Complete video-assisted thoracic surgery right upper lobe sleeve resection
Introduction
Since 1990s, complete video-assisted thoracic surgery (VATS) lobectomy for the treatment of lung cancer experienced the initial exploration stage, followed by debate on the surgical outcomes within the surgeon community. This surgery was then gradually accepted by thoracic surgeons, and eventually written into the guideline for the diagnosis and treatment of lung cancer (1), which demonstrated its indispensible advantages over the traditional open approach. However, central lung cancer was still considered a contraindication of thoracoscopic surgery. In 2002, Santambrogio et al. reported the first thoracoscopic-assisted sleeve resection for the treatment of a mucoepidermoid carcinoma located at the left lower lobe bronchus (2). In 2008, Mahtabifard et al. first reported a lobectomy case series of totally thoracoscopic sleeve resection (3). In 2012, we performed complete VATS sleeve resection in a patient with central lung cancer at the right upper lobe (Video 1).
Case report
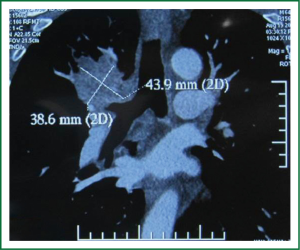
The patient was a 66-year-old male, who was admitted into our hospital due to coughing and blood-tainted sputum for over a month. He had a history of hypertension for 4 years, and a long history of heavy smoking, with a smoking index over 1,000 pack years. A chest CT scan, performed in other hospital on 10 August 2012, suggested a right upper lobe mass. A fibrous bronchoscopy, performed in our hospital on August 13, 2013, showed a neoplasm at the opening of the right upper lobe bronchus, blocking part of the bronchus. A biopsy with pathology suggested squamous carcinoma. A chest CT scan with enhancement, which was performed in our hospital on August 19, 2013, showed a right upper lobe mass considered as a central lung cancer, without visible lymph nodes enlargement in the mediastinum (Figure 1). The patient’s preoperative routine examinations did not reveal significant surgical contraindication, and his lung function was basically within the normal range.
Surgical techniques
The patient was placed in the left lateral decubitus position with slight anteversion. A cushion was placed underneath patient’s chest to elevate the chest. The ventilation of the patient was maintained using single lumen bronchus intubation with a right main bronchus blocker. The camera port, 1.5 cm in diameter, was placed in the eighth intercostal space on the right posterior axillary line, close to the scapular line. The main utility port, 4 cm in diameter and protected with a wound protector, was placed in the fourth intercostal space on the mid axillary line. An ancillary utility port, 1.5 cm in diameter, was placed in the sixth intercostal space on the anterior axillary line. A fourth port, 0.5 cm in diameter and to be used intraoperatively when necessary, was placed in the sixth intercostal space on the scapular line.
The inferior pulmonary ligament was divided and its lymph nodes were dissected. Mediastinal pleura anterior to the hilum were opened, and the upper lobe pulmonary vein was mobilized. The vein was then sealed and divided using a 45 mm Endo-GIA with a white load. The anterior apical branch of the upper pulmonary artery was mobilized and transected using a 45 mm Endo-GIA with a white load. Incomplete fissure was divided using a 60 mm Endo-GIA with a blue load. The posterior ascending branch of the upper pulmonary artery was divided using a 45 mm Endo-GIA with a white load.
Station 2, 4, 7, 10, and 11 lymph nodes were dissected. The right main bronchus and right middle bronchus were mobilized. The middle bronchus was divided using a scalpel at 1 cm below the opening of the upper lobe bronchus. The right main bronchus was divided using scissors at 1 cm below the opening of the upper lobe bronchus. The specimen was removed using a sample retrieval bag, and sent for frozen section pathology.
The end of the right main bronchus was anastomosed to the end of the middle bronchus using continuous 3-0 prolene sutures. The anastomosis was negative for the air leak, and middle and lower lobes were well inflated. Two drainage tubes were placed through the observation port and the ancillary utility port, respectively.
Discussion
To summarize, we believe several factors were critical to the surgical success in this case. The surgeon must be skilled with thoracoscopic operation techniques, and have strategies for the management of the accidents that may occur during the operation. The scope holder must be able to predict what the surgeon plans to do next, and be readily prepared to assist the surgeon. Before the operation, the location of the tumor, the length of the tissue affected, and its relationship to the trachea, bronchus and vessels, shall be accurately defined using bronchoscope and chest CT. Frozen section pathology shall be performed during the operation to ensure the negativeness of the margin. In cases without vessel invasion, pulmonary vessels and incomplete fissure shall be managed first, while the bronchus shall be mobilized at last. Surgeon shall try to sharply transect the bronchus, and produce even stump edges for convenient anastomosis. The anastomosis shall start from where it is relatively easier (4). In general, stitches shall be made at the membrane-ring border of both bronchus stumps, to align the stumps for the anastomosis. The anastomosis shall be made through the main utility port using a long needle holder and 3-0 prolene sutures. It shall start with continuous everted suture at the side, where the exposure is the most difficult. A pair of long forceps can be used to assist directing the needle.
Once the suturing on one side is completed, and the continuous suturing is conducted on the other side using a fresh needle and suture. The suture is tightened and knot is made at the border of bronchus membrane and cartilage ring. During the anastomosis, a certain distance shall be maintained between the needle entry point and the cutting edge of the trachea and bronchus. If the distance is too short, the tissue at the bronchus margin might be ruptured, as the suture is tightened. Surgeon shall be prepared to make open conversion at anytime, to ensure the safety of the patient.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ettinger DS, Akerley W, Bepler G, et al. Non-small cell lung cancer. J Natl Compr Canc Netw 2010;8:740-801. [PubMed]
- Santambrogio L, Cioffi U, De Simone M, et al. Video-assisted sleeve lobectomy for mucoepidermoid carcinoma of the left lower lobar bronchus: a case report. Chest 2002;121:635-6. [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [PubMed]
- Predina JD, Kunkala M, Aliperti LA, et al. Sleeve lobectomy: current indications and future directions. Ann Thorac Cardiovasc Surg 2010;16:310-8. [PubMed]