Comparison of closed-chest drainage with rib resection closed drainage for treatment of chronic tuberculous empyema
Introduction
Although a number of anti-tuberculosis (anti-TB) drugs have been used to cure tuberculosis, it is still being the main cause of death from a curable infectious disease (1,2). The prevalence of active pulmonary tuberculosis, smear positive pulmonary tuberculosis and bacteriological positive pulmonary tuberculosis in 2000 was 367 per 100,000 population, 122 per 100,000 population and 160 per 100,000 population in China, respectively (3). As a complication of tuberculosis, pleural tuberculosis also has a relatively high prevalence (4). Pleural tuberculosis is caused by Mycobacterium tuberculosis (5). Inflammation of the pleura usually is related to the development of delayed-type hypersensitivity against tubercle bacilli located on or near the pleural surface (6). In addition, if the treatment is not timely, tuberculous pleural proceed to a chronic, active infection of the pleural tuberculosis, which is named as chronic tuberculous empyema. Chronic tuberculous empyema, which is infected with Mycobacterium tuberculosis, anaerobic bacteria, Staphylococcus aureus, Streptococcus pneumoniae and other kinds of gram-negative bacteria, can induce inflammation and infection (7). These infections cause thickening, even calcification of the visceral and parietal pleura. It is difficult for anti-TB drugs to enter the abscess cavity, as well as pus become thick and dense, meanwhile, the deep vein diameter is small and easy to plug, so chronic tuberculous empyema is hardly cured (6).
In view of the effect of simple medical treatment is poor, chronic tuberculous empyema is generally treated by surgery. Surgery, which is challenging, should be conducted by experienced thoracic surgeons. At present, the surgical treatment for chronic tuberculous empyema includes intercostal chest drain (8-10), rib resection drainage (11) and fibreboard stripping surgery (12-14). Although the study has reported that the fibreboard stripped surgery has a significantly effect on treatment of patients with chronic tuberculous pyothorax, while fibreboard stripping surgery is difficult and sometimes required thoracic surgery or muscle flap to eliminate dead space (15,16). In addition, the fibreboard stripping surgery is more expensive and more painful for patients.
The intercostal chest drain is different from the rib resection drainage. During the process of rib resection drainage, the periosteum of the ribs is cut, and 4–5 cm of rib need to cut (11). However, intercostal chest drain is performed in intercostal but not on rib (9). It is not necessary to remove the ribs, and directly place the tube from the intercostal incision, as well the tube diameter of intercostal chest drain can be quite with that through rib resection drainage (10). Furthermore, surgical incision of intercostal drain is small, so the physician can operate in the ward treatment room. However, in recent years, some studies have shown that complications are induced by intercostal chest drain (9,10). Therefore, the efficacy of intercostal closed chest drain and rib resection closed drainage to cure the chronic tuberculous empyema is still a controversial topic.
In this study, intercostal closed chest drain and rib resection closed drainage were used to cure the 86 patients with tuberculous empyema, respectively. We aimed to compare the efficacy of intercostal closed chest drain and rib resection closed drainage on patients with tuberculous empyema.
Methods
Patients
This study retrospectively reviewed 86 patients with tuberculous empyema in Tuberculosis Treatment Center, Shanghai Pulmonary Hospital, Tongji University (Shanghai, China) between August 2010 and November 2015. Of the 86 patients, 22 cases who received closed-chest drainage were acted as the study group, meanwhile, 64 cases who received rib resection closed drainage were served as the control group. Patients who had diabetes, cardiovascular, blood and other complications were excluded in this study because of different etiology and disease process. This study was approved by the ethical committee of Clinic and Research Center of Tuberculosis, Shanghai Key Lab of Tuberculosis, Shanghai Pulmonary Hospital, Tongji University School of Medicine (No. K17-162).
Diagnostic criteria
The tuberculous empyema was diagnosed according to following criteria: (I) patients had significant symptoms, for instance, fatigue, low heat, night sweats, chest tightness, dry cough; (II) the patient had a history of TB or tuberculous pleurisy and the corresponding signs, and erythrocyte sedimentation at the fast rate, as well as without effective anti-TB treatment; (III) the characteristic of pleural effusion was purulence, ropiness, containing caseous material. There was no bacteria growth on common medium, but when pleural effusion was observed by mycobacterium smear or culture, the results showed positive or negative. The total number of pus cells was more than 10×109/L, among these cells, mostly were lymphocytes with protein content >40 g/L and specific gravity >1.020 (17); (IV) imaging findings showed a typical performance of chronic tuberculous empyema, including pleural thickening of parietal, calcification, the liquid dark area between parietal pleural, and extrapleural fat layer density increase (18).
