Approach to resection of sternoclavicular tumor abutting the common carotid artery in irradiated field
Introduction
Surgical approach of head and neck squamous cell carcinoma (HNSCC) metastases to the base of the neck including the sternoclavicular junction (SCJ) poses a challenge. Post-operative and post-radiation effects related to primary tumor treatment, and the close association with neurovascular structures at the SCJ increases the difficulty for a safe surgical resection. In order to ensure a safe approach, careful multi-disciplinary planning and adequate exposure of the surgical field and related vascular structures are necessary. Numerous approaches have been described for the management of lesions located in the apical thoracic region and mediastinum (1,2); however, a specific approach for tumors located in the SCJ in a hostile field is not well defined. We herein present a patient with a history of tracheostomy and neck radiation who presented with a HNSCC metastasis located at the SCJ. We describe our preoperative planning for vascular control and possible reconstruction as well as our surgical approach utilizing a bottom-to-top median sternotomy to the level of angle of Louis with an en bloc resection of manubrium, clavicles, and first ribs.
Case presentation
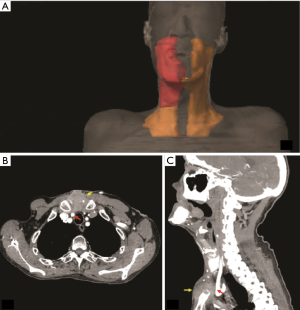
A 61-year-old male with a right clavicular mass was referred to our clinic. His past medical history was significant for heavy tobacco and alcohol use, and human papillomavirus (HPV) positive squamous cell carcinoma of the right tonsil (stage IVA, T4aN2bM0) treated with right pharyngectomy, cranial base resection, tracheostomy, and neck dissection with radial forearm free flap reconstruction. Subsequently, he received adjuvant chemo-radiotherapy (cisplatin and 60 gray of intensity-modulated radiation therapy) (Figure 1A). Eleven months later he presented with an enlarging right clavicular/suprasternal mass which proved to be metastatic HNSCC. On positron emission tomography (PET) scan, no other sites were suspicious for metastasis. We obtained a neck CT angiogram to better delineate the vascular anatomy, and this demonstrated a lobulated 5.6 cm mass located at the SCJ with sternal invasion and abutment to the right common carotid artery (Figure 1B,C, Figure 2). The case was discussed at the multi-disciplinary Head and Neck Cancer Tumor Board, and the consensus was to proceed with surgical resection followed by adjuvant chemotherapy and boost radiation therapy.
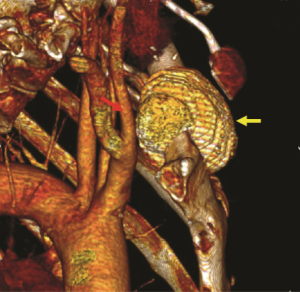
Given the history of radiation and tracheostomy, and the abutment of the tumor to the right common carotid artery, our greatest concern was the dissection of tumor off the vessel or potential en bloc resection with the vessel. As such, vascular surgery was involved. Because of the irradiated field and the potential of contamination from a possible airway injury, the plan was to avoid prosthetic vessel reconstruction. In preparation, we obtained vein mapping to ensure the great saphenous veins were of adequate caliber for vascular reconstruction. To ensure safe proximal access to the base of the innominate artery, we planned to approach the tumor from the inferior aspect with a sternotomy. Given the expected extent of the resection and the anticipated sternotomy, plastic surgery was involved. We planned for a rotational pectoralis major flap to cover the sternotomy.
