Ascending aorta reinterventions
Introduction
All patients who undergo ascending aorta surgery for the first time and/or an aortic valve replacement, and who are at risk of suffering an ascending aorta disease should be closely monitored using imaging techniques, such as computed tomography (CT), nuclear magnetic resonance (NMR), transthoracic echocardiography (TTE), and transesophageal echocardiography (TEE). The entire length of the diseased aorta should be considered, not only the treated segment; it is therefore necessary to closely monitor the whole aorta (1-3).
Ascending aorta reinterventions require a well-defined strategic approach in order to be successful. The associated technical difficulties require adequate planning of the intervention, whether cannulation, tissue dissection or prosthetic material is used (4-14).
Over time, we have learned that patients need ascending aorta reinterventions, and we have thus learned to pinpoint which patients require a more aggressive approach in the first intervention, in order to avoid reinterventions at a later stage. Patients undergoing bicuspid valve replacement surgery are at the highest risk of developing annuloaortic ectasia, dilatation or dissection of the ascending aorta; it is therefore important to also replace the ascending aorta when replacing the valve if the diameter of the ascending aorta is greater than 45 mm (3,4,15).
This article reports the main causes leading to ascending aorta reinterventions, and at which timepoint in the course of the disease they are performed. We also report the principal diagnostic techniques, the surgical strategies used, and we review the main studies published on this subject, identifying the principal post-reintervention mortality predictors, and the life expectancy of these patients.
Incidence and current situation
This type of disease currently represents up to 10% of ascending aorta surgery according to the various studies published. The mean interval between the first and second intervention varies between 40 and 60 months, and the majority of these reinterventions are elective, except in cases of acute aortic dissection, pseudoaneurysm, or endocarditis (3-8).
The causes that most often lead to ascending aorta and arch reinterventions vary depending on the study (see Table 1). The two main causes are the formation of an ascending aortic aneurysm following an aortic valve replacement (usually when a valve is replaced with a bicuspid aortic valve), and dilatation of the aorta in patients who undergo surgery for aortic dissection, and suffer an increase in the diameter of the untreated aortic segment, which usually presents with chronic dissection. Other causes are the development of pseudoaneurysm, infection of the aortic graft, or acute dissection in a previously operated patient. Finally, dysfunction or failure of the aortic prosthesis associated with dilatation of the ascending aorta is another cause. This failure often occurs after a valve-preserving procedure (David technique, Yacoub technique, etc.), or as a consequence of degeneration of a homograft or xenograft (3-8).
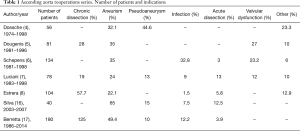
Full table
In the case of reinterventions due to an ascending aortic aneurysm, the purpose of the first intervention is usually to replace the aortic valve. Over time, these patients develop progressive dilatation of the aortic root and ascending aorta. Therefore, clinical guidelines recommend replacing the ascending aorta and changing the aortic valve at the same time when the diameter of the valve is greater than 4.5 cm, especially if the bicuspid valve is involved (15).
Over time, some patients with chronic dissection who have previously been operated on for acute type A dissection, develop dilatation of the segment of the aorta that was not replaced initially (distal ascending aorta and aortic arch). Many surgical teams recommend replacing the ascending aorta and aortic arch in type A aortic dissections, regardless of the presence of a second point of entry into the arch. Although this more aggressive approach is controversial, the majority agree that this method should be followed in younger patients (aged <50 years) or those with Marfan syndrome (1,2,11,12).
Clinical manifestations
The majority of patients remain asymptomatic and the disease is detected via imaging tests [echocardiography, CT scan or magnetic resonance imaging (MRI)] during check-ups. Annual follow-up is recommended for all patients who have undergone ascending aorta surgery. It is very important to maintain this follow-up for patients diagnosed with Marfan syndrome or connective tissue disorders, such as Ehler-Danlos syndrome, due to the rapid growth of the thoracic aorta in this patient group. The growth of the aorta (arch and descending segment) and the presence of residual valve regurgitation should be evaluated in this group if a valve-preserving procedure is performed; these facts have been shown to be independent predictors of long-term survival.
About 10% of patients who require aortic reintervention present with acute dissection or rupture, and require emergency surgery, with a very high rate of associated mortality.
Diagnosis and follow-up with imaging techniques
As noted above, patients who undergo replacement or repair of the aortic valve and/or replacement of the ascending aorta require yearly check-ups with imaging techniques. The entire aorta should be considered diseased, especially in patients with collagen disorders or a family history of aortic dissection or aneurysm. It is important to identify the course of the false and true lumens during follow-up, as well as the perfusion of the different organs and growth over time of the false lumen. This has been identified as a prognostic factor during follow-up.
As for the imaging techniques used, MRI is recommended as the technique of choice, although multislice CT and 3D reconstruction provide a very detailed and complete study. TEE makes it possible to study the valve function, particularly in valve-preserving techniques, and to identify the persistence of the false lumen (except in the arch).