Treatment method
Treatment of chronic tuberculous empyema with closed-chest drainage
All patients were given systemic anti-TB treatment. At the same time, local pyothorax was treated by closed thoracic drainage under local anesthesia. Firstly, B-ultrasound examination was performed for accurate positioning. Then B-ultrasound combined with chest computed tomography (CT), pleural thickness was measured. Next, a 1.5 cm-long incision was made in the chest wall skin along the long axis of the ribs, and then subcutaneous tissue and muscle as well as parietal pleura and fibrous board were separated. Moreover, according to the width of the intercostal space, the needle chest tube [specification of tube: 5.33 mm (16 Fr) × 360 mm, 6.67 mm (20 Fr) × 360 mm, or 8 mm (24 Fr) × 360 mm; Pacific Hospital Supply Co. Ltd, Shanghai, China] was inserted, and the needle core was pulled out, while the drain tube was left in the chest cavity. Finally, the drain tube was connected into the water bottle, and the incision was sutured to prevent the slippage of drain tube. The negative pressure derived from 20 cmH2O continuous was used to attract pleural effusion. In addition, patients took the lip reduction exercise for 1 h every day during catheterization.
Extubation indications: pleural fluid drain was less than 50 mL for 3 consecutive days, and there was no fluctuation in water seal bottle, at the same time chest X-ray or chest CT showed the compressed lung tissue stretched again (19).
Treatment of chronic tuberculous empyema with the closed rib resection drainage
Forty-five-degree semi-recumbent position was applied in survey, and rib resection closed drainage was usually operated by surgeons in our hospital. Incision was located at the bottom of the abscess cavity by chest X-ray or chest CT. Under general anaesthesia, a 4–5 cm-long incision along with rib cage was made. Then the chest wall muscle was cut and exposed the ribs, instantly cut the periosteum, subsequently, cut off 3 cm long ribs. So, the abscess cavity was opened, and a closed large-bore chest tube [Specification of tube: 4.67 mm (F14)-12.00 mm (F36) × 450 mm, Suzhou Weikang Medical Apparatus Co., Ltd., Suzhou, Jiangsu, China] was placed in abscess cavity. Finally, the water bottle was connected with the drain tube, and the incision was sutured.
Efficacy evaluation criteria
The treatment efficacy of patients was determined by clinical symptoms and imaging, which was divided into 5 levels. Recovery: clinical symptoms and the abscess disappeared or disappeared, and imaging showed pleural effusion completely was absorbed; significantly curative effect: clinical symptoms disappeared, and imaging showed that the narrow of abscess was more than 2/3; partly curative effect: symptoms relieved and imaging showed that the narrow of abscess was more than 1/3 but less than 2/3; negative effect: there was no decreased or even aggravation of patient symptoms, and imaging showed the narrow of abscess was less than 1/3; recurrence: abscess narrowed or disappeared after treatment, but abscess increased again after extubation, and the patient symptoms appeared recurrence. All patients were examined during 1-year follow-up time.
Statistical analysis
Data was analyzed using SPSS software (version 19.0, Chicago, IL, USA). Enumeration data were presented as percentage and analyzed by χ2 test, and measurement data were presented as mean ± standard deviation (SD) and analyzed by t-test. P value ≤0.05 was considered statistically significant.
Results
Patient characteristics
Totally, 86 patients received closed thoracic drainage. Among these 86 patients, 22 patients (17 men and 5 women) received closed-chest drainage, while 64 patients (55 men and 9 women) received closed rib resection drainage. The mean age of 22 patients in study group was 33.86±13.10 years (range, 19.00–60.00 years), and the mean age of 64 patients was 40.05±12.50 (range, 18.00–64.00 years). Meanwhile, there was no significant difference in gender and age between the study and control groups (Table 1). In addition, we found that the location of ten patients’ abscess cavity was on left, 11 patients’ location was on right and only one patient on both sides in the closed-chest drainage group. In the rib resection closed drainage group, the abscess cavities of 30 patients were on left, 33 patients were on right, and one patient on both sides.
