
Transcatheter aortic valve replacement in patients with bicuspid aortic valves
Introduction
First performed in 2002 under compassionate-use conditions (1), the transcatheter aortic valve replacement (TAVR) field for severe symptomatic aortic stenosis (AS) has rapidly evolved with the development of improved transcatheter valve technologies, safer vascular access, and facilitated implantation techniques, all resulting in better clinical outcomes. While initially used only in inoperable patients or those with high surgical risk (2,3), clinical trials demonstrating the equivalence and/or superiority of TAVR compared to surgical aortic valve replacement (SAVR) in intermediate-risk patients (4,5) have expanded clinical use indications (6). Moreover, there are several ongoing clinical trials in low-risk patients which potentially will justify the use of TAVR in AS patients who are younger and are currently treated by SAVR.
Bicuspid aortic valve (BAV) is the most frequently occurring congenital heart defect and has a prevalence of 0.5–2.0% in the overall population (7). BAV can be associated with both AS and aortic regurgitation (AR). In more than 50% of cases, BAV is associated with aortic root and/or ascending aorta dilatation (8). Though most commonly seen in patients who are younger (<60 years) requiring SAVR, the proportion of elderly patients (≥80 years of age) who have a congenitally bicuspid valve may be as high as 20% (9). Historically, due to their younger age, lower surgical risk, and more challenging anatomy, patients with BAV have been treated largely with SAVR, and have been excluded from all large-scale clinical trials comparing TAVR to SAVR. However, recent registry data and observational studies suggest that TAVR may be a feasible option for the treatment of BAV in certain anatomic situations, with the caveats of possibly increased PVR and/or aortic annulus or root injury (10).
Screening and planning
TAVR in BAV remains challenging due to a variety of anatomic and procedural factors. First, the more elliptical, as opposed to circular, nature of the aortic annulus that frequently accompanies BAV, along with the enlarged anatomy of the aortic root and ascending aorta make it more difficult to position and anchor a transcatheter valve. Second, during valve deployment, the valve frame can be asymmetrically or incompletely expanded and apposed due to patterns of asymmetric and excessive calcification of the valve and the aortic valvular complex. This may result in impaired hemodynamic outcomes (either increased transvalvular gradient or PVR) (11). Third, there is an increased risk of damage to the aortic root and ascending aorta during pre-dilatation valvuloplasty, valve deployment, and post-dilatation (11,12). These factors underscore the importance of pre-procedural planning with multi-modality imaging, with an emphasis on pre-procedural computed tomography (CT).
Congenital bicuspid valve morphology is seen well on high-resolution CT and is most commonly described by the Sievers and Schmidtke classification (types 0, 1, and 2) based on the number of raphe present (13) (Figure 1). The increased use of high-resolution CT has allowed a better understanding of bicuspid anatomy in patients undergoing evaluation for valve replacement, particularly when visualization of the aortic valve by standard transthoracic echocardiography is limited. In patients undergoing TAVR evaluation, CT also permits a comparison between bicuspid and tricuspid valves that may have procedural implications. In one study comparing patients with bicuspid (n=200) and tricuspid (n=200) valves, bicuspid valves were surprisingly less elliptical than expected, though with larger annular areas (521 vs. 463 mm2) and more eccentric calcification than tricuspid valves (14,15). Other studies examining CT characteristics of BAV before and after TAVR have shown bicuspid valves to be more elliptical than tricuspid valves with less complete valve expansion during TAVR, but with comparable valve function (16).

Outcomes
SAVR has long been the treatment of choice for patients with BAV and has excellent operative outcomes (17). Although randomized trials have established TAVR as the standard treatment for patients at high and intermediate surgical risk (3,4), these trials have excluded congenital bicuspid AS due to its unique morphological features. Nevertheless, growing experience, accumulated data, and technological advancements have led to the expanded use of TAVR in the BAV patients (18).
