Analysis of the severity and prognosis assessment of aged patients with community-acquired pneumonia: a retrospective study
Introduction
Community-acquired pneumonia (CAP), a common infection, could occur in all ages. The annual incidence of CAP is ranged from 5-11 per 1,000 population per year, and the incidence is more higher in elderly patients (1). Some previous studies reported that the risk of pneumonia increases markedly with age, and CAP had become one of the leading causes of death in elderly patients and the first reason for death from infection diseases (2-4), which now remains a more high-profile area of health care.
The elderly CAP patients with many concomitant diseases are easier to progress to severe CAP (SCAP) and difficult to cure, because these non-specific symptoms causing not to be evaluated the illness severity accurately in early stage delay the timely and effective treatment. It was reported that the morbidity of SCAP ranged from 5% to 35% with the mortality ranging from 20% to 50% (5,6). Therefore, SCAP deserves more attention [severity monitoring and prognosis assessment in early stage, mechanical ventilation (MV), and so on] because it has been one of the common causes leading to death in aged patients.
Assessment of disease severity is important in the management of CAP patients, guiding therapeutic options, improving prognosis in Intensive Care Unit (ICU). With increasing incidence of CAP, several scoring models have been developed in an attempt to accurately predict outcomes for CAP patients, which were used to decide various nursing grades and guide both general management and antibiotic treatment by a series of related clinical and laboratory features (7) for initial antibiotic administration is of great importance for prognosis of CAP (8).
In recent decades, CURB-65 score (9) and Pneumonia Severity Index (PSI) (10,11) have been regularly conducted to make risk stratification and assess the prognosis of patients with CAP, and APACHE II is one of the most widely used scoring systems for predicting mortality of patients in the ICU (12). In clinical practice, we find that the higher plasma N-terminal pro B-type natriuretic peptide (proBNP) levels the aged patients with CAP have, the worse prognosis they could have. Some studies had documented that plasma proBNP as a promising biomarker not only have an important role in predicting the prognosis and mortality of chronic heart failure (13,14), but also was extensively used to provide risk stratification and predict mortality for patients with CAP (15-17).
The purposes of this study were to compare the ability of proBNP and the three scoring models (CURB-65, PSI, and APACHE II) on assessing the predictive accuracy for three clinical outcomes (severity evaluation, need for invasive mechanical ventilation, and 28-day mortality) of the aged patients with CAP admitted to ICU, and to evaluate the prognostic factors.
Materials and methods
Subjects
In this retrospective study, a total of 240 consecutive recruited patients, who were aged ≥65 years old with a diagnosis of CAP at admission to the Emergency Intensive Care Unit (EICU) and Respiratory Intensive Care Unit (RICU) of the Chinese People’s Liberation Army (PLA) General Hospital, was analyzed from Jan 2011 to April 2013.
The study design was approved by the Clinical Ethics Committee of the Chinese PLA General Hospital. All of the patients or their family members were sufficiently informed the study details, and then signed informed consent forms upon admission to ICU.
Diagnosis of CAP and SCAP
The clinical diagnosis of CAP was defined as the presence of a new infiltrate on the chest X-ray together with symptoms and signs of a lower respiratory tract infection in a patient who was not hospitalized or other healthcare facility in the previous 14 days (18,19). The symptoms and signs of a lower respiratory tract infection included: white blood cell (WBC) >10×109/L or <4×109/L, fever (>38 °C) or hypothermia (<36 °C), new cough with or without purulent sputum, chest discomfort or dyspnea and signs of consolidation of lung tissue (20).
SCAP was defined as CAP associated with the presence of the following one major or two or more minor criteria: major criteria (PH <7.30 and systolic blood pressure <90 mmHg) and minor criteria (age >80 years old, respiratory rate ≥30 breaths/min, blood urea nitrogen >30 mg/dL, PaO2/FiO2 ≤250, Multilobar/bilateral infiltrates and altered mental status) (21).
All patients were treated with standard antibiotic therapy according to British Thoracic Society guidelines (22).
Exclusion criteria
We excluded (I) age <65 years old; (II) patients with the evidence for diagnosis of hospital-acquired pneumonia, or who were admitted to the hospital in the previous 14 days, and the onset of pneumonia symptoms was beyond 48hrs after admission (23); (III) infiltrate on the chest X-ray followed by: obstructive pneumonia resulting from malignancy, pulmonary edema, pulmonary embolism, noninfectious pneumonia (e.g., lupus pneumonitis), and so on; (IV) patients with severe immunosuppression, such as human immunodeficiency virus (HIV) infection, neutropenia <1×109/L, and taking immune-suppressing drugs (24).
