Report of a lung carcinoma extended to the left atrium through pulmonary vein
Introduction
Although relatively rare, the extension of the pulmonary neoplasm to the left atrium (LA) has been well documented, particularly in patients with primary lung cancer (1,2). In a previous review of 215 lung cancer patients studied by gadolinium-enhanced 3D magnetic resonance angiography, an involvement of the proximal portion of the pulmonary veins and an extension into the LA were found in 9 (4.2%) and 2 (0.9%) patients, respectively (3). Similarly, a more recent retrospective analysis of 4,668 patients who underwent surgery for lung cancer found pathological evidence of pulmonary vein and LA involvement in 34 (0.7%) and 25 (0.5%) subjects, respectively (4).
Tumors that directly invade the LA belong to T4 of the TNM classification, suggesting that the tumor is inoperable. However, lately, the indication of surgical resection of lung cancers has been expanded to some T4 patients, and long-term survival has been reported. Primary lung carcinomas can invade the LA through or along the pulmonary veins. The tumor extension through the pulmonary veins is few reported with scarce publications on the specialized literature (3). Therefore, the unusual primary lung carcinoma invasion of LA through pulmonary veins justifies this case report (5,6).
Case presentation
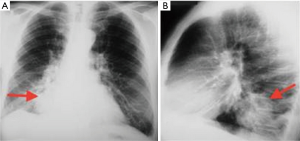
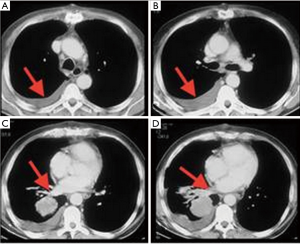
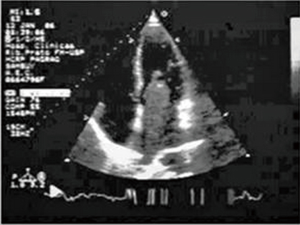
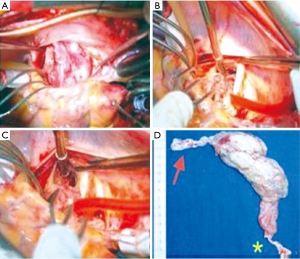
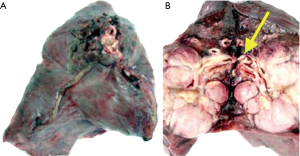
A 62-year-old man, previously healthy, presented with 1-month ventilatory-independent right hemithorax back pain, dry cough and large effort dyspnea. He also referred weight loss of 12 kg in 10 months and denied hemoptysis. As antecedents, he smoked 1–2 packs/year and moderate daily alcoholism. On physical examination, the patient was in good general condition, hydrated and regular respiration at rest [blood pressure (BP) =120/80 mmHg; heart rate (HR) =90 bpm; respiratory rate (RR) =16 rpm], with cardiac auscultation presenting two phonetically normal rhythmic sounds without murmurs. Pulmonary auscultation revealed a slightly diminished vesicular murmur in the lower 1/3 of the right hemithorax without adventitious noises. Chest radiography showed a mass over the right lower lung (Figure 1). A CT scan confirmed the radiography image with the mass extending along the right inferior pulmonary vein and a tumor in the LA (Figure 2). Transthoracic and transesophageal echocardiography revealed large mass within the LA (occupying almost the entire cavity), measuring about 10 cm × 3 cm at its largest diameter, prolapsing into the left ventricle (Figure 3). Bronchoscopy, head CT scan, and whole-body bone scintigraphy, as staging investigation, did not show any distant metastasis. The patient was successfully operated removing the intracardiac and inferior pulmonary vein tumor with the aid of cardiopulmonary bypass (Figure 4), followed by a right inferior lobectomy carried out after 25 days (Figure 5). After 30 days from surgery presented seizures associated a brain metastasis evidenced by CT when adjuvant radio and chemotherapy was started (Figure 6). During the next 90 days the clinical conditions worsening and the patients died 4 months after the surgical treatment.
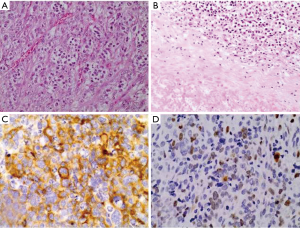
The morphological and immunohistochemically findings confirmed a diagnosis of large cell neuroendocrine carcinoma of the lung. The immunohistochemistry study confirmed the neuroendocrine differentiation of the tumor cells with positivity for chromogranin A, synaptophysin and neuro-specific enolase (NSE). On microscopic examination, the tumor had an organoid pattern composed of nests of large, pleomorphic cells with ovoid nuclei, prominent nucleoli and clear cytoplasm (Figure 6A). There were extensive areas of necrosis (Figure 6B). The immunohistochemistry study revealed positivity of the neoplastic cells for AE1AE3 (focal), 35βH11, CAM5.2 (focal), CEA (focal), chromogranin A (focal), synaptophysin (Figure 6C), NSE, and negativity for LCA, 34βE12, CK7, CK20, TTF-1. The proliferation index (Ki-67) was approximately 40% (Figure 6D).
Discussion
Left atrial tumor direct extension via pulmonary veins is uncommon and the literature search shows more cases involving sarcoma than direct lung extension of bronchogenic carcinoma (7). Guha and colleagues (2011) presenting an important left atrial extension of lung carcinoma simulating myocardial infarction highlighted a worldwide scarcity of reported cases. Very few of such cases have been reported worldwide (8). A left atrial mass as a manifestation of lung carcinoma was reported by researchers in Australia (9) and Memphis (10). Bronchogenic carcinoma mimicking left atrial myxoma was reported from Bombay, India (7). Left atrial invasion by lung carcinoma through a pulmonary vein was visualized by Lestuzzi et al. from Italy (11) by Desai et al. from Pittsburgh (12) and also by Watanabe and Kubo (6).
