Long-term quality of life after endovac-therapy in anastomotic leakages after esophagectomy
Introduction
Anastomotic leakages after esophagectomy remain to be a major complication leading to a prolonged ICU and hospital stay with high risk of mortality (1,2). Standard treatment options are endoscopic stent insertion, endoscopic transluminal drainage or surgical revision. In the last years, endoscopic endoluminal vacuum therapy (EVT) has been introduced and successfully used as a new treatment option (3,4). Several studies showed that the inflammatory septic response can be controlled and stabilized by drainage of the mediastinal leakage cavity and a healing of the wound cavity can be achieved (5-11). Different studies reported good results in short term survival of 80–96% (4,6-10,12-15). In our department EVT was successfully established with a significantly lower hospital mortality of septic patients compared to stent therapy and surgical revision (6).
Up to date a study that measures health related quality of life (HRQOL) is missing and of major interest as HRQOL is one of the most valuable goals in a successful long-term patient care. To classify HRQOL we compared HRQOL after EVT with HRQOL of patients without anastomotic leakages. Special interest was given to the influence of the site of the anastomosis, treatment specifics, length of ICU and hospital stay, anastomotic strictures, tumor stage, sepsis and neoadjuvant and adjuvant treatment on HRQOL after EVT.
Methods
Study cohort
To exclude a sampling bias, the leakage rate and incidence of anastomotic strictures were analyzed in all esophagus cancer patients treated with an esophagectomy between 2008 and 2014. The results of EVT-treated patients were compared to patients without leakages. A leakage was defined as any insufficiency of the gastroesophageal anastomosis or suture of the gastric conduit and included an ischemia of the upper end of the gastric conduit adjacent to the anastomosis. The definition of a leakage ranged from a small fistula to a complete disrupture of the esophagogastrostomy. All leakages were detected endoscopically.
Study design
A self-administered European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-C30 (EORTC QLQ-C30) with an additional upper gastrointestinal tract questionnaire was given to 73 selected patients for a prospective analysis. Informed consent was obtained from all patients and the study was approved by the local ethics committee (AZ: D421/13). A professional psycho-oncological support was offered to all patients. Assessment was carried out prior to surgery, after discharge, 6 months and 12 months after surgery. The questionnaire contained 30 main questions related to various diseases. The questionnaire has five function scales (physical functioning, role functioning, cognitive functioning, emotional functioning, social functioning) and three symptom scales (fatigue, pain, nausea/vomiting). Moreover, the questionnaire included a global health-scale, quality of life-scale and additional parameters commonly used to assess typical clinical symptoms and status of cancer patients (dyspnea, appetite loss, insomnia, constipation, diarrhea, financial difficulties). For easier interpretation, the assessed scores were transformed to a scale ranging from 0 to 100. High levels of global health, HRQOL and function scales indicated a higher ability. High scores of symptom-scales indicated suffering of the patient (16).
HRQOL was prospectively analyzed for all patients. In a second step HRQOL was tested between leakage patients and patients without leakages. Factors that might have an influence on HRQOL after EVT were analyzed in a third step. Age (<67 vs. ≥67 years), sex, site of the anastomosis (abdominal vs. thoracic vs. cervical anastomosis), length of EVT (<14 vs. ≥14 days), length of ICU (no ICU stay vs. <14 vs. ≥14 days) and hospital stay (<30 vs. ≥30 days), anastomotic strictures, tumor stage and entity, type of neoadjuvant and adjuvant treatment, tumor recurrence, type of thoracic approach (thoracoscopy vs. thoracotomy) and sepsis were entered in the correlation analysis. A cut-off of 67 years was chosen as this age represents the age of retirement in Germany. The cut-off of 30 days’ patient hospitalization or 14 days EVT-treatment and ICU-stay were chosen as most patients, who were treated or stayed beyond the cut off values suffered severe complications. As a control group, we used the prospectively assessed HRQOL-data of patients without leakages. These patients underwent surgery during the same time period the EVT-group received surgical treatment. There were no exclusion criteria.