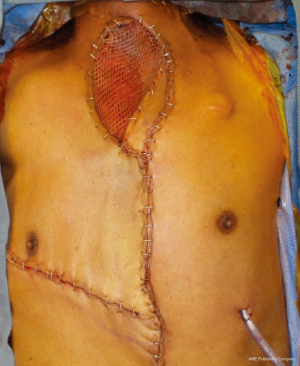
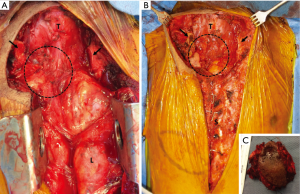
In the operating room, we prepped the groins and had fluoroscopy available such that we could place an endovascular balloon to occlude the innominate artery as a backup approach to obtain proximal control. An incision was made above the old tracheostomy site to excise the old scar. This was then carried down the midline to the xiphoid. Sternotomy was performed from the inferior aspect in combination with blunt finger dissection of the posterior sternum to ensure the sternum was free. The sternal plate was sawed up to the level of the angle of Louis, above which the sternum was adherent to the underlying structures. After this, the sternum was sawed transversely from the angle of Louis to the interspace below the 1st ribs. We then dissected and divided the medial portions of the first ribs and the left clavicle. This allowed us to mobilize the tumor cephalad and work on the dissection posterior to the sternum/mass. Despite the hostile field, the excellent exposure and access to proximal vasculature allowed us to dissect the tumor away from the innominate artery and the right common carotid artery safely. Subsequently, dissection plane around the right clavicle was achieved while maintaining good visualization of the right subclavian vein, and the medial edge of the right clavicle was divided. Finally, the remaining tumor adhered to the anterior wall of the trachea was dissected (Figure 3). We did make a pinhole defect in the anterior trachea which was primarily repaired. Frozen section on this tracheal margin was positive. Chest wall reconstruction was then completed using bilateral pectoralis major muscle myocutaneous flaps with a skin graft and vacuum-assisted wound closure (VAC) dressing (Figure 4). The patient had an excellent recovery without any perioperative complications and was discharged on post-operative day 6. All margins were negative except the tracheal margin, for which he received boost radiation therapy in addition to palliative immunotherapy with nivolumab. After 9 months, the patient is doing well without complications. With physical therapy, he has minimal range of motion deficits in his upper extremities.
Comments
HNSCC metastasis to locations such as the apical thoracic region and the SCJ are rare, and their resection can be challenging. Numerous surgical approaches have been described for resection of lesions located in the sternum, the base of the neck and apical thoracic region, as well as for the treatment of SCJ infections (2-4). In these approaches, a combination of different sternal and clavicular resections is described. Moreover, a complete resection of the SCJ has been described in some cases, with subsequent reconstruction of the chest wall defect with muscle flaps or sternal prosthesis (2-4).
Our case presented a challenge of hostile field from previous radiation and tracheostomy as well as the abutment to the common carotid artery, necessitating adequate exposure of the surgical field and access to proximal blood vessels. Approaching this tumor from the clavicle toward the sternum would not have provided optimal exposure or proximal control in the event of vascular complication. Our surgical approach was performed as described to obtain access and proximal vascular control in the case of carotid artery injury. This approach gave us a clear view of the tumor and its relation to the vascular structures, allowing us to achieve safe resection. In addition, we were prepared for endovascular control of the innominate artery as well as vascular reconstruction with saphenous vein. A multidisciplinary approach including thoracic, vascular, head and neck, and plastic surgeons is recommended to plan a safe approach and to optimize surgical field exposure, as well as the chest wall reconstruction.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- de Perrot M, Rampersaud R. Surgical approaches to apical thoracic malignancies. J Thorac Cardiovasc Surg 2012;144:72-80. [Crossref] [PubMed]
- Vanakesa T, Goldstraw P. Antero-superior approaches in the practice of thoracic surgery. Eur J Cardiothorac Surg 1999;15:774-80. [Crossref] [PubMed]
- Chen C, Huang X, Chen M, et al. Surgical management of a giant sternal chondromyxoid fibroma: a case report. J Cardiothorac Surg 2015;10:178. [Crossref] [PubMed]
- Puri V, Meyers BF, Kreisel D, et al. Sternoclavicular Joint Infection: A Comparison of Two Surgical Approaches. Ann Thorac Surg 2011;91:257-61. [Crossref] [PubMed]