Emergency drain for post pneumonectomy bronchopleural fistula: a drain placement technique based on the siphon principle
Introduction
Bronchopleural fistula (BPF) after pneumonectomy is a life-threatening complication occurring in 2% to 16% of patients (1,2). Diagnosis of BPF should be prompt and is usually obtained with fiberoptic bronchoscopy and CT scan. After diagnosis, the first step is to drain the pleural cavity from the infected effusion (empyema), to prevent hypertensive mediastinal shift and aspiration pneumonia. It may be difficult to safely and correctly perform this manoeuvre because of: (I) the drastic change in anatomy following pneumonectomy, with diaphragm raising and mediastinal shift; (II) the need to drain the lowest part of the cavity effectively by the inserted drainage tube, whose tip should ideally be positioned in the deepest part of the chest (3,4).
Several chest tube placement techniques are available to the surgeons who prefer one or another depending on experience, skill and availability of radiologic devices (ultrasounds-CT guided etc.). We herewith describe our technique of chest tube thoracostomy in case of a BPF, based upon the siphon principle.
Operative techniques
The aim of this technique is to drain the lowest part of the pleural cavity effectively avoiding mediastinal, diaphragmatic or intra-abdominal organ injuries (Figures 1-3).
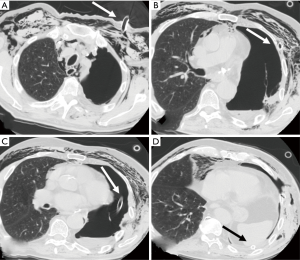
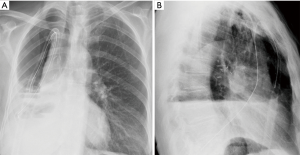
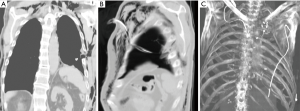
After an exploratory puncture with local anaesthetic, a skin incision in the 2nd or 3rd intercostal space in the hemiclavear line is made; then, by means of curved Klemmer forceps, the drain is inserted and tunnelled through the 3rd or 4th intercostal space (Figure 1A,B; Figure 3B,C). This allows the drain to be safely directed to the lowest part of the cavity, passing distal to mediastinal and diaphragmatic structures (Figure 1C,D). The drain is thus fixed to the skin by a standard purse string suture and the wound medicated with a cylindrical pack of gauzes under the tube, on the skin, to avoid the chest tube kinking. A chest X-ray performed after the procedure allows a proper identification of the tips’ end and its potential repositioning if not adequately lodged in the costophrenic sinus. In order to obtain an adequate drainage, at least a 24 gauge (Ch) chest tube is recommended.
Comments
Requirements to treat a post pneumonectomy empyema include an early drainage of the intrathoracic space, closure of the BPF and creation of an open thoracostomy, which is usually packed with medicated swabs and, eventually, closed (5-7). Rarely, the drain alone is sufficient to allow the fistula to close by itself; however, a conservative management of the BPF has shown to be effective in case of small fistulae (8). Furthermore, drainage of the empyema through chest tube alone, not followed by an open window thoracostomy, may be an appropriate compromise to those impaired patients who, due to their condition, (compromised lung function tests, limited cardiopulmonary reserve, impaired general condition, early cancer recurrence, chest wall deformities such as scoliosis, small fistulas, etc.) may not withstand it.
The need of early chest cavity drainage is mandatory to prevent a mediastinal hypertensive shift and contralateral inhalation pneumonia. However, cardiac dislocation, diaphragm and abdominal organ raising and massive subcutaneous emphysema could make this manoeuvre hazardous and unsafe.
In addition, the tip of the drainage tube should be positioned in the deepest part of the cavity where secretions and potentially infected fluid may stagnate. The main advantage of the proposed technique is to drain the deepest part of the pleural cavity, entering the chest in a safe position distal to mediastinal, vascular, diaphragmatic and abdominal structures (Figure 1C).
Our technique is based on the so-called “siphon principle”: a siphon is a continuous tube that allows liquid to drain from a reservoir (chest cavity) through an intermediate point (insertion point of the drainage tube on the skin) located higher than the reservoir, the flow (pleural fluid) being driven only by the difference in hydrostatic pressure without the need of a pump. The end tip of the tube (the collection chamber) must be lower than the liquid surface in the reservoir (9).
This technique also permits an even irrigation and drainage of the chest cavity by means of another small apical tube (Figure 2A), in order to improve the cavity drainage, cleansing and obtain control of the empyema.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent obtained at admission of the patient.
References
- Deschamps C, Bernard A, Nichols FC 3rd, et al. Empyema and bronchopleural fistula after pneumonectomy: factors affecting incidence. Ann Thorac Surg 2001;72:243-7; discussion 248. [Crossref] [PubMed]
- Borri A, Leo F, Veronesi G, et al. Extended pneumonectomy for non-small cell lung cancer: morbidity, mortality, and long-term results. J Thorac Cardiovasc Surg 2007;134:1266-72. [Crossref] [PubMed]
- Filosso PL, Guerrera F, Sandri A, et al. Errors and Complications in Chest Tube Placement. Thorac Surg Clin 2017;27:57-67. [Crossref] [PubMed]
- Filosso PL, Sandri A, Guerrera F, et al. Management of Chest Drains After Thoracic Resections. Thorac Surg Clin 2017;27:7-11. [Crossref] [PubMed]
- Zanotti G, Mitchell JD. Bronchopleural Fistula and Empyema After Anatomic Lung Resection. Thorac Surg Clin 2015;25:421-7. [Crossref] [PubMed]
- Zahid I, Routledge T, Billè A, et al. What is the best treatment of postpneumonectomy empyema? Interact Cardiovasc Thorac Surg 2011;12:260-4. [Crossref] [PubMed]
- Vallières E. Management of empyema after lung resections (pneumonectomy/lobectomy). Chest Surg Clin N Am 2002;12:571-85. [Crossref] [PubMed]
- Boudaya MS, Smadhi H, Zribi H, et al. Conservative management of postoperative bronchopleural fistulas. J Thorac Cardiovasc Surg 2013;146:575-9. [Crossref] [PubMed]
- Ganci S, Yegorenkov V. Historical and pedagogical aspects of a humble instrument. Eur J Phys 2008;29:421-30. [Crossref]


