
Intercostal nerve blockade for thoracic surgery with liposomal bupivacaine: the devil is in the details
Thoracotomy and minimally invasive video thoracoscopic surgery are the top two causes of short-term and chronic pain resulting from elective surgical procedures (1). Analgesia presents a substantial challenge in day to day practice for thoracic surgeons. Posterior intercostal nerve blocks (PINB) are one of several modalities to address this, and they can be quite effective for pain control. A major limitation has been the duration of action. Lidocaine 1% lasts for 2 hours; with epinephrine the half-life extends to 3 hours. Bupivacaine’s half-life is about 4 hours, potentially as long as 10 hours in some patients. Intercostal absorption is second only to direct intravenous injection. With the introduction of an extended release local anesthetic, liposomal bupivacaine, there has been renewed interest in use of PINB as the pillar of a pain management strategy for thoracic patients, given the 72–96-hour duration of blockade. There have been at least 13 publications in the last 4 years on the use of liposomal bupivacaine for PINB (2-14).
Administration of PINB can be done quickly and easily by the surgeon as part of the operation. This is appealing to avoid the added time and coordination needed for spinal or epidural placement. It is operator dependent and requires attention to important details.
Inject at the very beginning of the surgical case (15)
There is some controversy on the efficacy of pre-emptive analgesia; yet administration of an effective regional block that leads to a neural blockade before incision, with an agent that remains active during the inflammatory phase of nociception (12–48 h) meets the requirements of an adequate preemptive intervention. In our experience, administration of PINB before incision, whether making VATS or thoracotomy incision, is a critical factor in the efficacy of PINB as an analgesic strategy in thoracic surgery.
Administration of the PINB percutaneously, rather than transpleurally
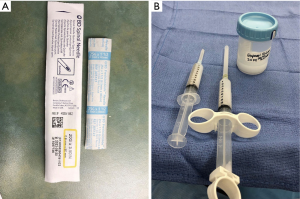
This visibly retains the injectate in the interspace more effectively and at least anecdotally has been much more effective for PINB. The presence of the VATS camera to guide this is immensely helpful (after preemptively blocking the port site and then placing the camera) (Figures 1,2), also see video: https://www.annalsthoracicsurgery.org/cms/10.1016/j.athoracsur.2016.05.050/attachment/b46c50ae-94ba-45a6-8ceb-6a5981fb9419/mmc1.mp4 (14).
Dilute the drug with saline
This provides a larger volume, albeit same dose of active drug, to be injected into each interspace, giving greater opportunity for the drug to interface with the intercostal nerve (Figure 2B). We dilute to a total volume of 40 cc for VATS cases, 80 cc for thoracotomy.
Inject as many interspaces as possible
It is important to inject widely, not just the interspaces which are incised for ports or thoracotomy. This will provide much better relief for chest tube—related pain not only at the chest tube exit site, but also along the parietal pleura which has afferent somatic pain fibers. In addition, inflammatory mediators within the pleural space related to surgery will trigger local pain receptors throughout the parietal pleura; the broader the PINB, the better this process can be mitigated.
In the December 2018 issue of this journal, Dr. Dominguez and colleagues published a retrospective review of 80 patients undergoing intercostal block with either bupivacaine or liposomal bupivacaine for VATS surgery (16). The study was performed at a Kaiser facility in the San Francisco bay area by 3 surgeons over a 2-year period. Patients had either VATS wedge, VATS lobectomy, or minimally invasive esophagectomy. The intervention was compared between two consecutive time periods. Length of stay, pain scores and morphine equivalents in the first 24 hours, and time to ambulation were compared.
The description of the PINB is lacking in detail; however, it does indicate that the block was done at the end of the surgical procedure. It is not stated if this was administered transpleurally or transcutaneously. Only the port incision interspaces, and one above and below were blocked. The authors state that the same dose of bupivacaine with epinephrine was used as was used with liposomal bupivacaine. This would be 266 mg of 0.25% which is 106 mL; it would be a challenge to inject this much volume in just 3 or 4 interspaces. Furthermore this exceeds the maximum safe dose of bupivacaine (not liposomal), 225 mg, which is 90 mL of 0.25% formulation; still a large volume for 3 or 4 interspaces.
There are limitations with the chosen patient population compared, and the endpoints. The inclusion of esophagectomies is problematic due to many confounders of length of stay, and the abdominal incisions are not covered by the unilateral intercostal block. Reported pain scores cannot distinguish the efficacy of the PINB when there are also abdominal port incisions that contribute to pain scores.
Opioid use was reported only up to 24 hours, which does not tell the whole story. The straight bupivacaine is still in effect for up to half of that time period, so it is expected that opioid use would be the same in the two groups. Why compare an intervention at 24 hours when one medication (straight bupivacaine) lasts 7–10 hours, and the other lasts 72–96 hours? It would make more sense to compare pain scores for multiple days to appreciate the difference between the two strategies (3,6,7,12,13). Pain scores are relevant for at least the duration of the hospital stay. Furthermore, the morphine equivalents in the first 24 hours reported for the two groups (29.8 and 31.9 mg), is higher than the total hospital stay morphine equivalents for VATS in our series (22 mg) (13). This suggests that the use of PINB in isolation, without a dedicated enhanced recovery pathway, is not sufficient to achieve good pain control and opioid reduction simultaneously.
