Performance evaluation of MR-proadrenomedullin and other scoring systems in severe sepsis with pneumonia
Introduction
Sepsis is one of the leading causes of death in critically ill patients. Early and accurate diagnosis and risk evaluation are crucial for management of sepsis (1,2). Adrenomedullin (ADM) is a novel diagnostic instrument, and it may be helpful to manage the sepsis as well as predicting the prognosis in sepsis patients. ADM, a peptide with 52 amino acids, is one of the most potent vasodilating agents, and it has immune modulating activity and some metabolic properties (3,4). ADM also has a bactericidal activity that is further enhanced by modulation of complement activity and regulation. As a consequence of these activities, serum level of ADM increases in sepsis (5,6). The accurate measurement of ADM is a challenging procedure due to its rapid blood clearance. The stable mid-region part of proadrenomedullin (MR-proADM) directly shows level of the fast degraded active peptide of ADM, and it has been detected in plasma of patients (5,7). Because immediate and accurate diagnosis with appropriate risk assessment is vital for optimal care of critically ill patients, many studies, most of the these studies compared the sepsis and healthy control patients, have been worked to evaluate the importance of MR-proADM as a sole diagnostic biomarker in sepsis and septic shock due to pneumonia (8,9).
In present study, we aimed to compare the effect of MR-proADM level, other diagnostic markers, and scoring systems between severe sepsis and CAP patients in terms of severity of disease and mortality rate.
Materials and methods
This observational, single-centre, and prospective randomised study was performed between September 2011 and September 2012. Study was approved by the local ethic committee for human studies, and written informed consent was obtained from all patients. Patients were divided into two groups. Thirty one patients were diagnosed as pneumonia according to their chest X-ray and Turkish Thorax Association Pneumonia Guideline, and they were also diagnosed as severe sepsis or septic shock according to 2001 International Sepsis Definitions Conference Report (10,11). Twenty six patients (control group) were admitted to emergency service due to CAP. Same treatment procedure was performed to all patients in ICU.
The CAP was defined by the presence of one or several newly acquired respiratory signs or symptoms which were included cough, sputum production, dyspnea, core body temperature >38.0 °C, abnormal breath sounds and rales, leukocyte count >10 or <4×109 cells l-1 and an infiltration on chest X-ray (10).
Patients younger than 18, diagnosed with sepsis or septic shock with other reasons, and diagnosed with congestive heart failure were excluded from this study. Patients’ age, sex, additional diseases, and body mass index (BMI) were recorded. Acute Physiology and Chronic Health Evaluation (APACHE) II, Sequential Organ Failure Assessment (SOFA) score, and pneumonia severity index (PSI) were calculated (12-14).
Measurement of serum biomarkers
C-reactive protein (CRP), d-dimer, white blood cell (WBC) counts, and serum procalcitonin (PCT) levels were measured. Blood sample was obtained from peripheral vein for each patient for MR-proADM analysis. The blood was separated into plasma immediately after sampling, and these samples were stored at –80 °C until analyzed. MR-proADM was measured using a new sandwich immunoassay method (MR-proADM; Brahms; Hennigsdorf, Germany).
Definitions
Intra-assay imprecision was under 10% over the entire measuring range, and the functional assay sensitivity [interassay coefficient of variation (CV) <20%] was 0.12 nmol/L. ProADM levels were considered normal when <4 nmol/L based in the median value of proADM observed in healthy adults (2). The time-resolved amplified cryptate emission technology assay was performed (Kryptorn PCT; Brahms, Hennigsdorf, Germany) to analyse serum PCT. Serum CRP concentrations were measured by immunoturbidimetric assay on modular analyser (Roche Diagnostics, Meylan, France).