Esophagectomy was done by abdomino-thoracic approach (Ivor-Lewis approach) (n=53) with thoracic anastomosis, three-field approach (McKeown approach) (n=16) with cervical anastomosis or abdominal-transhiatal approach without thoracotomy (n=4) with abdominal anastomosis. The decision of the site of the anastomosis depended on the tumor resection margin. Passage was re-established by a gastric conduit. Anastomotic leakages were detected by endoscopy. The resection specimen was reviewed by the hospital’s pathologist. In patients with anastomotic leakages an Endo-Sponge® or Eso-Sponge® system (B. Braun, Melsungen, Germany) was used as previously published (4-6).
Statistical analysis
Metric parameters were expressed as total numbers (%), median or mean value ± standard deviation. Comparison of function- and symptom scores at different assessment time points of all patients and between the treatment groups were tested with a paired t-test. Influence of demographic and clinical parameters on HRQOL-functioning and symptom scores under EVT-treatment were tested by using a one-way ANOVA. All distribution and frequencies of medical data were compared by Pearson-Chi-Quadrat test. A P value <0.05 was considered statistically significant. All analyses were conducted using the Statistical Package for Social Sciences software (version 22.0, SPSS Inc., Chicago, IL, USA).
Results
Patient and treatment characteristics
Between 2008 and 2014, a total of 187 esophagus cancer patients were treated by an esophagectomy at the UKSH, Campus Kiel. The leakage rate was 33%. Patients with a leakage were treated in 78% by EVT, 8% by stent insertion and 14% by surgical revision. Anastomotic strictures were found in 9%. Strictures were found significantly more often in patients treated with EVT (20%) (P=0.006). Due to a small number of patients, patients with stent-treatment and surgical revision were not included in the HRQOL analysis.
Seventy-three patients agreed to participate in the prospective HRQOL-assessment. Of these 73 patients, 23 were treated by EVT and 50 had no leakage. Patients were followed up for a median of 1.6 years (0–6 years). In the study cohort, the mean age of the patients was comparable between the groups. There were more men in both groups. Patient’s sex was not significantly different between the groups. An adenocarcinoma was diagnosed in 79.5%, a squamous cell carcinoma in 20.5%. There was no difference in the incidence of the different tumor entities. Looking at the tumor stage most patients had T3-tumours followed by T0, T1 and T2-tumours. There was a significant higher incidence of T0-tumours in the no leakage-group compared to the EVT-group. A positive lymph node status was diagnosed more often in both groups. There was no significant difference in the incidence of positive lymph nodes or tumor recurrence between groups. A tumor positive resection margin was diagnosed more often in the EVT-group. None of the patients had an extra-esophageal tumor spread at the time of resection. Neoadjuvant chemotherapy was the most favored neoadjuvant treatment concept 49%. Most patients had no adjuvant treatment 66%. There was no significant difference in the type of the performed neoadjuvant and adjuvant treatment concept between the groups. The most favored site of the anastomosis was intra-thoracic in 73%. Minimal invasive thoracoscopic surgery was used significantly more often in the EVT-group. The surgical approach and site of the anastomosis was not significantly different between the groups. A hospitalization ≥30 days, an ICU-stay ≥14 days, incidence of sepsis and an anastomotic stricture were observed significantly more often in the EVT-group. Length of EVT was 25±17 days. There were no EVT-related complications. Because of the good clinical status an insertion of an endoscopic stent was done in 9% (n=2) patients with the aim to accelerate the healing process. In 9% (n=2) an additional surgical revision was needed to clean the pleural cavity via minimal invasive thoracoscopic approach in an ongoing septic condition of the patients on the ICU. Both patients survived and a complete healing of the leakage cavity was achieved by EVT. Over all the complete healing of the wound cavity was reached in 91%. All P values, patient and treatment characteristics are shown in Table 1.