The use of TAVR in BAV has been reported in several case studies and has been associated with increased PVR (19), valve malapposition (20), and higher rates of permanent pacemaker (PPM) implantation (15). A recent meta-analysis of 13 observational studies containing data on 758 BAV patients showed a device success rate of 95%, similar to rates seen in the Society of Thoracic Surgery/American College of Cardiology (STS/ACC) Transcatheter Valve Therapy (TVT) registry (10,21) (Table 1). The pooled incidence of moderate and severe PVR was 12.2% (95% CI, 3.2% to 24.7%) which is higher than that reported for tricuspid aortic valves. Early safety events, including all-cause mortality, stroke, life-threatening bleeding, major vascular complications, or valve dysfunction, occurred at equal rates in BAV and tricuspid valves. There was also no difference in the rate of annular rupture between BAV and tricuspid aortic valves. However, there was a higher need for PPM placement in those with BAV (10). Both increased rates of PPM placement and PVR have been associated with increased long-term mortality in the tricuspid aortic valve population after TAVR in some studies (22). The mechanisms underlying increased PVR and PPM rates are thought to be due to the elliptical nature of the annulus, asymmetric cusps, and severe focal calcification seen in BAV patients.
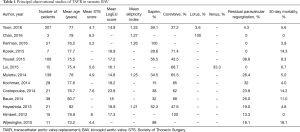
Full table
Technical adjustments during the TAVR procedure are commonly applied to reduce the likelihood of increased rates of PVR, PPM placement, and aortic annulus/root injury. Valve oversizing and overexpansion has been reduced and valve positioning is more cranial, attempting to anchor the prosthesis as much in the heavily calcified leaflets as in the true annulus. These techniques may reduce the need for PPM implantation and aortic root/annulus injury but may also exaggerate incomplete apposition and PVR. Newer generation transcatheter valve types may reduce PVR due to externally applied skirts or cuffs designed to improve apposition without increased trauma to aortic valve structures. In the largest series of TAVR in BAV comparing first-generation valves without external skirts (Sapien and CoreValve) to second-generation valves with external skirts (Sapien 3 and Lotus) there was a decrease in PVR from 8.5% to 0.0% (P=0.002) (23). More data is needed with the newer generation of devices to see if design modifications and newer techniques can improve outcomes after TAVR in BAV patients.
There are no intermediate- or long-term comparative survival data in BAV patients treated with TAVR, as studies have been limited by the young age of BAV patients and less frequent comorbidities compared with the tricuspid AS population. However, a recent study comparing the outcomes of TAVR between the BAV and tricuspid AS populations using propensity-score matching showed patients with BAV had more frequent conversion to surgery compared to those with tricuspid AS [2.0% vs. 0.2%; OR 11.00; 95% CI, (1.42–85.20); P=0.006] and the need for second valve implantation [4.8% vs. 1.5%; OR 3.71; 95% CI, (1.61–8.56); P=0.002], and moderate or severe paravalvular leak [10.4% vs. 6.8%; OR 1.61; 95% CI, (1.04–2.48); P=0.04], leading to lower device success rate [85.3% vs. 91.4%; OR 0.54; 95% CI, (0.37–0.80)] (24). The cumulative all-cause mortality rates at 2-year follow-up were comparable between the bicuspid and tricuspid AS groups (17.2% vs. 19.4%; P=0.28) (24). Given the higher prevalence of bicuspid AS in a younger population, expanding the use of TAVR to this group warrants longer term durability data and possibly a randomized trial versus SAVR alternatives (25).