Surgical indications
The indications for reinterventions on the ascending aorta are similar to those of the first intervention. However, given the complexity of reinterventions, associated comorbidities should be taken into account, such as lung or kidney disease, fragility or acute signs and symptoms of endocarditis or acute dissection, as these comorbidities involve a greater risk.
The ascending aorta diameter (>55 mm in patients with no connective tissue disorders, 50 mm in those with bicuspid problems and risk factors, and >42 mm in Marfan syndrome and connective tissue disorders), the speed of growth (>0.5 cm/year), and the baseline disease should all be taken into consideration. Therefore, a 50-year-old patient who has previously undergone bicuspid valve surgery with a diameter >50 mm should be operated on (15).
Patients who present with acute dissection, endocarditis, or pseudoaneurysm should be operated on urgently, taking morbidity into consideration. In this high-risk group of patients, it is particularly important for a multidisciplinary team to evaluate comorbidity. Therefore, a 78-year-old patient with chronic renal failure, associated vascular disease, and acute dissection could be rejected for surgery.
Indications for avoiding reintervention on the ascending aorta
- As pointed out above, the best approach is to prevent the need for reintervention. Patients with a bicuspid aortic valve are at the highest risk of developing aneurysm, dissection, or rupture of the aorta. When replacing the valve, the ascending aorta should be replaced (Bentall or Wheat procedure) if the diameter is greater than 45 mm.
- In case of bicuspid valve with ascending aorta greater than 50 mm and if risk factors coexists (coarctation of the aorta, systemic hypertension, family history of dissection, or increase in aortic diameter >3 mm/year) surgery of the aorta is indicated (15).
- The entire length of the aorta is diseased in patients with Marfan syndrome or connective tissue disorders, in whom a more aggressive approach is recommended, with a valve-preservation or Bentall procedure when the diameter of the aorta exceeds 42–45 mm. Moreover, if the arch is also diseased (>42–45 mm), or if the patient suffers acute dissection, the entire aortic arch should be replaced.
- In the event of heart surgery with associated dilatation of the ascending aorta, the latter should be replaced when the size exceeds 45 mm, bearing in mind the associated comorbidity.
Surgical technique
The majority of ascending aorta reinterventions can be performed via central aortic arch cannulation and under moderate hypothermia (32–34 °C). In reinterventions on the aortic arch and/or acute dissection, axillary artery cannulation is recommended. In the event of pseudoaneurysms or CT findings of the aorta being close to the sternum, peripheral cannulation with hypothermia at 24–26 °C is highly recommended (axillary artery-femoral vein, femoral artery and vein) to prevent accidents during resternotomy. In these cases, decompression of the left ventricle may be useful, by performing a left anterolateral mini-thoracotomy to avoid ventricular distension in the event of onset of ventricular fibrillation.
Axillary cannulation has been shown to be very useful in reinterventions where circulatory arrest is required, performing selective cerebral perfusion at a flow of 10 mL/kg/min and a temperature of 14 °C, to maintain radial artery pressure between 45 and 60 mmHg. In addition, systemic temperature tends to be maintained at 25–28 °C when using this technique. Adequate protection of the brain is achieved with this method, thereby avoiding systemic injuries caused by deep hypothermia, such as coagulation disorders, lung damage, or generalized inflammatory response (18-21).
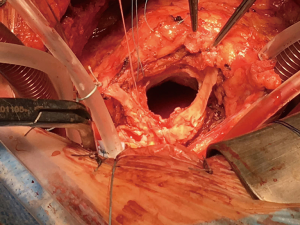
Tissue dissection can be very complicated due to associated adherences (Figure 1); it is therefore important to attempt to remove all of the diseased tissue. Regarding the technique used to replace the aortic valve and root, the Bentall procedure is recommended, occasionally with Cabrol modification (see Figure 2), in which an 8 mm tube should be used when the coronary ostia are difficult to mobilize because of either adherences or calcifications.
Results
Table 2 shows the results of the principal studies published on ascending aorta reinterventions. Hospital mortality varies from 5% to 15%, and depends on etiology and associated comorbidities. These studies give the following hospital mortality predictors: age, infection, acute dissection, emergency surgery, time of cardiopulmonary bypass, preoperative creatinine, and presence of associated lung disease. Two of these studies, one of which was performed with a propensity score analysis, show no difference in mortality compared with the first intervention, after adjustment for comorbidity risk (4-8,16,17).
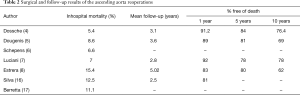
Full table
The most common postoperative complications are reintervention due to bleeding, neurological damage, and renal failure. In these studies, age and the need for circulatory arrest are identified as predictors.
The follow-up of these studies shows survival of 85–90% at 1 year, 80–84% at 5 years and 62–76% at 10 years. Once the higher hospital mortality of patients undergoing a first intervention has been surpassed, the hospital mortality of the group undergoing a second intervention is comparable to that of the first group during follow-up (4-8,16,17).