Statistical analysis
All statistical analysis was performed using SPSS 11.5 (SPSS Inc) for Windows. Descriptive statistic was expressed as mean ± SD or median (min-max), and categorical variables were expressed as case number and percentage. Kolmogorov Smirnov test was carried out to analyze continuous variables. Student’s t-test was performed to analyze the difference of mean in groups and Mann Whitney U test was used to analyze difference of median in groups. Categorical variables were analyzed to use Pearson’s test or Fischer exact test. The effect of PSI, SOFA, and MR-proADR levels on 4- and 8-week mortality rate was analyzed to use multivariate linear regression analysis. Odds ratio and 95% confidence interval were calculated for all variables. Bonferroni correction was performed to control the type 1 error in all multivariate analysis.
Results
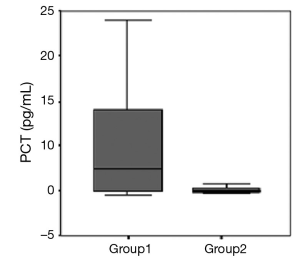
There was no statistically difference between the groups in terms of age, gender, BMI, d-dimer, WBC, and MR-proADM levels (Table 1). The PSI levels, SOFA scores and APACHE II scores were significantly higher in group 1 (P<0.001) (Table 1). Mean CRP levels were significantly higher in group 1 when compared the group 2 (P<0.010). Mean PCT levels were also higher in group 1 than the group 2 (P<0.001) (Figure 1). MR-proADM levels were 5.14 mg/mL in group 1 and 4.83 mg/mL in group 2. There was no significantly difference between the groups in terms of MR-proADM levels (P=0.780). The number of additional disease similar between the groups (P=1.000), whereas the number of patients who had acute respiratory distress syndrome were high in group 1 (P<0.012) (Table 2).
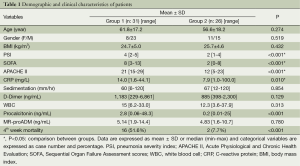
Full table
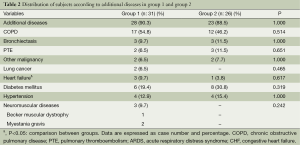
Full table
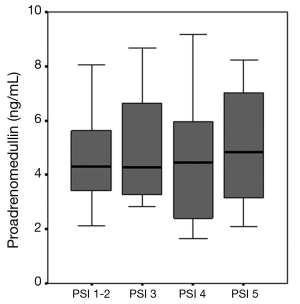
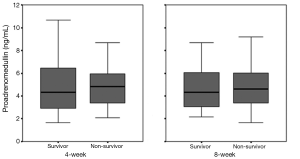
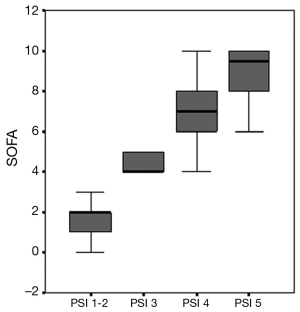
We found correlation between the augmentation of MR-proADM levels and PSI scores, but there was no significantly different (P>0.05) (Figure 2). According to 4- and 8-week mortality rate, MR-proADM levels were higher in non-survivor group, but there was no significant different between the groups (P=0.90) (Figure 3).
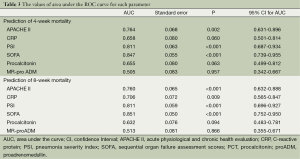
SOFA scores were most significant predictors to determine the 4- and 8-week mortality when parameters evaluated separately in all patients (P<0.001). Each score increment in SOFA caused to 1.618 times (95% CI, 1.246-2.102) increasing the 4-week mortality rate (P<0.001) (Figure 4).
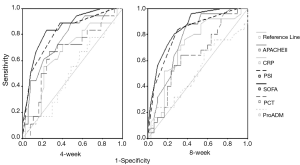
When patients were assessed separately in terms of 4- and 8-week mortality, SOFA score, PSI index, APACHE II scores were found significantly higher in patients who died in 4- and 8-week (P<0.001). Mean inotropic agents use, length of ICU stay, and d-dimer level were also higher in these patients (P<0.001, P<0.031, P<0.006, respectively). The ROC curves of all parameters that we compared for the prediction of 4- and 8-week mortality are shown in Figure 5. The values of area under the ROC curve for each parameter were also shown in Table 3.