Introduction of scoring models
The CURB-65 scoring model developed by Dr. Lim, consists of five indexes: confusion, BUN >7 mmol/L, respiratory rate >30 breaths/min, systolic blood pressure <90 mmHg and/or diastolic blood pressure ≤60 mmHg, and age ≥65 yr. One point was allocated to each variable present and patients were stratified into different mortality risk groups (9).
PSI scoring model was introduced in 1997 following a multicenter study in over 50,000 inpatients and has a good ability of severity assessment. It consists of 20 variables in four categories including demographics, comorbidity, physical exam findings, and laboratory and radiographic findings. It results in five class point scoring systems reflecting an increasing risk of mortality (10).
APACHE II scoring model proposed by Dr. Knaus, uses a point score upon initial value of 12 routine physiologic measurements, age, and previous health status to provide a general measure of severity of disease (12).
Data collection
Clinical data of 240 elderly patients with CAP were collected and analyzed retrospectively, including the basic information (e.g., age, gender, and underlying diseases), diagnosis upon ICU admission, worst vital signs (e.g., temperature, breathing rate, heart rate, and blood pressure) and laboratory tests (e.g., proBNP, bilirubin, creatinine, and electrolytes, and so on) within 24 hours after admission to ICU, time of ICU stay, and the clinical outcomes. CURB-65, PSI, and APACHE II scores were calculated according to the above data. We measured NT-proBNP using a quantitative electrochemiluminescence immunoassay (Elecsys pro-BNP; Roche Diagnostic AG) according to the instructions of the kit manufacturer. The pathogens isolated and identified from sputum and/or bronchoalveolar lavage fluid (BALF) were recorded in the first three consecutive days after admission.
Outcomes measures
The primary clinical outcome of the study was observed including assessing severity, and predicting need for MV and 28-day mortality.
Statistical analysis
All data were analyzed using SPSS V.17 (SPSS, Inc., Chicago, Illinois, USA) for windows. Quantitative variables were expressed as mean ± standard deviation (SD) for normal distribution data and as medians (25th and 75th percentiles) for non-normal distribution data. Qualitative data were presented as frequencies and percentages. For continuous variables, the Student t-test was used to compare the data between the two groups and analysis of variance was employed to compare the three groups. The x2 tests were performed for qualitative variables. Receiver operating characteristic (ROC) curves were operated to evaluate candidate indicators with regards to the outcomes assessment of patients with CAP. Logistic regression analysis was performed to select the variables associated with the prognosis of patients. Two-side probabilities of less than 0.05 were regarded as statistically significant.
Results
General characteristics
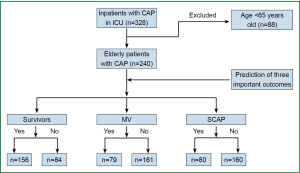
A total of 328 patients with CAP were admitted to EICU and RICU from Jan 2010 to April 2013 in our hospital. Of these, 88 patients were later excluded due to less than 65 yrs. The remaining 240 patients (73.2%), with the mean age of 75±8 years old, 143 (59.6%) male, were enrolled. Based on 28-day mortality, the 240 patients were grouped into 156 survivors (65%) and 84 non-survivors (35%); according to severity of the illness, these aged patients were divided into 80 SCAP patients (33%) and 160 non-SCAP (67%); based on need for MV, the enrolled patients were divided into 79 MV group (33%) and 161 non-MV group (67%) (Figure 1).
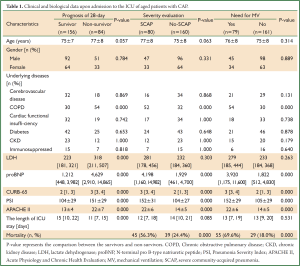
The demographic and biochemical data of the enrolled patients are summarized in Table 1. Admission levels of NT-proBNP, CURB-65, PSI, and APACHE II scores were significantly higher in non-survivors, SCAP patients, and MV group compared to 28-day survivors, non-SCAP patients, and no-MV group, respectively (P<0.001).The length of ICU stay was remarkable longer in survivors than that in non-survivors (P<0.001) but not in requirement of MV patients (P=0.531) and in diagnosis as SCAP (P=0.085). And there was statistical difference in the mortality between MV and non-MV and between SCAP and non-SCAP patients (P<0.001). Statistical difference was not marked on age and underlying diseases.
