Video-assisted thoracoscopic right lower lobectomy: the Tianjin Chest Hospital experience
Introduction
Over twenty years of development in Video-assisted thoracoscopic lung surgery (VATS), has led to the development of innovative techniques for major lung resections which rivals the traditional open thoracotomy. VATS lobectomy is now well established and performed all around the world. Previously, there was much debate about the feasibility of the technique in cancer surgery and proper lymph node handling (1). Recently, several studies have shown no significant difference in post-op survival rates and that there might even be a better outcome by VATS (2-4); leading some to claim that VATS is at least not inferior to a resection via traditional thoractomy. A VATS lobectomy is a challenging and technically demanding procedure to perform, yet there lacks a consensus about the basic procedures for the technique. Currently, procedures is performed with a variation of up to 5 incisions (5,6), different lobe specific approaches and a wide variation of instruments and camera positions (7). The VATS pneumonectomy currently employed in the Department of Thoracic Surgery at Tianjin Chest Hospital of China is described below (Video 1).
Case presentation
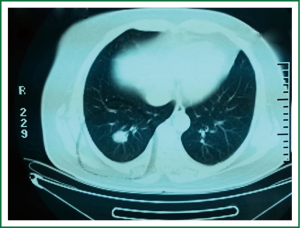
A 56-year-old woman presented with an incidental finding of a right lower lobe lesion on plain chest CT, which was a 25 mm × 15 mm lesion (Figure 1). The clinical diagnosis was Non-Small Cell Lung Cancer. There was no clinical symptom with the patient and no other therapeutic approaches was provided.
Operative techniques
Three ports were created to facilitate optimal views of the hilum and placement of the instruments during VATS. A 3 cm utility incision (extendable if necessary) was made in the 4th intercostal space along the right anterior axillary line. A 30 degree 10 mm high definition video thoracoscope was placed through the port in the 7th intercostal space along the right midaxillary line. The posterior incision (approx. 1.5 cm) was made under the inferior angle of scapula in the 9th intercostal space.
Since the lesion was located deep in the right lower lobe, local resection was unsuitable and lobectomy was considered. The first step of lobectomy was to assess the chest wall, pleurae and hilar structures, including the pulmonary artery, vein and bronchus, and confirm resectability. There was extensive adhesion between the chest wall and the upper and middle lobes. The upper and middle lobes were dissected with a combination of blunt and sharp incisions.
The lower lobe was retracted superiorly and the inferior pulmonary ligament was cut off. The posterior pleura was cut opened up to the level of the azygos vein. The lung was pushed anteriorly and the esophagus was retracted posteriorly. Then the subcarinal lymph nodes were exposed and excised and so the carinal bifurcation and the contralateral bronchus were exposed clearly.
After the subcarinal lymph nodes were dissected, the inferior pulmonary vein were easily exposed, encircled with a silk suture as a dragline and transected with a stapler inserted through the utility incision. Next, the pulmonary artery branches to right lower lobe, including superior segmental artery, was isolated after dividing the oblique fissure anteriorly. These artery branches was lifted away from the parenchyma with a silk suture and transected with a stapler inserted through the utility incision.
Next, when transecting the lower lobe bronchus, one should be sure of the position of the middle lobe bronchus on the right side and usually, the stapler should be closed at the site of the planned firing and the lung is then inflated to demonstrate airflow in the middle lobe.
After lobectomy, the station 2R and 4R nodes were removed en-bloc. The pleura was opened above the azygos vein. The fatty tissue including the nodes was gripped and dissected, and the whole tissue was removed in one piece.
Comments
We have presented a safe, reliable and reproducible procedure to VATS lobectomy here. Acceptability of the technique relates to benefits including reduced length of hospital stay, decreased blood loss, decreased pain, improved cosmesis, earlier return to normal activities and improved tolerance of chemotherapy. At our institution, we carry out the VATS operations from 2006 and finished the first VATS lobectomy in 2008. Over the last 3 years, more than 300 lobectomy cases were undertaken by VATS every year, and the cases increased year by year. At present, we have a large experience with about 900 cases performed by a standardized three-port anterior approach with sequential division of the hilar structures, proper lymph node handling, no rib spreading and vision relying on the monitor only. This allows us to perform VATS lobectomies in the majority of the cases even if there are significant difficulties and the rate of VATS lobectomy is 70% now. Of the all cases, diagnoses cover NSCLC and benign disease. Benign diagnoses include mycobacterial abscess, bronchiectasis, bullitis, et al. For NSCLC, tumours ranged from 5 mm to 5 cm in diameter. There were only a little conversions (<4%) for severe intra-operative haemorrhage, extensive adhesions, or need for complex resection. The complications occurring at a rate of less than 10% were prolonged air leak, pneumonia, intra-operative bleed, and so on. The 30-day mortality rate and in-hospital mortality rate were less than 1%. Most adopter think that the benefit of a standardized three-port anterior approach are: the utility incision is placed directly over the hilum and the major pulmonary vessels; Easy to deal with the major vessels in the procedure; The same approach to all lobes makes it easy to reproduce and learn; No need of changing the surgeons’ position or the place of the incision if a conversion is required (8). In terms of case numbers, our learning curve was estimated to be about 30 cases. In our opinion, master of this VATS lobectomies is not only needing a technical proficiency, but also having to overcome psychological factors. We believe that the increasing use of minimally invasive techniques for lobectomy and other major pulmonary resections would be highly desirable.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wright GM. Video-assisted thoracoscopic pulmonary resections - The Melbourne experience. Ann Cardiothorac Surg 2012;1:11-5. [PubMed]
- Downey RJ, Cheng D, Kernstine K, et al. Video-Assisted Thoracic Surgery for Lung Cancer Resection: A Consensus Statement of the International Society of Minimally Invasive Cardiothoracic Surgery (ISMICS) 2007. Innovations (Phila) 2007;2:293-302. [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [PubMed]
- Walker WS, Carnochan FM, Pugh GC. Thoracoscopic pulmonary lobectomy. Early operative experience and preliminary clinical results. J Thorac Cardiovasc Surg 1993;106:1111-7. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [PubMed]
- Gossot D. Technical tricks to facilitate totally endoscopic major pulmonary resections. Ann Thorac Surg 2008;86:323-6. [PubMed]
- Hansen HJ, Petersen RH. Video-assisted thoracoscopic lobectomy using a standardized three-port anterior approach - The Copenhagen experience. Ann Cardiothorac Surg 2012;1:70-6. [PubMed]