Conclusions
- Ascending aorta reinterventions are a challenge for surgeons, and are difficult to resolve. Given the progress made in perioperative management, and the experience gained, the hospital mortality rate is 5–15%, depending on etiology (infection, pseudoaneurysm, dissection), the need for emergency surgery, and comorbidity factors, such as kidney or lung disease.
- All patients undergoing surgery for aortic diseases should be closely monitored using imaging techniques, given the progression of the disease in the untreated segment, which increases the risk of acute aortic syndrome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Russo CF, Mazzetti S, Garatti A, et al. Aortic complications after bicuspid aortic valve replacement: long-term results. Ann Thorac Surg 2002;74:S1773-6; discussion S1792-9.
- Pieters FA, Widdershoven JW, Gerardy AC, et al. Risk of aortic dissection after aortic valve replacement. Am J Cardiol 1993;72:1043-7. [Crossref] [PubMed]
- Borger MA, Preston M, Ivanov J, et al. Should the ascending aorta be replaced more frequently in patients with bicuspid aortic valve disease? J Thorac Cardiovasc Surg 2004;128:677-83. [Crossref] [PubMed]
- Dossche KM, Tan ME, Schepens MA, et al. Twenty-four year experience with reoperations after ascending aortic or aortic root replacement. Eur J Cardiothorac Surg 1999;16:607-12. [Crossref] [PubMed]
- Dougenis D, Daily BB, Kouchoukos NT. Reoperations on the aortic root and ascending aorta. Ann Thorac Surg 1997;64:986-92. [Crossref] [PubMed]
- Schepens MA, Dossche KM, Morshuis WJ. Reoperations on the ascending aorta and aortic root: pitfalls and results in 134 patients. Ann Thorac Surg 1999;68:1676-80. [Crossref] [PubMed]
- Luciani GB, Casali G, Faggian G, et al. Predicting outcome after reoperative procedures on the aortic root and ascending aorta. Eur J Cardiothorac Surg 2000;17:602-7. [Crossref] [PubMed]
- Estrera AL, Miller CC 3rd, Porat E, et al. Determinants of early and late outcome for reoperations of the proximal aorta. Ann Thorac Surg 2004;78:837-45. [Crossref] [PubMed]
- Strauch JT, Spielvogel D, Lauten A, et al. Technical advances in total aortic arch replacement. Ann Thorac Surg 2004;77:581-89; discussion 589-90. [Crossref] [PubMed]
- Bachet JE, Termignon JL, Dreyfus G, et al. Aortic dissection. Prevalence, cause, and results of late reoperations. J Thorac Cardiovasc Surg 1994;108:199-205. [PubMed]
- Pugliese P, Pessotto R, Santini F, et al. Risk of late reoperations in patients with acute type A aortic dissection: impact of a more radical surgical approach. Eur J Cardiothorac Surg 1998;13:576-80; discussion 580-1. [Crossref] [PubMed]
- Yu HY, Chen YS, Huang SC, et al. Late outcome of patients with aortic dissection: study of a national database. Eur J Cardiothorac Surg 2004;25:683-90. [Crossref] [PubMed]
- Kazui T, Yamashita K, Terada H, et al. Late reoperation for proximal aortic and arch complications after previous composite graft replacement in Marfan patients. Ann Thorac Surg 2003;76:1203-7. [Crossref] [PubMed]
- Carrel T, Beyeler L, Schnyder A, et al. Reoperations and late adverse outcome in Marfan patients following cardiovascular surgery. Eur J Cardiothorac Surg 2004;25:671-5. [Crossref] [PubMed]
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014;35:2873-926. [Crossref] [PubMed]
- Silva J, Maroto LC, Carnero M, et al. Ascending aorta and aortic root reoperations: are outcomes worse than first time surgery? Ann Thorac Surg 2010;90:555-60. [Crossref] [PubMed]
- Berretta P, Di Marco L, Pacini D, et al. Reoperations versus primary operation on the aortic root: a propensity score analysis. Eur J Cardiothorac Surg 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Sabik JF, Nemeh H, Lytle BW, et al. Cannulation of the axillary artery with a side graft reduces morbidity. Ann Thorac Surg 2004;77:1315-20. [Crossref] [PubMed]
- Ueda Y, Okita Y, Aomi S, et al. Retrograde cerebral perfusion for aortic arch surgery: analysis of risk factors. Ann Thorac Surg 1999;67:1879-82. [Crossref] [PubMed]
- Bachet J, Guilmet D, Goudot B, et al. Antegrade cerebral perfusion with cold blood: a 13-year experience. Ann Thorac Surg 1999;67:1874-8. [Crossref] [PubMed]
- Moon MR, Sundt TM 3rd. Influence of retrograde cerebral perfusion during aortic arch procedures. Ann Thorac Surg 2002;74:426-31. [Crossref] [PubMed]