Full table
Demographic and clinic characteristics of patients’ survivor and non-survivor groups within are summarized in Table 4. The CRP level was significantly higher in patients who died in 8-week when compared the patients who died 4-week (P<0.020).
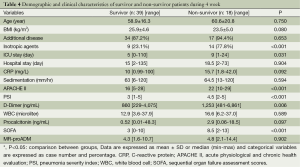
Full table
The MR-proADM was not a significant diagnostic tool to predict 4- and 8-week mortality in all patients (P=0.709, P=0.50, respectively). The PCT and CRP levels were not also valuable for the prediction of 4- and 8-week mortality (P>0.05).
When SOFA, APACHE II scores, and PSI levels compared to MR-proADM individually; all parameters were significantly superior to MR-proADM to predict 4-week mortality (P<0.001, P=0.003, and P<0.001, respectively).
The MR-proADM and SOFA scores combination was found 86.8% specific and 66.7% sensitive to predict 4-week mortality. Additionally, MR-ProADM and PSI combination had 92.1% specificity and 50.1% sensitivity to predict mortality in 4 weeks. When group 1 evaluated for 4-week mortality, MR-proADM and SOFA scores combination provided 78.6% specificity and 75.0% sensitivity, and MR-proADM, SOFA score, and APACHE II combination showed 71.4% specificity and 75% sensitivity.
The MR-proADM was found 90.3% specific and 24.0% sensitive to predict 8-week mortality. MR-proADM and PSI combination showed 71% specificity and 84% sensitivity to expect 8-week mortality. MR-proADM, SOFA scores, and APACHE II combination showed 80.6% specificity and 76.0% sensitivity, and it provided strong for the prediction 8-week mortality. In group 1, 77.8% specificity and 85.7% sensitivity were found when this combination used for the prediction of 8-week mortality.
Discussion
Present study has shown that MR-proADM was not enough to predict severity of disease and 4- and 8-week mortality rate by itself, but MR-proADM had high sensitivity and specifity when combined with SOFA and APACHE II scores. SOFA score was observed a most valuable determiner, when the PSI based evaluation was performed for all phases of the CAP patients.
Many markers and scoring systems have been studied to predict prognosis and mortality in sepsis, septic shock, and pneumonia. Evaluation of prognosis in CAP patients is very challenging procedure and it is required deep assessments. Serum markers are as important as scoring systems to predict severity of disease and mortality rate (8,15). Some serum markers such as PCT and CRP are commonly being used by the researchers (16). Pierrakos and Vincent mentioned that neither PCT nor CRP was not solely enough to determine mortality rate, whereas PCT are superior to CRP in severe septic shock and sepsis patients (17-19). Pierrakos also stated that a single biomarker was not enough to determine prognosis, and combinations are needed for more accurate results (17). In our study, while PCT and CRP level were found high in severe sepsis and septic shock patients, these results were not enough to determine the mortality rate.
Recent studies have been mentioned that MR-proADM was superior to other markers to predict mortality rate, but characteristics of patients were different than our study in terms of severity of disease (2,8,20). Most of the participants in these studies had not a severe disease. Huang and co-workers performed a wide series study on 1,653 participants, and they found that MR-proADM was correlated with mortality and severity of disease but not a prognostic value in high risk CAP patients (9).
In present study, MR-proADM was high in all patients, but we didn’t found any correlation between MR-proADM and severity of disease or mortality rate. These results are similar with Huang et al. (9) study, and our results suggest that MR-proADM is not a good prognostic value in patients who have a severe disease.