Full table
HRQOL-characteristics
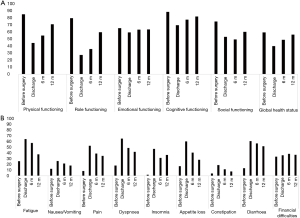
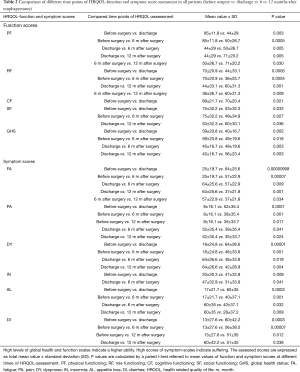
Response rates of all HRQOL-assessed patients were 30% before surgery [EVT-group: 39% (n=9), no leakage-group: 26% (n=13)], 51% at discharge [EVT-group: 43% (n=10), no leakage-group: 54% (n=27)], 78% at 6 months [EVT-group: 78% (n=18), no leakage-group: 78% (n=39)] and 65% at 12 months after esophagectomy [EVT-group: 65% (n=15), no leakage-group: 64% (n=32)]. In a first step HRQOL of all patients was prospectively analyzed. After surgery, all patients had a significant reduction in all function scales except emotional functioning, which was unaffected throughout the entire time of assessment. For symptom scores, patients complained about more fatigue, pain, dyspnea, insomnia, appetite loss and diarrhea at time of discharge. Except for the symptoms diarrhea and pain, all symptom-scores and all function-scores recovered over time, but did not reach levels reported prior to surgery. Twelve months after surgery patients still complained about significantly worse diarrhea and pain (Figure 1). Significant values of HRQOL of all patients are shown in Table 2.
Full table
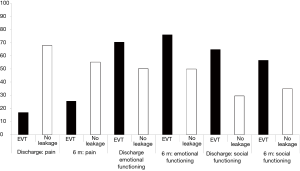
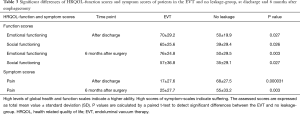
In a second step, a possible difference between EVT-treated patients and patients without leakages were analyzed. This comparison showed a significantly better emotional functioning and social functioning in the EVT-treated patients. Furthermore, after EVT patients complained about less pain after discharge and 6 months after surgery (Figure 2). Significant values of HRQOL in differences between EVT-treated patients and patients without leakages are shown in Table 3. Almost all functioning and symptom scores showed a continuous improvement after surgery in both groups, but a comparable HRQOL as measured before surgery was achieved in none of the groups.
Full table
HRQOL after EVT
In the third step factors were analyzed, which might influence HRQOL of EVT-patients. Older patients (≥67 years) complained about significantly worse constipation and appetite loss after discharge and 6 months after surgery. Younger patients complained about more financial difficulties before surgery. Correlation of tumor stage showed significantly worse scores for fatigue in patients with lymph node metastases 12 months after surgery. Patients with a tumor recurrence showed a higher rate of insomnia 6 months after surgery. T-stage, R-status, tumor grading and entity had no effect on HRQOL after EVT. Analysis of EVT therapy characteristics and complications showed significantly worse scores for patients with strictures, after sepsis, a shorter hospital stay, a shorter ICU-stay and shorter therapy duration. These patients reported about lower physical functioning, cognitive-functioning, global health status and more appetite loss 6 and 12 months after surgery. Surprisingly patients with sepsis, a longer hospital, longer ICU-stay and longer duration of EVT reported about better symptom and function scores. A sepsis under EVT predicted significantly less pain at discharge and a better role functioning 12 months after surgery. Patients with a longer ICU-stay had a significant better role functioning 12 months after surgery. A hospital stay ≥30 days was associated with significantly less pain at discharge and 12 months after surgery. Patients with duration of EVT ≥14 days complained about significantly less pain and appetite loss and showed a better physical functioning 12 months after surgery. All significant EVT-related HRQOL-scores are shown in Table 4.
