents (DES) from January 2003 through December 2013, Chang et al. compared outcomes in those with CR vs. IR (8). Using propensity-score matching, there was no significant difference in the primary outcome of all-cause mortality (8.6% vs. 9.0%; HR 1.03; 95% CI, 0.80–1.32, P=0.83), as well as in the secondary outcomes of stroke and repeat revascularization; whereas the risk of acute myocardial infarction (MI) on follow up was higher in those with IR vs. CR (HR 1.86; 95% CI, 1.08–3.19, P=0.02) (8).
We offer the following observations. First, the study by Chang et al. used an anatomical definition of CR, in which CR was defined as the absence of diameter stenosis ≥50% in major epicardial coronary arteries or their side branches with diameter ≥2.5 millimeters after successful stent implantation during index hospitalization irrespective of the function or viability of relevant myocardium (8). It should be emphasized that there is no guideline or expert-consensus document addressing how CR should be defined with various existing definitions as summarized in Table 1 (1,2,9). While the anatomical-based definition has been the most widely used classification in completeness studies, reported in nearly 90% of manuscripts included in a large meta-analysis (10), in contemporary clinical practice, a functional and/or physiological approach is encouraged. According to this definition revascularization of ischemic territories, as demonstrated by either non-invasive stress testing or fractional-flow reserve, is pursued while medical management is recommended for non-flow limiting stenosis (5-7). Therefore, while the findings of the study by Chang et al. are informative and expand on the results seen in other observational studies of CR vs. IR we believe a prospective randomized clinical trial of CR vs. IR would have been preferable to retrospective propensity-matching. Furthermore, an ischemia-guided definition of CR that takes into account the functional status of the stenosis and the myocardium subtended by the vessel in question would have better reflected contemporary practice.
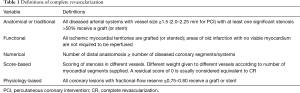
Full table
Recent data using myocardial perfusion imaging (MPI) has further elucidated on the importance of using a functional/physiological approach to define CR (11). In a small, retrospective analysis, Li et al. examined patients with evidence of stress-induced myocardial ischemia on SPECT MPI who had significant stenosis of the left main coronary artery and/or stenosis of at least one major coronary artery that had undergone PCI within 3 months after MPI with the purpose of evaluating the impact of IR by angiographic vs. functional (MPI) criteria (11). Similar to the findings by Chang et al., using the anatomical/angiographic definition, Li and colleagues demonstrated that a mean follow-up of 47±21 months there was no statistical difference in the cumulative incidence of all-cause death (primary endpoint) (12% vs. 24%, P=0.08); with no difference observed in major adverse cardiac events (MACE) (composite of all-cause death, non-fatal MI, repeat revascularization) (20% vs. 30%, P=0.28). However, when using the MPI criteria, patients with functional CR had a significantly lower cumulative incidence of both all-cause death (12% vs. 27%, P=0.048) and MACE (17% vs. 36%, P=0.025). The findings of this small, yet provocative study provide further insights into the value of using a functional/physiological-based definition.
Further supporting the use of functionally-guided CR, the Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) sub-study assessed whether the presence of residual angiographic disease using the residual SYNTAX score (RSS) and SYNTAX revascularization index (SRI) had prognostic significance after achieving functionally CR with FFR guidance and demonstrated that residual angiographic lesions that are not functionally significant do not predict a worse outcome (12).
Second, it has long-been recognized in studies examining CR vs. IR that observational studies have yielded conflicting results and large multicenter randomized clinical trials, while preferable from a methodological standpoint, are lacking (10). Ijsselmuiden et al. randomized 219 patients with multivessel disease to CR or culprit-only revascularization and found no benefit of CR during a follow-up of 4.6±1.2 years (13). There are 3 published RCTs showing benefit of CR in patients with ST-segment elevation acute myocardial infarction (STEMI) (14-16) and a large ongoing RCT (COMPLETE) trial (NCT01740479) expected to have results in 2018. Two large meta-analyses have been performed and both have favored CR over IR (10,17). Our group performed the largest meta-analysis (assessing both CABG and PCI) of CR in 35 studies including 89,883 patients, and demonstrated that relative to IR, CR was associated with a 30% reduction in long-term mortality, 22% reduction in MI, and a 26% reduction in repeat coronary revascularization; with the mortality benefit being consistent across studies irrespective of revascularization modality (CABG: RR 0.70; 95% CI, 0.61–0.80, P<0.001; and PCI: RR 0.72; 95% CI, 0.62–0.81, P<0.001) and the definition of CR (anatomic definition: RR 0.73; 95% CI, 0.67–0.79, P<0.001; and non-anatomic definition: RR 0.57; 95% CI, 0.36–0.89, P=0.014) (10). Similarly, Aggarwal et al. performed a large meta-analysis (nine studies, including 37,116 patients) focused exclusively on PCI during the stent era and demonstrated that compared to IR, patients undergoing CR had a 18% reduction in mortality, 33% reduction in non-fatal MI and 30% reduction subsequent CABG, with no difference in the incidence of repeat PCI (17).