Full Table
Classification of pathogen
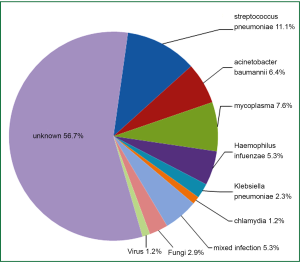
In an attempt to define which pathogen was the etiology of pneumonia, the pathogens were isolated and identified from sputum and/or BALF of the enrolled elderly patients with CAP. The etiology of CAP were classified into the following groups: (I) typical pathogens, such as streptococcus pneumoniae, Haemophilus influenzae, acinetobacter baumannii, and Klebsiella pneumoniae; (II) atypical pathogens, such as mycoplasma, chlamydia; (III) other pathogens, such as fungi, viral agents; (IV) unknown etiology. The incidence of the detected pathogens causing the elderly CAP is depicted in Figure 2.
Predictive value for three clinical outcomes in elderly CAP
Admission levels of proBNP, CURB-65, PSI, and APACHE II using receiver operator characteristic (ROC) curves for predicting 28-day mortality and need for MV, and severity assessment are shown in Figure 3.
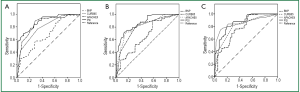
Admission NT-proBNP, CURB-65, PSI, and APACHE II were compared for these ability to predict three important clinical outcomes in Table 2. PSI had the highest area under the curve (AUC) and specificity for the three outcomes considered (AUC was 0.868, specificity was 0.906 for 28-day mortality; AUC was 0.864, specificity was 0.831 for requirement of MV; and AUC was 0.888, specificity was 0.894 for identifying SCAP).
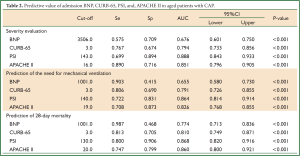
Full Table
NT-proBNP had the highest sensitivity of 0.987 but lowest specificity of 0.468 on prediction of mortality, while the highest sensitivity of 0.903 but lowest specificity of 0.415 on predicting need for MV. And APACHE II scoring model with the highest sensitivity of 0.890 was used to identify SCAP in Table 2.
Logistic regression analysis for the related factors affecting the prognosis of the elderly patients with CAP
Based on the 28-day mortality, the enrolled patients were divided into survival group and non-survival group. In logistic regression analysis, only three indicators were associated with the prognosis of the elderly patients suffering from CAP: systolic blood pressure, PSI and APACHE II scores, with the odd ratio (OR) values of 0.986, 1.249, and 1.019, respectively in Table 3.
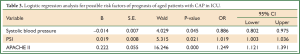
Full Table
Discussion
CAP is recognized as one of the main diseases in elderly people, frequently associated with sepsis and with high morbidity and mortality (25). Decreased immune function in seniors may be one of the leading causes to the development of CAP, which remains a serious and costly illness all over the world, including developed countries (26). Severity assessment is an increasing important component of the management of CAP to assist physicians in predicting outcome of the disease upon presentation to reduce CAP-related mortality (23). BNP has been documented as a reliable marker for identification of sepsis-induced myocardial depression and risk stratification and predict mortality for patients with CAP (15,17,27). And proBNP levels in plasma were found to predict short-term mortality in patients with CAP (28).
The present study documented that both plasma NT-proBNP and the three scoring models (CURB-65, PSI, and APACHE II) can evaluate severity, and predict need for MV and 28-day mortality. The PSI scoring models performed excellently in predicting the three clinical outcomes with the largest AUC and the highest specificity, and PSI has been confirmed as a powerful tool to classify and predict the mortality risk in patients with pneumonia from different population (10,22), but it does not allow for individual predictions, and easily to be affected by subjective judgment of doctors.
In our study, NT-proBNP levels were significantly higher in non-survivors, MV group, and SCAP patients compared to 28-day survivors, no-MV group, and non-SCAP patients, respectively, with the highest sensitivity but lowest specificity on prediction of mortality and need for MV in aged patients suffering from CAP, but it was inferior to PSI. This result was inconsistent with previous study. Dr. Kim documented that the performance of NT-proBNP was comparable to those of PSI and CURB-65 in predicting mortality of CAP (28).