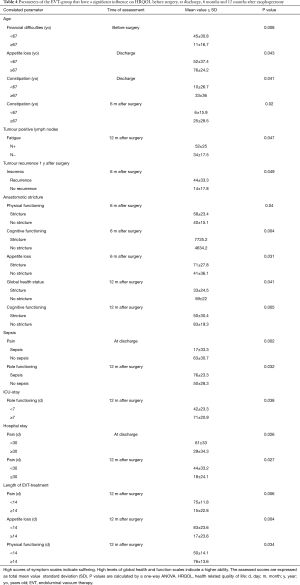
Full table
Discussion
To our knowledge this study presents the first results of HRQOL-assessment of EVT-treated patients in a prospective longitudinal study design up to 12 months after surgery. The leakage rate of 33% in all 187 esophagus resected patients is in the upper range of reported leakage rates, which range from 0.57% up to 53% (12,17,18). Looking at the high range of reported leakages and the missing definition of complications in 63%, as shown in a meta-analysis by Blencowe et al. (19), leads one to assume that a clear definition of complications and leakages in esophageal surgery is needed. Therefore, an international consensus conference recently proposed a standardization for complications associated with esophagectomy (20). The higher rate of leakages in this study might be due to aggressive endoscopic diagnostics in our institution and wide inclusion criteria for leakages. Compared to surgically revised and stent-treated patients, EVT-treatment showed significant better results in successful closure of the cavity and survival, which led to a primary EVT-treatment of patients with anastomotic leakages at our institution (6). Only few patients in an ongoing septic condition under EVT-treatment needed an additional surgical revision in this study. Results of different studies showed, that EVT resulted in a better healing of the wound cavity compared to stent therapy (21,22). Therefore, a stent-insertion is rarely used as an additional treatment option at our institution. Due to a small number of patients treated by stent-insertion or surgical revision, it was not possible to compare all leakage treatment options in this single-center analysis.
The higher incidence in R1-resection margins in the EVT-group might reflect a technically more complex surgery to resect these tumors and might also lead to a higher risk of an anastomotic leakage. Though, there is still disagreement if an advanced tumor stage leads to a higher risk of leakages. Cooke et al. described a significant correlation of an advanced tumor stage with the incidence of leakages, while Viklund et al. did not confirm these results (18,23). Further studies are needed to confirm these results.
It is known that HRQOL drops after surgery and recovers within 1 year after surgery. Nevertheless, patients still suffer from impaired HRQOL in the long-term follow up (24-26). This initial impairment of HRQOL with a following recovery was also measured in this study. The significantly worse complains for diarrhea and pain can be explained by the type of surgery and treatment after surgery. Most patients had a more invasive thoracotomy, which is known to be associated with more pain and was significantly more often used in the no leakage-group. The effect of a better HRQOL due to a minimal invasive thoracoscopy was recently reported and showed lower incidents of pneumonia and minor pain (24,27). The worse complains of diarrhea in the long-term follow up could be explained by a different diet and an adjuvant oncological treatment. Several authors reported about an impaired HRQOL in patients with complications after esophagectomy (24,28,29). This was not confirmed by the data of this study. Surprisingly, patients suffering anastomotic leakages showed a better HRQOL and comparable scores to patients without leakages were measured 1 year after surgery. These findings are explainable by a good tolerance of EVT in the long-term follow up and a so-called shift response (26,29,30). After the definition of the world health organization HRQOL is the individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals. In this study patients with anastomotic leakages and a complicated longer hospital-stay are happy having survived this complication and seem to value their HRQOL in the first 6 months after surgery less serious, which led to these unexpected results of a better HRQOL compared to patients with an uncomplicated postoperative course.
In this study, young patients reported about financial difficulties, even before surgery. This can be explained with a better financial background and a better support of older patients by their families. Comparable data were published by our research group in patients, who had received a liver transplantation (31). Symptoms that correlated with a higher age were constipation and appetite loss, which are known to be occurring more often in older patients (32,33).