In summary, PINB with liposomal bupivacaine, especially in the setting of an enhanced recovery pathway, has been shown to be an effective strategy for postoperative pain management, opioid reduction, reduced length of stay, and reduced complications compared to traditional methods, such as epidural or patient-controlled analgesia (PCA) pumps. The efficacy of this strategy requires attention to specific details, such as timing and technique of injection, dilution with saline, and injection of multiple interspaces (typically interspaces 3–10 when technically possible). The recent publication in this journal (16) reports no benefit to liposomal bupivacaine compared to bupivacaine PINB for VATS surgery because of a lack of attention to these important details, and choice of endpoints. There is plenty of data to support our opinion that liposomal bupivacaine PINB as part of an enhanced recovery pathway is a major improvement to the care of thoracic surgical patients.
Acknowledgements
Funding: For LW Martin: NCI Cancer Center Support Grant 5P30CA044579-27.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Clarke H, Soneji N, Ko DT, et al. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ 2014;348:g1251. [Crossref] [PubMed]
- Mehran RJ, Walsh GL, Zalpour A, et al. Intercostal Nerve Blocks With Liposomal Bupivacaine: Demonstration of Safety, and Potential Benefits. Semin Thorac Cardiovasc Surg 2017;29:531-7. [Crossref] [PubMed]
- Rice DC, Cata JP, Mena GE, et al. Posterior Intercostal Nerve Block With Liposomal Bupivacaine: An Alternative to Thoracic Epidural Analgesia. Ann Thorac Surg 2015;99:1953-60. [Crossref] [PubMed]
- Yin C, Matchett G. Intercostal administration of liposomal bupivacaine as a prognostic nerve block prior to phenol neurolysis for intractable chest wall pain. J Pain Palliat Care Pharmacother 2014;28:33-6. [Crossref] [PubMed]
- Ilfeld BM, Viscusi ER, Hadzic A, et al. Safety and Side Effect Profile of Liposome Bupivacaine (Exparel) in Peripheral Nerve Blocks. Reg Anesth Pain Med 2015;40:572-82. [Crossref] [PubMed]
- Kelley TM Jr, Bailey DW, Sparks P, et al. Intercostal Nerve Blockade with Exparel® Results in Lower Opioid Usage during the First 24 Hours after Video-Assisted Thorascopic Surgery. Am Surg 2018;84:1433-8. [PubMed]
- Parascandola SA, Ibañez J, Keir G, et al. Liposomal bupivacaine versus bupivacaine/epinephrine after video-assisted thoracoscopic wedge resection†. Interact Cardiovasc Thorac Surg 2017;24:925-30. [Crossref] [PubMed]
- Pedoto A, Amar D. Liposomal Bupivacaine for Intercostal Nerve Block: Pricey or Priceless? Semin Thorac Cardiovasc Surg 2017;29:538-9. [Crossref] [PubMed]
- Rincavage M, Hammond L, Reddy S, et al. Pain control using liposomal bupivacaine versus bupivacaine for robotic assisted thoracic surgery. Int J Clin Pharm 2019;41:258-63. [Crossref] [PubMed]
- Saby A, Swaminathan K, Pangarkar S, et al. Alleviating Thoracotomy Pain With Intercostal Liposomal Bupivacaine: A Case Report. PM R 2016;8:1119-22. [Crossref] [PubMed]
- Khalil KG, Boutrous ML, Irani AD, et al. Operative Intercostal Nerve Blocks With Long-Acting Bupivacaine Liposome for Pain Control After Thoracotomy. Ann Thorac Surg 2015;100:2013-8. [Crossref] [PubMed]
- Van Haren RM, Mehran RJ, Mena GE, et al. Enhanced Recovery Decreases Pulmonary and Cardiac Complications After Thoracotomy for Lung Cancer. Ann Thorac Surg 2018;106:272-9. [Crossref] [PubMed]
- Martin LW, Sarosiek BM, Harrison MA, et al. Implementing a Thoracic Enhanced Recovery Program: Lessons Learned in the First Year. Ann Thorac Surg 2018;105:1597-604. [Crossref] [PubMed]
- Mehran RJ, Martin LW, Baker CM, et al. Pain Management in an Enhanced Recovery Pathway After Thoracic Surgical Procedures. Ann Thorac Surg 2016;102:e595-6. [Crossref] [PubMed]
- Kissin I. Preemptive analgesia. Anesthesiology 2000;93:1138-43. [Crossref] [PubMed]
- Dominguez DA, Ely S, Bach C, et al. Impact of intercostal nerve blocks using liposomal versus standard bupivacaine on length of stay in minimally invasive thoracic surgery patients. J Thorac Dis 2018;10:6873-9. [Crossref] [PubMed]