Similarly, and in contrast to the findings by Chang et al., a recent large study of 23,342 patients assessing the long-term outcome of IR after PCI in the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) (18), in which IR was defined as any non-treated significant (at least 60%) stenosis in a coronary artery supplying over 10% of the myocardium, demonstrated that IR was associated with an adjusted hazard ratio (HR) of 2.12 (95% CI, 1.98–2.28, P<0.000) for the composite end-point of death, MI, or repeat revascularization at 1-year.
In summary, the study by Chang et al. adds to the existing literature of observational studies with conflicting results between IR and CR. Despite the existing differences observed among various observational studies, large meta-analyses studies have suggested a significant benefit of CR over IR. Many of the previously existing barriers to achieving CR, such as the presence of chronic total occlusion (CTO) have been surpassed in contemporary registries using the hybrid approach now reporting procedural success in over 90% of cases (19). Until we have more definitive data from COMPLETE, the best available evidence in 2016 suggests that CR using a physiology-based definition should be pursued whenever feasible in symptomatic patients with multivessel disease.
Acknowledgements
Funding: Dr. Garcia is a recipient of a career development award (1IK2CX000699-01) from the VA Office of Research and Development.
Footnote
Provenance: This is an invited Commentary commissioned by the Section Editor Yue Liu (Associate Professor, Department of Cardiology, The First Affiliated Hospital of Harbin Medical University, Harbin, China).
Conflicts of Interest: Dr. Brilakis—research support from the department of Veterans Affairs (PI of the Drug Eluting Stents in Saphenous Vein Graft Angioplasty-DIVA trial and Merit grant-I01-CX000787-01) and from the National Institutes of Health (1R01HL102442-01A1); consulting/honoraria from St Jude Medical, Boston Scientific, Asahi, Janssen, Sanofi, Abbott Vascular, Somahlution, Elsevier, and Terumo; research support from Guerbet; spouse is an employee of Medtronic. The other authors have nothing to disclose.
References
- Sandoval Y, Brilakis ES, Canoniero M, et al. Complete versus incomplete coronary revascularization of patients with multivessel coronary artery disease. Curr Treat Options Cardiovasc Med 2015;17:366. [Crossref] [PubMed]
- Ong AT, Serruys PW. Complete revascularization: coronary artery bypass graft surgery versus percutaneous coronary intervention. Circulation 2006;114:249-55. [Crossref] [PubMed]
- Buda AJ, Macdonald IL, Anderson MJ, et al. Long-term results following coronary bypass operation. Importance of preoperative actors and complete revascularization. J Thorac Cardiovasc Surg 1981;82:383-90. [PubMed]
- Vander Salm TJ, Kip KE, Jones RH, et al. What constitutes optimal surgical revascularization? Answers from the bypass angioplasty revascularization investigation (BARI). J Am Coll Cardiol 2002;39:565-72. [Crossref] [PubMed]
- Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol 2010;55:2816-21. [Crossref] [PubMed]
- Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007;49:2105-11. [Crossref] [PubMed]
- De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991-1001. [Crossref] [PubMed]
- Chang M, Ahn JM, Kim N, et al. Complete versus incomplete revascularization in patients with multivessel coronary artery disease treated with drug-eluting stents. Am Heart J 2016;179:157-65. [Crossref] [PubMed]
- Gössl M, Faxon DP, Bell MR, et al. Complete versus incomplete revascularization with coronary artery bypass graft or percutaneous intervention in stable coronary artery disease. Circ Cardiovasc Interv 2012;5:597-604. [Crossref] [PubMed]
- Garcia S, Sandoval Y, Roukoz H, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 2013;62:1421-31. [Crossref] [PubMed]
- Li J, Schindler TH, Qiao S, et al. Impact of incomplete revascularization of coronary artery disease on long-term cardiac outcomes. Retrospective comparison of angiographic and myocardial perfusion imaging criteria for completeness. J Nucl Cardiol 2016;23:546-55. [Crossref] [PubMed]
- Kobayashi Y, Nam CW, Tonino PA, et al. The Prognostic Value of Residual Coronary Stenoses After Functionally Complete Revascularization. J Am Coll Cardiol 2016;67:1701-11. [Crossref] [PubMed]
- Ijsselmuiden AJ, Ezechiels J, Westendorp IC, et al. Complete versus culprit vessel percutaneous coronary intervention in multivessel disease: a randomized comparison. Am Heart J 2004;148:467-74. [Crossref] [PubMed]
- Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med 2013;369:1115-23. [Crossref] [PubMed]
- Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol 2015;65:963-72. [Crossref] [PubMed]
- Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet 2015;386:665-71. [Crossref] [PubMed]
- Aggarwal V, Rajpathak S, Singh M, et al. Clinical outcomes based on completeness of revascularisation in patients undergoing percutaneous coronary intervention: a meta-analysis of multivessel coronary artery disease studies. EuroIntervention 2012;7:1095-102. [Crossref] [PubMed]
- Hambraeus K, Jensevik K, Lagerqvist B, et al. Long-Term Outcome of Incomplete Revascularization After Percutaneous Coronary Intervention in SCAAR (Swedish Coronary Angiography and Angioplasty Registry). JACC Cardiovasc Interv 2016;9:207-15. [Crossref] [PubMed]
- Christopoulos G, Menon RV, Karmpaliotis D, et al. The efficacy and safety of the "hybrid" approach to coronary chronic total occlusions: insights from a contemporary multicenter US registry and comparison with prior studies. J Invasive Cardiol 2014;26:427-32. [PubMed]