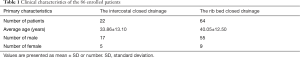
Full table
Effectiveness
A total of 86 cases were successfully received closed thoracic drainage. In the study group (22 patients), the average catheterization time was 126.14±36.84 days, however, the average catheterization time in control group (64 patients) reached 130.05±13.12 days via the closed rib resection drainage. Among them, 2 (9.09%) patients in the study group, 9 (14.06%) patients in the control group, whose clinical symptoms disappeared and pleural effusion completely absorbed, were successfully cured and recovery. Clinical symptoms disappeared, 13 (59.09%) patients in the study group, 31 (48.44%) patients attained a significant curative effect. Meanwhile, 6 (27.27%) patients and 19 (29.69%) patients in study and control groups, respectively, whose symptoms eased and abscess narrowed more than 1/3 but less than 2/3, reached to partly curative effect. However, the treatment effect of 1 (4.55%) patient in study group and 5 (7.81%) patients in control group was negative (Table 1). In the course of surgery, pus pneumothorax was found one case in study group and three cases in control group. In addition, these two surgical methods were both minimally debridement, so the intraoperative blood loss was only a small amount. Furthermore, there were no complications (such as pneumothorax, hemothorax) after surgery in both two groups. There was no significant difference in the curative effect of closed-chest drainage and rib resection closed drainage in the treatment of chronic tuberculous empyema (Table 2, P>0.05), while the average catheterization time of rib resection closed drainage (130.05±13.12 days) was significant longer than that (126.14±36.84 days) in course of closed-chest drainage (P<0.05).
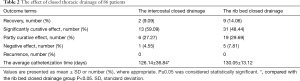
Full table
Two special cases
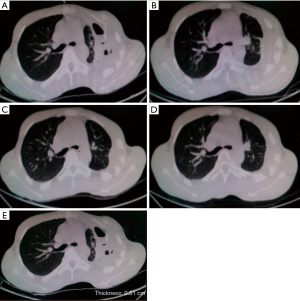
Case 1
A 19-year-old man had clinical symptoms, such as cough, sputum, chest tightness and chest pain. External chest CT showed that left abscess had pleural effusion, and he was diagnosed as left tuberculous empyema. On September 21, 2010, he was in hospital and received closed-chest drainage treatment under local anesthesia, and the tube was extubated after 133 days.
The changes in the chest of patient and pleural thickness were shown and measured by CT (Figure 1), and the obvious difference was observed between after catheterization for 1 week (Figure 1A; September 29, 2010) and after extubation for 10 months (Figure 1D; December 14, 2011). The abscess was narrowed more than 2/3 after extubation for 3 weeks (Figure 1B; February 23, 2011). The abscess almost disappeared after extubation for 6 months (Figure 1C; August 17, 2011), and the abscess completely disappeared after extubation for 10 months (Figure 1D; December 14, 2011). The thickness of pleura (after catheterization for 1 week) was 0.51 cm (Figure 1E).
Case 2
A 19-year-old man was diagnosed with left tuberculous empyema. Under local anesthesia, he received closed-chest drainage treatment. Silicone drain tube was inserted about 6-cm depth, and was connected into the water bottle On February 23, 2011. After 69 days, the tube was extubated on May 2, 2011. The CT showed the changes of chest between prior to admission and after extubation for 8 months (Figure 2A-D). Meanwhile, pleural thickness of patient was presented in Figure 2E two weeks after catheterization.
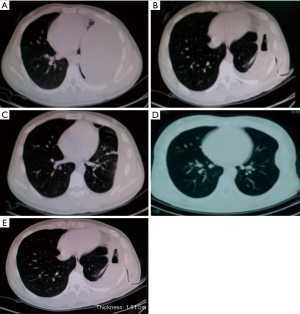
As shown in Figure 2A (February 12, 2011), the abscess was clearly observed, while the abscess was narrowed more than 1/3 after catheterization for 2 weeks (Figure 2B; March 9, 2011). The abscess almost disappeared after extubation for 3 weeks (Figure 2C; May 23, 2011), and completely disappeared after extubation for 8 months (Figure 2D; January 17, 2012). The thickness of pleura was 1.51 cm (Figure 2E) indicating that the closed-chest drainage had a good effect on this patient.
Discussion
Tuberculous empyema is an infection of the pleural cavity by Mycobacterium tuberculosis that provokes the accumulation of purulent pleural fluid (20). Tuberculous empyema usually occurs in younger (21) middle-aged (22,23) patients. The diagnosis of tuberculous empyema is depended on CT imaging by finding a thick, calcific pleural rind and rib thickening surrounding loculated pleural fluid (24).