Dr. Fine conducted a meta-analysis about the prognosis of CAP and proposed that the high mortality for hospitalized CAP may be related to its morbidity in those with different serious co-morbidities and the aged (11). In our study, only COPD existed difference with statistical significance between 28 survivors and non-survivors, but was not associated with prognosis by logistic regression analysis. Partly because this was a small sample size and single-center study leading to minor difference cannot detect, and partly because the enrolled patients’ condition were more severe when admitted to ICU covering the effect of age and underlying diseases on prognosis.
In our study, CURB-65 was documented to be less accurate than PSI and APACHE II scoring models. Nevertheless, as a moderate indictor to predict the three clinical outcomes of elderly patients with CAP, CURB-65 with the biggest advantage of its simplicity and handleability in comparison with the PSI and APACHE II, is for used in outpatients with CAP.
All the enrolled scoring systems contain admission blood pressure variable, which is considered to be associated with prognosis of patients with CAP. Hypotension is a positive factor for increasing mortality, and had been confirmed by fine using meta-analysis (11). The logistic regression analysis in our study pointed out systolic blood pressure was a protective factor for prognosis indicating that the higher systolic blood pressure is, the better the prognosis will be. Of course, the very high blood pressure is unfavorable to the prognosis. In additional, the PSI and APACHE II scores as risk factors for prognosis of elderly patients with CAP were proposed in the study. As effective indexes for assessing severity of disease, the more severe the disease, the higher the scores, and the patient’s condition is more imminent.
CAP as a sensitive and stimulating stressor to the cardiovascular system in aged through increased peripheral vascular resistance to increase cardiac workload. Additionally, some pro-inflammatory substances such as lipopolysaccharides, TNF-α, and even endotoxin, could decrease cardiac function by altering cardiac loading condition (29). ProBNP is vasoactive hormones secreted from cardiac myocytes, and its plasma levels increased with the extent of cardiac stress. So plasmas proBNP could be a more sensitive indicator for CAP-induced cardiac dysfunction, and will be a promising barker on prediction of mortality and need for MV, and severity evaluation in CAP patients. These findings should be validated by some larger multi-centers studies.
The strength of this study is that all the participants focused in our study were aged patients (≥65 years old), who had specific clinical features of their own. Through comparing the admission NT-proBNP, CURB-65 scores, PSI scores, and APACHE II scores, we found the four predictors were good at predicting the clinical outcomes of elderly patients suffering from CAP. And there was few studies about investigating admission proBNP on predicting 28-day mortality, and this is the firstly reported the value of proBNP in assessing the severity of CAP and predicting need for MV.
Admittedly, several objective factors should be considered in the interpretation of our study results: (I) study was based on the retrospective and observational design leading to ignore some low-influence factors; (II) the present study was conducted on relatively a less number of patients rather than large samples study. The small sample size in groups may be insufficient to detect minor difference; (III) the specific pathogens were isolated and detected from only 43.3% of aged patients with CAP, which restricted the full investigation of the pathogens in CAP. (IV) The overall mortality of enrolled patients with CAP was obviously higher (35%) than other CAP-related studies such as by Man in which the mortality of CAP was 8.6% (24). Different degrees of severity of the enrolled CAP patients can affect the results of study.
Conclusions
The level of plasma proBNP and three scoring models (CURB-65, PSI, and APACHE II) within 24 hrs after admission to ICU can make assessment of severity, and predict need for MV and 28-day mortality in the elderly patients with CAP, and PSI scores was the best predictor. CURB-65 score with the advantages of simplicity could help clinicians determine hospital or ICU admission or not for outpatients management. And physiological level of systolic blood pressure is the protection factor in prognosis. Further studies are required to confirm these results.
Acknowledgments
We express our gratitude to the nurses and doctors of EICU/RICU/SICU of the Chinese PLA General Hospital for help to this study.
Disclosure: The authors declare no conflict of interest.
