Massive pericardial effusion after Nuss procedure: to drain or not to drain?
Introduction
Fever, dyspnoea and leukocytosis after Nuss procedure are usually attributed to post-operative atelectasis, pneumonia, or prosthetic infection. However, the features may also be the result of post-pericardiotomy syndrome (PPS), a rare complication normally associated with pericardial trauma, particularly in the face of febrile pericardial effusion unresponsive to antibiotics. We present a case of massive febrile pericardial effusion after Nuss procedure, with rapid clinical improvement and resolution of pericardial effusion after a therapeutic trial of corticosteroid administration.
Case presentation
A 11-year-old boy developed gradual worsening of pectus excavatum during follow-up for his history of open right upper lobectomy for congenital pulmonary airway malformation. Correction of pectus excavatum was indicated in view of Haller’s index of 4.7, and significantly compromised lung function [forced expiratory volume at 1st second (FEV1): 58.7% predicted; FEV1/FVC (forced vital capacity): 79.9% predicted].
Following adhesiolysis of the complete right pleural symphysis, standard Nuss procedure was performed using a 11.5-inch stainless steel bar entered and tunnelled from the right chest. The steel bar achieved good conformation to the chest wall, and was anchored with left sided stabilizer, and subsequently secured to the chest wall with polyester sutures. The total operative time was 105 minutes. His early post-operative course was uneventful, and the chest drain was removed on the third post-operative day.
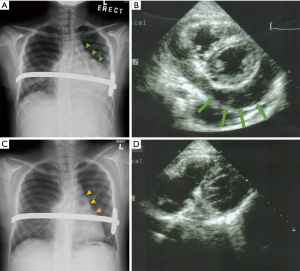
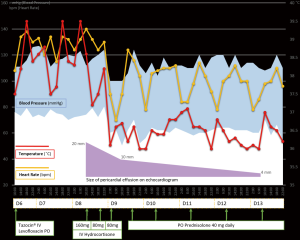
However, he developed a high swinging fever on the fifth post-operative day with increasing serum inflammatory markers (white blood cell count 13.0×109/L, C-reactive protein 186.8 mg/L), which was not responsive to intravenous broad-spectrum antibiotics. Blood, urine and sputum cultures yielded no organisms. Upon subsequent deterioration in clinical condition with desaturation and tachycardia, an urgent contrast computer tomography scan of the thorax was done under intravenous hydrocortisone cover for his history of asthma, and showed pericardial thickening and a large amount of pericardial effusion, as well as moderate bilateral pleural effusion. Echocardiogram revealed massive pericardial effusion up to 20 mm thickness with no evidence of pericardial tamponade or haemopericardium (Figure 1). Emergency subxiphoid pericardial window creation was initially contemplated, but was cancelled as patient showed rapid improvement in pyrexia and tachycardia during the 6-hourly doses of intravenous hydrocortisone following computed tomography (Figure 2). Repeat echocardiogram showed decreasing pericardial effusion. White cell count and C-reactive protein also showed steep decreasing trend. He received a short course of oral prednisolone 40 mg daily. A follow-up echocardiogram 6 days after steroid therapy also revealed resolving pericardial effusion to only 4 to 6 mm thickness (Figure 1). He was discharged on post-operative day 14 and subsequent echocardiogram was unremarkable.
Discussion
Development of pericardial effusion is an uncommon complication after Nuss procedure, and the reported incidence was only up to 2.4% (1). Serious pericardial effusion with pericardial tamponade was rarely reported, and may represent delayed presentation of bar displacement, cardiac or major vessel injury such as the aorta (2), and PPS (3).
PPS is more commonly known as a complication after surgery which involved opening of the pericardium, and affects up to 40% patients after cardiac surgery. As the placement of Nuss bar requires tunnelling across the anterior mediastinum, the pericardium may be irritated during the course of bar insertion due to traction, pressure or even inadvertent puncture. These may trigger aseptic inflammation of the pericardium, and develop into PPS. Pericardial effusion accompanying PPS may present in the early or late post-operative period (4), or can even cause recurrent cardiac tamponade. When suboptimally treated, pericardial constriction requiring pericardiectomy may be the sequel in up to 13% cases (5).
PPS is usually a febrile disease associated with leucocytosis and elevated inflammatory markers which can mimic and be mistaken as post-operative infections of the lung, wound or prosthesis. Poor response to intravenous antibiotics and negative septic work-up should effectively exclude prosthetic infection. An increasingly enlarging or globular cardiac shadow on chest X-ray (CXR) and effusion should alert clinician to obtain early echocardiographic examination. Absence of haemopericardium decreases likelihood of major vessel or organ injury, and should lead to a raised suspicion of PPS. As PPS can be highly and rapidly responsive to corticosteroids, early administration of corticosteroids can serve as a therapeutic trial, to prevent pericardial tamponade, and avoid the risk of invasive pericardial drainage by pericardiocentesis, percutaneous balloon pericardiotomy or surgical creation of pericardial window, when there are no obvious septic foci. Empirical use of acetylsalicylic acids, non-steroidal anti-inflammatory drugs and colchicine lacks clinical evidence to support their effectiveness in the current clinical context. As therapeutic trial of corticosteroids cannot guarantee success for every case, it is important to be vigilant of non-responders, to monitor for worsening of haemodynamic parameters, and to perform pericardial drainage promptly.
In conclusion, PPS is an uncommonly reported and diagnosed complication with potentially serious consequences following Nuss procedure, mandating a high index of suspicion. An early therapeutic trial with corticosteroids may be attempted to achieve potential rapid clinical improvement and avoidance of invasive procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Nuss D, Croitoru DP, Kelly RE Jr, et al. Review and discussion of the complications of minimally invasive pectus excavatum repair. Eur J Pediatr Surg 2002;12:230-4. [Crossref] [PubMed]
- Hoel TN, Rein KA, Svennevig JL. A life-threatening complication of the Nuss procedure for pectus excavatum. Ann Thorac Surg 2006;81:370-2. [Crossref] [PubMed]
- Muensterer OJ, Schenk DS, Praun M, et al. Postpericardiotomy syndrome after minimally invasive pectus excavatum repair unresponsive to nonsteroidal anti-inflammatory treatment. Eur J Pediatr Surg 2003;13:206-8. [Crossref] [PubMed]
- Russo AM, O'Connor WH, Waxman HL. Atypical presentations and echocardiographic findings in patients with cardiac tamponade occurring early and late after cardiac surgery. Chest 1993;104:71-8. [Crossref] [PubMed]
- Alraies MC, Al Jaroudi W, Shabrang C, et al. Clinical features associated with adverse events in patients with post-pericardiotomy syndrome following cardiac surgery. Am J Cardiol 2014;114:1426-30. [Crossref] [PubMed]