An advanced tumor stage reflected by tumor positive lymph nodes and an early tumor recurrence was associated with more insomnia and fatigue and is consistent with the literature (24,34). Anastomotic strictures are a known long-term complication (26,35,36). In this study, anastomotic strictures occurred significantly more often after EVT and were associated with an impaired HRQOL. These patients didn’t reach HRQOL-scores of patients without a stricture even after endoscopic dilation of the stricture. A reason for the higher incidence of strictures after EVT is mostly due to the inflammatory response in the leakage cavity and following enhanced cicatrization (37,38). Here it is not clear if the higher incidence of strictures is directly related to the EVT or, if the strictures are only related to inflammatory response in the leakage cavity and following enhanced cicatrization. To clarify this, a retrospective analysis comparing different leakage treatment options is needed. A prospective study design would be critical from the ethical point of view as EVT, compared to alternative treatment options, leads to significant better survival rates. A second reason in this study could be that 5 of these 6 patients had a recurrence of the tumor within the first year after surgery and appetite loss and eating disorders might have led to an impaired HRQOL.
The present study’s limitation is mainly related to the sample size and the study design as the patient’s treatment was not possible to be randomized. The sample size of EVT-treated patients was small due to this innovative treatment option, which was used for 6 years at the time of the data assessment. Otherwise, a sampling bias was ruled out as the rate of EVT to no-leakage patients was in proportion to the rate of EVT to no-leakage patients in all patients treated by esophagectomy. A randomized trial was not possible because due to significant better survival rates under EVT compared to other leakage treatment options. Therefore, a prospective randomized multicenter study comparing HRQOL of the different treatment options would be favorable but also hard to perform concerning the ethical point of view. A further weak aspect of the study is the low number of patients treated by EVT. This is due to the fact that EVT for leakages after esophagectomy is a quiet young treatment option with good survival rates, which has not been performed for a long time. Maybe in the near future, a study with a larger number of patients can be done. A selection bias cannot be ruled out. Some patients might have overestimated or underestimated their activities or may have misinterpreted the questions. Patients who were too weak to respond to the questionnaire were not included. This is reflected by the gap of participating patients between discharge and 6 and 12 months after surgery, as patients might have been too weak to fill out the questionnaire after surgery and a longer hospital stay. The low response rate before surgery might be due to mental stress by the upcoming operation. Furthermore, patients with EVT were longer in the hospital and had a longer contact to the doctors during EVT, which might has influenced them in judging their individual HRQOL in answering the questionnaires. Nevertheless, due to a longitudinal study design, we were able to investigate changes in HRQOL within individuals over time.
In conclusion EVT showed a comparable outcome in HRQOL in the long-term follow up compared to patients without leakages. One factor that predominantly had an influence on HRQOL after EVT was an anastomotic stricture. In future studies the question whether an advanced tumor-stage before surgery is associated with a higher risk of anastomotic leakages or anastomotic strictures after EVT should be investigated. A multicenter study with a greater number of patients is needed to confirm the study’s results and compare these results to other leakage treatment options.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors N Heits, C Schafmayer, J Hampe, B Schniewind and JH Egberts received financial support by B. Braun (Melsungen, Germany) for talks referred to Eso-Sponge® system therapy and visits of esophagus disease related conferences. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. Informed consent was obtained from all patients and the study was approved by the local ethics committee (AZ: D421/13). A professional psycho-oncological support was offered for all patients.
