Is ischemic postconditioning in STEMI worth pursuing?
We have, with interest, read the editorial on our study DANAMI-3–iPOST (1) and do agree on most of the aspects touched upon. We do, however, want to add to the editorial by raising a few points.
The concept of conditioning in addition to primary PCI faces a number of challenges. The time from symptom to reperfusion has decreased dramatically over the years, in DANAMI-3 it was median 2.7 hours. Thus, in a contemporary setting, many patients suffer small infarcts and consequently any additional treatment modality on top of primary PCI may not add to the clinical outcome. On the other hand, the conditioning agent exenatide was most efficient to protect against reperfusion injury in early comers STEMI patients (2). Still, it will be difficult to prove clinical benefit of a new modality if the event rate a priori is low.
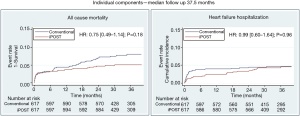
Hazard ratio for all-cause death in favor of iPOST was 0.75 (P=0.18) in DANAMI-3–iPOST and thus the authors may be correct that we were facing a power problem. Of interest the Kaplan Meyer curves for heart failure hospitalization diverge very early but end up being superimposed after 3 years. Kaplan Meyer curves for all-cause mortality diverge after approximately 6 months and continue so—though without reaching statistical significance (Figure 1). However, censoring of patients after hospitalization for heart failure leave them out of consideration for subsequent death. The cohort will be followed-up and 5-year data reported.
The translation of cardio protection in animal studies into a clinical setting is complicated by the fact that animal models do not face real thrombus formation but merely ligation of a coronary artery with subsequent ischemia and reperfusion. Thus, if reperfusion injury in human is caused by peripheral embolization to a certain extent, iPOST will not work. Further, any potential effect will depend on the conditioning protocol including the length and number of occlusions. Our protocol (30 sec/30 sec) was based on our proof-of-concept trial in which this algorithm was used (3). Staat et al. did, however, use a 60 sec/60 sec protocol in the first human trial (4).
We believe that any future attempt to design a trial to prove iPOST efficacious should address some important issues. Thus, the population should probably be enriched (large area at risk, short duration of symptoms) and confounders should be eliminated (competing diseases including old age). In addition, the iPOST protocol should comply with the demand that iPOST must for certain be instituted prior to prolonged reperfusion and without causing peripheral embolization. Finally, the clinical endpoint should be sufficiently hard to be meaningful and therefore the number of patients larger than in DANAMI-3–iPOST.
Acknowledgements
We acknowledge the DANAMI3 study Group.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Engstrøm T, Kelbæk H, Helqvist S, et al. Effect of ischemic postconditioning during primary percutaneous coronary intervention for patients with st-segment elevation myo-cardial infarction: a randomized clinical trial. JAMA Cardiol 2017;2:490-7. [Crossref] [PubMed]
- Lønborg J, Kelbæk H, Vejlstrup N, et al. Exenatide reduces final infarct size in pa-tients with ST-segment-elevation myocardial infarction and short-duration of ischemia. Circ Cardiovasc Interv 2012;5:288-95. [Crossref] [PubMed]
- Lønborg J, Kelbaek H, Vejlstrup N, et al. Cardioprotective effects of ischemic post-conditioning in patients treated with primary percutaneous coronary intervention, evaluated by magnetic resonance. Circ Cardiovasc Interv 2010;3:34-41. [Crossref] [PubMed]
- Staat P, Rioufol G, Piot C, et al. Postconditioning the human heart. Circulation 2005;112:2143-8. [Crossref] [PubMed]