There were no clear patterns regarding the histological type or tumor location in these cases. On the other hand, all the tumors showed rapid growth and comprised a large mass in the lung parenchyma. Especially the cardiac and intravascular portions of each tumor were less differentiated and more necrotic than the primary focus in the lung. Radical surgery using a cardiopulmonary bypass for lung cancer patients with such intracardiac involvement is useful for improvement of the performance status and reduces the risk of sudden death due to cardiac failure or tumor emboli (13).
According to Ballo and colleagues, the evolution towards cerebral stroke has rarely been reported. They described an atypical case of hematogenous metastatic invasion of the LA from pulmonary neoplasm extension presenting as an ipsilateral stroke (14). In the present case, the intracardiac and the pulmonary masses were similar on the microscopic examination. The tumor showed an organoid pattern and was composed of large cells with ovoid nuclei, dispersed chromatin, and prominent nucleoli. There were extensive necrotic areas, and mitotic figures were frequent. No areas with squamous or glandular differentiation were found, ruling out a combined tumor (large cell neuroendocrine carcinoma and squamous cell carcinoma or large cell neuroendocrine carcinoma and adenocarcinoma). Even though extremely rare, the intracardiac extension of lung large cell neuroendocrine has been previously reported in the literature (15).
As pointed in the introduction of this text, the case report has two primary justifications, even considering the poor outcome: (I) rarity and (II) the possibility of the surgical treatment of a tumor belong to T4 of the TNM classification. It is possible to speculate that cerebral metastases, directly related to poor clinical outcome, predate the cardiac surgery. This consideration is based on the surgical observation that the cardiac mass was removed en bloc without fragmentation.
Finally, two points deserve criticism: (I) the patient received brain CT to check metastasis and brain MRI with contrast is the standard image to check brain metastasis as the initial staging of lung cancer, and (II) even considering the evolution towards cerebral stroke has been rarely reported. In this case report, we describe an atypical case of haematogenous metastatic invasion of the LA from pulmonary neoplasm extension presenting as an ipsilateral stroke whose ASCO classification changed during the clinical management. the option of intraoperative radiotherapy for such a trouble case we did not carry out it because, unfortunately, our hospital does not have technical conditions to do it.
Acknowledgements
This report is partially supported by FAPESP, CNPq and FAEPA.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Stella F, Dell'Amore A, Caroli G, et al. Surgical results and long-term follow-up of T(4)-non-small cell lung cancer invading the left atrium or the intrapericardial base of the pulmonary veins. Interact Cardiovasc Thorac Surg 2012;14:415-9. [Crossref] [PubMed]
- Chuah KL, Yap WM, Loh HL, et al. Intravenous extension of sarcomatoid carcinoma of the lung to the left atrium. Pathology 2006;38:359-61. [Crossref] [PubMed]
- Takahashi K, Furuse M, Hanaoka H, et al. Pulmonary vein and left atrial invasion by lung cancer: assessment by breath-hold gadolinium-enhanced three-dimensional MR angiography. J Comput Assist Tomogr 2000;24:557-61. [Crossref] [PubMed]
- Riquet M, Grand B, Arame A, et al. Lung cancer invading the pericardium: quantum of lymph nodes. Ann Thorac Surg 2010;90:1773-7. [Crossref] [PubMed]
- Gates GF, Aronsky A, Ozgur H. Intracardiac extension of lung cancer demonstrated on PET scanning. Clin Nucl Med 2006;31:68-70. [Crossref] [PubMed]
- Watanabe N, Kubo K. Images in cardiology: Intra-left atrial invasive mass extended via the pulmonary vein. Heart 2001;85:271. [Crossref] [PubMed]
- Mehan VK, Deshpande J, Dalvi BV, et al. Direct extension of bronchogenic carcinoma through pulmonary veins into the left atrium mimicking left atrial myxoma. Chest 1992;101:1722-3. [Crossref] [PubMed]
- Guha P, Sardar P, Mookerjee S, et al. Left atrial extension of lung carcinoma simulating myocardial infarction, unusual presentation: case report and literature review. Tanaffos 2011;10:69-71. [PubMed]
- Kadappu KK, Rajaratnam R, Kachwalla H, et al. Lung cancer mimicking left atrial mass. Postgrad Med J 2008;84:386-7. [Crossref] [PubMed]
- Campos P, D'Cruz IA, Dweik HW, et al. Posterior mediastinal spread of bronchogenic carcinoma simulating a mass within the left atrium. Echocardiography 2004;21:341-3. [Crossref] [PubMed]
- Lestuzzi C, Viel E, Mimo R, et al. Left atrial invasion by lung carcinoma through a pulmonary vein. Int J Cardiovasc Imaging 2001;17:107-10. [Crossref] [PubMed]
- Desai MY, Mankad S. Extension of bronchogenic carcinoma through pulmonary vein into the left atrium detected by echocardiography. Echocardiography 2004;21:189-91. [Crossref] [PubMed]
- Kodama K, Doi O, Tatsuta M. Unusual extension of lung cancer into the left atrium via the pulmonary vein. Int Surg 1990;75:22-6. [PubMed]
- Ballo P, Laureano R, Briganti M, et al. Left Atrial Mass Invasion from Pulmonary Neoplasm Extension via the Right Upper Pulmonary Vein Presenting as Ipsilateral Stroke. Case Rep Med 2016;2016:7084234. [Crossref] [PubMed]
- Costache VS, Lantuejoul S, Stoica S, et al. Giant intracardiac neoplasic thrombus of a large cell neuroendocrine carcinoma of the lung. Cardiovasc Pathol 2010;19:e85-7. [Crossref] [PubMed]