References
- Markar SR, Karthikesalingam A, Vyas S, et al. Hand-sewn versus stapled oesophago-gastric anastomosis: systematic review and meta-analysis. J Gastrointest Surg 2011;15:876-84. [Crossref] [PubMed]
- Saluja SS, Ray S, Pal S, et al. Randomized trial comparing side-to-side stapled and hand-sewn esophagogastric anastomosis in neck. J Gastrointest Surg 2012;16:1287-95. [Crossref] [PubMed]
- D'Cunha J, Rueth NM, Groth SS, et al. Esophageal stents for anastomotic leaks and perforations. J Thorac Cardiovasc Surg 2011;142:39-46.e1. [Crossref] [PubMed]
- Ahrens M, Schulte T, Egberts J, et al. Drainage of esophageal leakage using endoscopic vacuum therapy: a prospective pilot study. Endoscopy 2010;42:693-8. [Crossref] [PubMed]
- Heits N, Stapel L, Reichert B, et al. Endoscopic endoluminal vacuum therapy in esophageal perforation. Ann Thorac Surg 2014;97:1029-35. [Crossref] [PubMed]
- Schniewind B, Schafmayer C, Voehrs G, et al. Endoscopic endoluminal vacuum therapy is superior to other regimens in managing anastomotic leakage after esophagectomy: a comparative retrospective study. Surg Endosc 2013;27:3883-90. [Crossref] [PubMed]
- Wedemeyer J, Brangewitz M, Kubicka S, et al. Management of major postsurgical gastroesophageal intrathoracic leaks with an endoscopic vacuum-assisted closure system. Gastrointest Endosc 2010;71:382-6. [Crossref] [PubMed]
- Hwang JJ, Jeong YS, Park YS, et al. Comparison of Endoscopic Vacuum Therapy and Endoscopic Stent Implantation With Self-Expandable Metal Stent in Treating Postsurgical Gastroesophageal Leakage. Medicine (Baltimore) 2016;95:e3416. [Crossref] [PubMed]
- Scott RB, Ritter LA, Shada AL, et al. Endoluminal Vacuum Therapy for Ivor Lewis Anastomotic Leaks: A Pilot Study in a Swine Model. Clin Transl Sci 2017;10:35-41. [Crossref] [PubMed]
- Smallwood NR, Fleshman JW, Leeds SG, et al. The use of endoluminal vacuum (E-Vac) therapy in the management of upper gastrointestinal leaks and perforations. Surg Endosc 2016;30:2473-80. [Crossref] [PubMed]
- Schorsch T, Müller C, Loske G. Pancreatico-gastric anastomotic insufficiency successfully treated with endoscopic vacuum therapy. Endoscopy 2013;45 Suppl 2 UCTN:E141-2.
- Weidenhagen R, Hartl WH, Gruetzner KU, et al. Anastomotic leakage after esophageal resection: new treatment options by endoluminal vacuum therapy. Ann Thorac Surg 2010;90:1674-81. [Crossref] [PubMed]
- Laukoetter MG, Mennigen R, Neumann PA, et al. Successful closure of defects in the upper gastrointestinal tract by endoscopic vacuum therapy (EVT): a prospective cohort study. Surg Endosc 2017;31:2687-96. [Crossref] [PubMed]
- Ooi G, Burton P, Packiyanathan A, et al. Indications and efficacy of endoscopic vacuum-assisted closure therapy for upper gastrointestinal perforations. ANZ J Surg 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Schorsch T, Müller C, Loske G. Endoscopic vacuum therapy of anastomotic leakage and iatrogenic perforation in the esophagus. Surg Endosc 2013;27:2040-5. [Crossref] [PubMed]
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-76. [Crossref] [PubMed]
- Aminian A, Panahi N, Mirsharifi R, et al. Predictors and outcome of cervical anastomotic leakage after esophageal cancer surgery. J Cancer Res Ther 2011;7:448-53. [Crossref] [PubMed]
- Cooke DT, Lin GC, Lau CL, et al. Analysis of cervical esophagogastric anastomotic leaks after transhiatal esophagectomy: risk factors, presentation, and detection. Ann Thorac Surg 2009;88:177-84; discussion 184-5. [Crossref] [PubMed]
- Blencowe NS, Strong S, McNair AG, et al. Reporting of short-term clinical outcomes after esophagectomy: a systematic review. Ann Surg 2012;255:658-66. [Crossref] [PubMed]