It had been reported that the degree of pleural fibrosis of tuberculous empyema was higher than that of other bacterial empyema (25). Meanwhile, the treatment effect of chronic tuberculous empyema was poor (19). In addition, some scholars thought that tuberculous empyema could not be completely cured by internal medicine, and the fibrous empyema only could be cured by surgery. Studies revealed that the pleural thickness could influence the choice of treatment for tuberculous empyema, and the pleural thickness of 1.0 cm could be used as the cut-off value to choose internal drainage or surgical operation (26,27). However, a number of studies showed that the internal diameter of the indwelling catheter in internal drainage was related to the efficacy of treatment. Meanwhile, they suggested that the use of image guided small bore catheters could have a good outcome, therefore, it was acted as a primary drainage procedure or a rescue treatment when larger tubes had failed (28-32). Therefore, we thought that the thickness of pleural should not be considered as only one factor for surgery or not.
In this study, closed-chest drainage and rib resection closed drainage were used to cure tuberculous empyema. The results showed that after closed-chest drainage treatment, 2 (9.09%) patients were recovery, 13 (59.09%) patients had significantly curative effect, 6 (27.27%) patients had partly curative effect, 1 (4.55%) patient was negative effect, and there was no patient recurrence during 1-year follow-up time. Meanwhile, they attained a better outcome on patients with no complications via closed-chest drainage, which were not consistent with the Kong’s (9) and Harris’s (10) studies because of the difference of included case, and there is higher rate of complications in Kong’s study (9). In addition, the average catheterization time was 126.14±36.84 days, which was longer than that of Kundu’s study (19). In Kundu’s study, the observation time was set for 1 day before extubation, while in our study, more stringent indications for extubation and 3 days were set for observation before extubation based on the principle that pus should be drained clean as far as possible.
Similar to the results of closed-chest drainage treatment, after closed rib resection drainage, 9 (14.06%) patients were successfully recovery, 31 (48.44%) patients were significantly curative effect, 19 (29.69%) patients had partly curative effect, and 5 (7.81%) patients had negative effect. These results suggested that closed-chest drainage both the closed-chest drainage and rib resection closed drainage had a good outcome on patients with tuberculous empyema. The closed-chest drainage was entirely operated by physician and as well as could greatly reduce the pain and economic costs of patients. However, rib resection drainage needed to cut 4–5 cm rib and got greatly pain for patients. Furthermore, the catheterization time in rib resection closed drainage was longer than that in closed-chest drainage. Therefore, closed-chest drainage maybe superior to rib resection drainage for the treatment of chronic tuberculous empyema.
However, our study had some limitations. First, the included patients, whose average age was only 33.86 years old, were relatively young. While for older patients, because of its poor tolerance, closed-chest drainage was not recommended. Second, this study only suggested that closed-chest drainage had a short-term effect, but its long-term effect should be further investigated.
In conclusion, the closed-chest drainage, compared to rib resection closed drainage, had a better outcome and more advantages for young patients with tuberculous empyema in the short-term.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethical Committee of Clinic and Research Center of Tuberculosis, Shanghai Key Lab of Tuberculosis, Shanghai Pulmonary Hospital, Tongji University School of Medicine (No. K17-162).
References
- Dye C. Global epidemiology of tuberculosis. Lancet 2006;367:938-40. [Crossref] [PubMed]
- Bartu V, Kopecka E. Situation of multidrug-resistant tuberculosis in the Czech Republic, unusual case study. Respir Med CME 2009;2:185-8. [Crossref]
- National Technic Steering Group Of The Epidemiological Sampling Survey For Tuberculosis. Duanmu H. Report on fourth national epidemiological sampling survey of tuberculosis. Zhonghua Jie He He Hu Xi Za Zhi 2002;25:3-7. [PubMed]
- Conde MB, Loivos AC, Rezende VM, et al. Yield of sputum induction in the diagnosis of pleural tuberculosis. Am J Respir Crit Care Med 2003;167:723-5. [Crossref] [PubMed]
- Magness DJ. Empyema necessitans caused by Mycobacterium tuberculosis in an immunocompetent patient. WMJ 2013;112:129-30. [PubMed]
- Iseman MD, Madsen LA. Chronic tuberculous empyema with bronchopleural fistula resulting in treatment failure and progressive drug resistance. Chest 1991;100:124-7. [Crossref] [PubMed]
- Kim DJ, Im JG, Goo JM, et al. Chronic tuberculous empyema: relationships between preoperative CT findings and postoperative improvement measured by pulmonary function testing. Clin Radiol 2005;60:503-7. [Crossref] [PubMed]
- Reddy JB, Kilim SR. A Study on Tuberculous Empyema Thoracis in Children. J Evolut Med Dent Sci 2015;4:2330-4. [Crossref]
- Kong VY, Oosthuizen GV, Sartorius B, et al. An audit of the complications of intercostal chest drain insertion in a high volume trauma service in South Africa. Ann R Coll Surg Engl 2014;96:609-13. [Crossref] [PubMed]
- Harris A, O'Driscoll BR, Turkington PM. Survey of major complications of intercostal chest drain insertion in the UK. Postgrad Med J 2010;86:68-72. [Crossref] [PubMed]
- Huh JP, Lee JC, Jung TE, et al. Surgical treatment of loculated empyema: closed rib resectional drainage. Korean J Thorac Cardiovasc Surg 1998;31:1063-9.