Many scoring systems have been used to determine prognosis in CAP patients. However PSI is one of the most important scoring systems to predict prognosis, 10% false classification might be found particularly patients who have high PSI level (21). Other disadvantage of PSI is an age dependent estimation failure. Overestimation might be occurring in elderly patients who have high comorbidity, whereas risk assessment can be underestimated in young patients who haven’t any additional diseases. This estimation failure might cause an unnecessary hospital admission due to CAP with low mortality rate. Niederman et al. reported that at least 30-60% of low mortality risk patients admitted to hospital due to CAP (22-24). In present study, we found correlation between MR-proADM and PSI level in terms of augmentation, but this increment was not significantly different between patients who had PSI 4-5 and PSI 1-3. This result is considered that, PSI classification should reevaluate by the researchers.
Narvaez-Rivera et al. (25) performed a study on 33 CAP patients, and they compared SOFA, APACHE II, PSI, and CURB-65 scoring system with some serum markers. They found that SOFA scores were most valuable factor in determining high risk patients. In present study, we found that SOFA score was superior to other serum markers and scoring systems. These results are corelated with Narvaez-Rivera et al. (25) results, and SOFA scores had a good correlation with severity of disease and mortality rate.
Travaglino et al. (26) compared MR-proADM, PCT, and APACHE II scores with suspicion for sepsis on 128 patients, and they found that MR-proADM and PCT were significantly higher according to healthy subjects. They also found that both markers correlated with APACHE II scores. They claim that combination of scores and serum markers is more helpful for the risk assessment (26).
Combination model of MR-proADM and various scoring system has been investigated in many studies. Crain and his co-workers compared MR-proADM with PSI score and PSI only, and they found a high accuracy rate in MR-proADM and PSI combination to predict treatment failure and prognosis (8,27). According to competence network or the study of community acquired pneumonia (CAPTNEZ) study, combination of MR-proADM and CURB65 had a better accuracy rate to predict prognosis in CAP patients (28).
In our study, when we assessed various scoring system with MR-proADM, SOFA score plus MR-proADM was a most remarkable combination in sepsis and septic shock subjects. MR-proADM, SOFA, and APACHE II scores were also successful to predict both 4- and 8-week mortality rates.
In our study we have some limitations. We analyzed only severe sepsis patients in study group; therefore number of patients in our study was limited. We tried to provide homogeneity in study group in terms of comorbidity, but it was not adequate due to study design.
Conclusions
In conclusion, MR-proADM was found higher in each step of the disease patients who have CAP. Increasing of MR-proADM level was not significant in high risk patients according to PSI risk assessment. SOFA score was a most important indicator for risk evaluation in severe sepsis and septic shock patients, and combination SOFA and MR-proADM provided a high sensitivity and specifity. When MR-proADM is used with scoring systems, physicians can get good results in terms of prediction of mortality and prognosis in CAP patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001;29:1303-10. [PubMed]
- Christ-Crain M, Morgenthaler NG, Struck J, et al. Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: an observational study. Crit Care 2005;9:R816-24. [PubMed]
- Linscheid P, Seboek D, Zulewski H, et al. Autocrine/paracrine role of inflammation-mediated calcitonin generelated peptide and adrenomedullin expression in human adipose tissue. Endocrinology 2005;146:2699-708. [PubMed]
- Marutsuka K, Nawa Y, Asada Y, et al. Adrenomedullin and proadrenomudullin N-terminal 20 peptide (PAMP) are present in human colonic epithelia and exert an antimicrobial effect. Exp Physiol 2001;86:543-5. [PubMed]