- Low DE, Alderson D, Cecconello I, et al. International Consensus on Standardization of Data Collection for Complications Associated With Esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg 2015;262:286-94. [Crossref] [PubMed]
- Brangewitz M, Voigtlander T, Helfritz FA, et al. Endoscopic closure of esophageal intrathoracic leaks: stent versus endoscopic vacuum-assisted closure, a retrospective analysis. Endoscopy 2013;45:433-8. [Crossref] [PubMed]
- Mennigen R, Harting C, Lindner K, et al. Comparison of Endoscopic Vacuum Therapy Versus Stent for Anastomotic Leak After Esophagectomy. J Gastrointest Surg 2015;19:1229-35. [Crossref] [PubMed]
- Viklund P, Lindblad M, Lu M, et al. Risk factors for complications after esophageal cancer resection: a prospective population-based study in Sweden. Ann Surg 2006;243:204-11. [Crossref] [PubMed]
- Akkerman RD, Haverkamp L, van Rossum PS, et al. Long-term quality of life after oesophagectomy with gastric conduit interposition for cancer. Eur J Cancer 2015;51:1538-45. [Crossref] [PubMed]
- Fuchs H, Holscher AH, Leers J, et al. Long-term quality of life after surgery for adenocarcinoma of the esophagogastric junction: extended gastrectomy or transthoracic esophagectomy? Gastric Cancer 2016;19:312-7. [Crossref] [PubMed]
- Egberts JH, Schniewind B, Bestmann B, et al. Impact of the site of anastomosis after oncologic esophagectomy on quality of life--a prospective, longitudinal outcome study. Ann Surg Oncol 2008;15:566-75. [Crossref] [PubMed]
- Maas KW, Cuesta MA, van Berge Henegouwen MI, et al. Quality of Life and Late Complications After Minimally Invasive Compared to Open Esophagectomy: Results of a Randomized Trial. World J Surg 2015;39:1986-93. [Crossref] [PubMed]
- Scarpa M, Saadeh LM, Fasolo A, et al. Health-related quality of life in patients with oesophageal cancer: analysis at different steps of the treatment pathway. J Gastrointest Surg 2013;17:421-33. [Crossref] [PubMed]
- Cavallin F, Pinto E, Saadeh LM, et al. Health related quality of life after oesophagectomy: elderly patients refer similar eating and swallowing difficulties than younger patients. BMC Cancer 2015;15:640. [Crossref] [PubMed]
- Deschamps C, Nichols FC 3rd, Cassivi SD, et al. Long-term function and quality of life after esophageal resection for cancer and Barrett's. Surg Clin North Am 2005;85:649-56. xi. [Crossref] [PubMed]
- Heits N, Meer G, Bernsmeier A, et al. Mode of allocation and social demographic factors correlate with impaired quality of life after liver transplantation. Health Qual Life Outcomes 2015;13:162. [Crossref] [PubMed]
- Chang L, Toner BB, Fukudo S, et al. Gender, age, society, culture, and the patient's perspective in the functional gastrointestinal disorders. Gastroenterology 2006;130:1435-46. [Crossref] [PubMed]
- Sato Y, Fukudo S. Gastrointestinal symptoms and disorders in patients with eating disorders. Clin J Gastroenterol 2015;8:255-63. [Crossref] [PubMed]
- Zieren HU, Jacobi CA, Zieren J, et al. Quality of life following resection of oesophageal carcinoma. Br J Surg 1996;83:1772-5. [Crossref] [PubMed]
- Urschel JD. Esophagogastrostomy anastomotic leaks complicating esophagectomy: a review. Am J Surg 1995;169:634-40. [Crossref] [PubMed]
- Walther B, Johansson J, Johnsson F, et al. Cervical or thoracic anastomosis after esophageal resection and gastric tube reconstruction: a prospective randomized trial comparing sutured neck anastomosis with stapled intrathoracic anastomosis. Ann Surg 2003;238:803-12; discussion 812-4. [Crossref] [PubMed]
- Rice TW. Anastomotic stricture complicating esophagectomy. Thorac Surg Clin 2006;16:63-73. [Crossref] [PubMed]
- Dresner SM, Lamb PJ, Wayman J, et al. Benign anastomotic stricture following transthoracic subtotal oesophagectomy and stapled oesophago-gastrostomy: risk factors and management. Br J Surg 2000;87:362-73. [Crossref] [PubMed]