- Ning XZ, Xia ZH, Wang HJ. The application effect and the safety analysis of pleural fibreboard stripped in chronic tuberculous pyothorax. China Modern Medicine 2014;(16).
- He F, Li YH, Wang XY. Timing of pleural fibreboard endarterectomy surgical treatment on chronic tuberculous empyema. J Clin Pulm Med 2010;15:1254-5.
- Xu X, Yang H. The analysis of the treatment of chronic tuberculous empyema by using stripped pleural fibreboard. J Clin Pulm Med 2002;7:10-1.
- Okumura Y, Takeda S, Asada H, et al. Surgical results for chronic empyema using omental pedicled flap: long-term follow-up study. Ann Thorac Surg 2005;79:1857-61. [Crossref] [PubMed]
- Chen YW, Zhang Z, Liao YD, et al. Investigation of vascular pedicle muscle flap intrathoracic filling in the treatment of chronic tuberculous encapsulated empyema. J Clin Pulm Med 2014;19:1835-7.
- Crofton J, Horne N, Miller F. Clinical tuberculosis. London, UK: Palgrave Macmillan, 1992. NCID: BA29830681.
- Shim SS, Kim Y. CT findings in Differential Diagnosis between Tuberculous Pleurisy and Malignant Effusion. ESTI 2012 meeting; June 22-24; London/UK. ESTI, 2012:E-0084.
- Kundu S, Mitra S, Mukherjee S, et al. Adult thoracic empyema: A comparative analysis of tuberculous and nontuberculous etiology in 75 patients. Lung India 2010;27:196-201. [Crossref] [PubMed]
- Ferrer J. Tuberculous pleural effusion and tuberculous empyema. Semin Respir Crit Care Med 2001;22:637-46. [Crossref] [PubMed]
- Goldschlager T, Frawley G, Crameri J, et al. Comparison of thoracoscopic drainage with open thoracotomy for treatment of paediatric parapneumonic empyema. Pediatr Surg Int 2005;21:599-603. [Crossref] [PubMed]
- Liu YH, Lin YC, Liang SJ, et al. Ultrasound-guided pigtail catheters for drainage of various pleural diseases. Am J Emerg Med 2010;28:915-21. [Crossref] [PubMed]
- Hofmann HS, Neu R, Potzger T, et al. Minimally Invasive Vacuum-Assisted Closure Therapy With Instillation (Mini-VAC-Instill) for Pleural Empyema. Surg Innov 2015;22:235-9. [Crossref] [PubMed]
- Sahn SA, Iseman MD. Tuberculous empyema. Semin Respir Infect 1999;14:82-7. [PubMed]
- Malhotra P, Aggarwal AN, Agarwal R, et al. Clinical characteristics and outcomes of empyema thoracis in 117 patients: a comparative analysis of tuberculous vs. non-tuberculous aetiologies. Respir Med 2007;101:423-30. [Crossref] [PubMed]
- Mao C. Effect of pleural thickness of tuberculous empyema on the choice of treatment. Chinese Journal of Rural Medicine and Pharmacy 2012;19:12-3.
- Yuan W. Clinical analysis of the treatment for tuberculous purulent according to pleural thickness. Chinese And Foreign Medical Research 2011;9:33-4.
- Silverman SG, Mueller PR, Saini S, et al. Thoracic empyema: management with image-guided catheter drainage. Radiology 1988;169:5-9. [Crossref] [PubMed]
- Ulmer JL, Choplin RH, Reed JC. Image-guided catheter drainage of the infected pleural space. J Thorac Imaging 1991;6:65-73. [Crossref] [PubMed]
- Westcott JL. Percutaneous catheter drainage of pleural effusion and empyema. AJR Am J Roentgenol 1985;144:1189-93. [Crossref] [PubMed]
- Merriam MA, Cronan JJ, Dorfman GS, et al. Radiographically guided percutaneous catheter drainage of pleural fluid collections. AJR Am J Roentgenol 1988;151:1113-6. [Crossref] [PubMed]
- Roberts HS. BTS guidelines for the management of pleural infection. Thorax 2004;59:178. [Crossref] [PubMed]