- Eto T. A review of the biological properties and clinical implications of adrenomedullin and proadrenomedullin N-terminal 20 peptide (PAMP), hypotensive and vasodilating peptides. Peptides 2001;22:1693-711. [PubMed]
- Nishio K, Akai Y, Murao Y, et al. Increased plasma concentrations of adrenomedullin correlate with relaxation of vascular tone in patients with septic shock. Crit Care Med 1997;25:953-7. [PubMed]
- Struck J, Tao C, Morgenthaler NG, et al. Identification of an adrenomedullin precursor fragment in plasma of sepsis patients. Peptides 2004;25:1369-72. [PubMed]
- Christ-Crain M, Morgenthaler NG, Stolz D, et al. Pro-adrenomedullin to predict severity and outcome in community-acquired pneumonia Crit Care 2006;10:R96. [PubMed]
- Huang DT, Angus DC, Kellum JA, et al. Midregional proadrenomedullin as a prognostic tool in community acquired pneumonia. Chest 2009;136:823-31. [PubMed]
- Ozlu T, Bülbül Y, Alatas F, et al. Consensus report on diagnosis and treatment of community-acquired pneumonia in adults. Toraks 2009;10:1-24. Available online: http://toraks.dergisi.org/text.php3?id=639
- Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003;31:1250-6. [PubMed]
- Knaus WA, Zimmerman JE, Wagner DP, et al. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 1981;9:591-7. [PubMed]
- Vincent JL, de Mendonça A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 1998;26:1793-800. [PubMed]
- Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003;58:377-82. [PubMed]
- Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination: relevant or relic? Arch Intern Med 1999;159:1082-7. [PubMed]
- Kopterides P, Tsangaris I. Procalcitonin and sepsis: recent data on diagnostic utility prognostic potential and therapeutic implications in critically ill patients. Minerva Anestesiol 2012;78:823-35. [PubMed]
- Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Crit Care 2010;14:R15. [PubMed]
- Suberviola B, Castellanos-Ortega A, Llorca J, et al. Prognostic value of proadrenomedullin in severe sepsis and septic shock patients with community acquired pneumonia. Swiss Med Wkly 2012;142:w13542. [PubMed]
- Brunkhorst FM, Al-Nawas B, Krummenauer F, et al. Procalcitonin, C-reactive protein and APACHE II score for risk evaluation in patients with severe pneumonia. Clin Microbiol Infect 2002;8:93-100. [PubMed]
- Potocki M, Breidthardt T, Reichlin T, et al. Midregional pro-Adrenomedullin in addition to b-type natriuretic peptides in the risk stratification of patients with acute dyspnea: an observational study. Crit Care 2009;13:R122. [PubMed]
- Aronsky D, Haug PJ. Assessing the quality of clinical data in a computer-based record or calculating the pneumonia severity index. J Am Med Inform Assoc 2000;7:55-65. [PubMed]
- Restrepo MI, Mortensen EM, Velez JA, et al. A comparative study of community-acquired pneumonia patients admitted to the Ward and the Intensive Care Unit. Chest 2008;133:610-7. [PubMed]
- Valencia M, Badia JR, Cavalcanti M, et al. Pneumonia severity index class V patients with community-acquired pneumonia: characteristics, outcomes, and value of severity scores. Chest 2007;132:515-22. [PubMed]
- Niederman MS. Making sense of scoring systems in community acquired pneumonia. Respirology 2009;14:327-35. [PubMed]
- Narvaez-Rivera RM, Rendon A, Salinas-Carmona MC, et al. Soluble RAGE as a severity marker in community acquired pneumonia associated sepsis. BMC Infect Dis 2012;12:15. [PubMed]
- Travaglino F, De Berardinis B, Magrini L, et al. Utility of Procalcitonin (PCT) and Mid regional pro-Adrenomedullin (MR-proADM) in risk stratification of critically ill febrile patients in Emergency Department (ED). A comparison with APACHE II score. BMC Infect Dis 2012;12:184. [PubMed]
- Courtais C, Kuster N, Dupuy AM, et al. Proadrenomedullin, a useful tool for risk stratification in high Pneumonia Severity Index score community acquired pneumonia. Am J Emerg Med 2013;31:215-21. [PubMed]
- Krüger S, Ewig S, Giersdorf S, et al. Cardiovascular and inflammatory biomarkers to predict short- and longterm survival in community-acquired pneumonia: Results from the German Competence Network, CAPNETZ. Am J Respir Crit Care Med 2010;182:1426-34. [PubMed]