Conclusions
Although AS due to BAV was previously considered a relative contraindication for TAVR, multiple series have shown TAVR to be feasible, reasonably safe, and efficacious in the BAV population. While higher rates of PVL and need for PPM were seen in first generation devices, advanced techniques and newer-generation devices have been associated with improved device success rates with fewer complications. The ultimate utility and safety of TAVR as an initial treatment strategy for patients with BAV will require larger studies to evaluate the long-term outcomes and durability of TAVR in comparison to surgical alternatives.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation 2002;106:3006-8. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010;363:1597-607. [Crossref] [PubMed]
- Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011;364:2187-98. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2016;374:1609-20. [Crossref] [PubMed]
- Thourani VH, Kodali S, Makkar RR, et al. Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet 2016;387:2218-25. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2017;135:e1159-95. [Crossref] [PubMed]
- Roberts WC. The congenitally bicuspid aortic valve. A study of 85 autopsy cases. Am J Cardiol 1970;26:72-83. [Crossref] [PubMed]
- Verma S, Siu SC. Aortic dilatation in patients with bicuspid aortic valve. N Engl J Med 2014;370:1920-9. [Crossref] [PubMed]
- Roberts WC, Janning KG, Ko JM, et al. Frequency of congenitally bicuspid aortic valves in patients >/=80 years of age undergoing aortic valve replacement for aortic stenosis (with or without aortic regurgitation) and implications for transcatheter aortic valve implantation. Am J Cardiol 2012;109:1632-6. [Crossref] [PubMed]
- Reddy G, Wang Z, Nishimura RA, et al. Transcatheter aortic valve replacement for stenotic bicuspid aortic valves: Systematic review and meta analyses of observational studies. Catheter Cardiovasc Interv 2018;91:975-83. [Crossref] [PubMed]
- Praz F, Windecker S, Huber C, et al. Expanding Indications of Transcatheter Heart Valve Interventions. JACC Cardiovasc Interv 2015;8:1777-96. [Crossref] [PubMed]
- Al-Attar N, Himbert D, Barbier F, et al. Delayed aortic dissection after transcatheter aortic valve implantation. J Heart Valve Dis 2013;22:701-3. [PubMed]
- Sievers HH, Schmidtke C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg 2007;133:1226-33. [Crossref] [PubMed]
- Philip F, Faza NN, Schoenhagen P, et al. Aortic annulus and root characteristics in severe aortic stenosis due to bicuspid aortic valve and tricuspid aortic valves: implications for transcatheter aortic valve therapies. Catheter Cardiovasc Interv 2015;86:E88-98. [Crossref] [PubMed]
- Perlman GY, Blanke P, Webb JG. Transcatheter aortic valve implantation in bicuspid aortic valve stenosis. EuroIntervention 2016;12:Y42-5. [Crossref] [PubMed]
- Kawamori H, Yoon SH, Chakravarty T, et al. Computed tomography characteristics of the aortic valve and the geometry of SAPIEN 3 transcatheter heart valve in patients with bicuspid aortic valve disease. Eur Heart J Cardiovasc Imaging 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Masri A, Kalahasti V, Alkharabsheh S, et al. Characteristics and long-term outcomes of contemporary patients with bicuspid aortic valves. J Thorac Cardiovasc Surg 2016;151:1650-1. [Crossref] [PubMed]
- Yoon SH, Sharma R, Chakravarty T, et al. Transcatheter aortic valve replacement in bicuspid aortic valve stenosis: where do we stand? J Cardiovasc Surg (Torino) 2018;59:381-91. [PubMed]
- Mylotte D, Lefevre T, Sondergaard L, et al. Transcatheter aortic valve replacement in bicuspid aortic valve disease. J Am Coll Cardiol 2014;64:2330-9. [Crossref] [PubMed]
- Yousef A, Simard T, Webb J, et al. Transcatheter aortic valve implantation in patients with bicuspid aortic valve: A patient level multi-center analysis. Int J Cardiol 2015;189:282-8. [Crossref] [PubMed]
- Grover FL, Vemulapalli S, Carroll JD, et al. 2016 Annual Report of The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol 2017;69:1215-30. [Crossref] [PubMed]
- Nazif TM, Dizon JM, Hahn RT, et al. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: the PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc Interv 2015;8:60-9. [Crossref] [PubMed]
- Yoon SH, Lefevre T, Ahn JM, et al. Transcatheter Aortic Valve Replacement With Early- and New-Generation Devices in Bicuspid Aortic Valve Stenosis. J Am Coll Cardiol 2016;68:1195-205. [Crossref] [PubMed]
- Yoon SH, Bleiziffer S, De Backer O, et al. Outcomes in Transcatheter Aortic Valve Replacement for Bicuspid Versus Tricuspid Aortic Valve Stenosis. J Am Coll Cardiol 2017;69:2579-89. [Crossref] [PubMed]
- Yoon SH, Maeno Y, Kawamori H, et al. Diagnosis and Outcomes of Transcatheter Aortic Valve Implantation in Bicuspid Aortic Valve Stenosis. Interv Cardiol 2018;13:62-5. [PubMed]