References
- Brar NK, Niederman MS. Management of community-acquired pneumonia: a review and update. Ther Adv Respir Dis 2011;5:61-78. [PubMed]
- Marston BJ, Plouffe JF, File TM Jr, et al. Incidence of community-acquired pneumonia requiring hospitalization. Results of a population-based active surveillance Study in Ohio. The Community-Based Pneumonia Incidence Study Group. Arch Intern Med 1997;157:1709-18. [PubMed]
- Ramirez JA. Community-acquired pneumonia in adults. Prim Care 2003;30:155-71. [PubMed]
- Vila-Corcoles A, Ochoa-Gondar O, Rodriguez-Blanco T, et al. Epidemiology of community-acquired pneumonia in older adults: a population-based study. Respir Med 2009;103:309-16. [PubMed]
- Alvarez-Lerma F, Torres A. Severe community-acquired pneumonia. Curr Opin Crit Care 2004;10:369-74. [PubMed]
- de Castro FR, Torres A. Optimizing treatment outcomes in severe community-acquired pneumonia. Am J Respir Med 2003;2:39-54. [PubMed]
- Lee JC, Hwang HJ, Park YH, et al. Comparison of severity predictive rules for hospitalised nursing home-acquired pneumonia in Korea: a retrospective observational study. Prim Care Respir J 2013;22:149-54. [PubMed]
- Houck PM, Bratzler DW, Nsa W, et al. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med 2004;164:637-44. [PubMed]
- Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003;58:377-82. [PubMed]
- Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997;336:243-50. [PubMed]
- Fine MJ, Smith MA, Carson CA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA 1996;275:134-41. [PubMed]
- Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-29. [PubMed]
- Hunt PJ, Richards AM, Nicholls MG, et al. Immunoreactive amino-terminal pro-brain natriuretic peptide (NT-PROBNP): a new marker of cardiac impairment. Clin Endocrinol (Oxf) 1997;47:287-96. [PubMed]
- Talwar S, Squire IB, Davies JE, et al. Plasma N-terminal pro-brain natriuretic peptide and the ECG in the assessment of left-ventricular systolic dysfunction in a high risk population. Eur Heart J 1999;20:1736-44. [PubMed]
- Mueller C, Laule-Kilian K, Scholer A, et al. B-type natriuretic peptide for risk stratification in community-acquired pneumonia. J Intern Med 2005;258:391-3. [PubMed]
- Christ-Crain M, Breidthardt T, Stolz D, et al. Use of B-type natriuretic peptide in the risk stratification of community-acquired pneumonia. J Intern Med 2008;264:166-76. [PubMed]
- Nowak A, Breidthardt T, Christ-Crain M, et al. Direct comparison of three natriuretic peptides for prediction of short- and long-term mortality in patients with community-acquired pneumonia. Chest 2012;141:974-82. [PubMed]
- Ewig S, de Roux A, Bauer T, et al. Validation of predictive rules and indices of severity for community acquired pneumonia. Thorax 2004;59:421-7. [PubMed]
- Johnson PD, Irving LB, Turnidge JD. 3: Community-acquired pneumonia. Med J Aust 2002;176:341-7. [PubMed]
- Phua J, See KC, Chan YH, et al. Validation and clinical implications of the IDSA/ATS minor criteria for severe community-acquired pneumonia. Thorax 2009;64:598-603. [PubMed]
- España PP, Capelastegui A, Gorordo I, et al. Development and validation of a clinical prediction rule for severe community-acquired pneumonia. Am J Respir Crit Care Med 2006;174:1249-56. [PubMed]
- British Thoracic Society Standards of Care Committee. BTS Guidelines for the Management of Community Acquired Pneumonia in Adults. Thorax 2001;56 Suppl 4:IV1-64. [PubMed]
- Chalmers JD, Singanayagam A, Hill AT. Systolic blood pressure is superior to other haemodynamic predictors of outcome in community acquired pneumonia. Thorax 2008;63:698-702. [PubMed]
- Man SY, Lee N, Ip M, et al. Prospective comparison of three predictive rules for assessing severity of community-acquired pneumonia in Hong Kong. Thorax 2007;62:348-53. [PubMed]
- Watkins RR, Lemonovich TL. Diagnosis and management of community-acquired pneumonia in adults. Am Fam Physician 2011;83:1299-306. [PubMed]
- Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. JAMA 2004;291:1238-45. [PubMed]
- Post F, Weilemann LS, Messow CM, et al. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med 2008;36:3030-7. [PubMed]
- Jeong KY, Kim K, Kim TY, et al. Prognostic value of N-terminal pro-brain natriuretic peptide in hospitalised patients with community-acquired pneumonia. Emerg Med J 2011;28:122-7. [PubMed]
- Jianhui L, Rosenblatt-Velin N, Loukili N, et al. Endotoxin impairs cardiac hemodynamics by affecting loading conditions but not by reducing cardiac inotropism. Am J Physiol Heart Circ Physiol 2010;299:H492-501. [PubMed]