Risk factors for postoperative complications after lung resection for non-small cell lung cancer in elderly patients at a single institution in China
Introduction
Lung cancer remains the most frequent cancer worldwide with an estimated 1.8 million new cases (13% of total cancer incidence) and 1.6 million deaths (20% of total cancer mortality) in 2012 (1). Non-small cell lung cancer (NSCLC) constitutes roughly 80% of all lung cancer cases, and more than 50% of NSCLC patients are older than 65 years while over 30% are at least 70 years old at diagnosis (2). According to the statistics from the International Agency for Research on Cancer (IARC), the morbidity and mortality rates of lung cancer in China are highest in the world (1). In addition, the World Health Organization estimates that the annual lung cancer mortality rate in China may reach 1 million by 2025 (3).
Resection still represents the main curative treatment modality for patients with NSCLC. Recent data suggest that pulmonary resection for lung cancer is justified in elderly patients and that age itself is not a contraindication for surgical intervention (4,5), even in octogenarians (6). However, morbidity and mortality rates after pulmonary resections increase with increasing age, especially in elderly patients with severe comorbidities (7,8). As a consequence of growing and ageing populations in China, reducing postoperative complications and mortality is a major issue and still represents a clinical challenge frequently-faced by the thoracic surgeon.
The aim of the present study is to perform a statistical assessment of risk factors for postoperative complications after pulmonary resection for NSCLC in elderly patients at our institution by conducting a retrospective review.
Materials and methods
Approval for the study was obtained and the need for individual patient consent was waived by the Institutional Review Board. A prospectively maintained database of all patients undergoing thoracic surgery for lung cancer, approved by the Institutional Review Board, was used to identify those patients greater than or equal to 70 years of age who underwent pulmonary resection for NSCLC by either an open approach or by a thoracoscopic approach between January 2003 and December 2013 in the Department of Thoracic Surgery at Beijing Chest Hospital. Excluded patients included those who underwent an exploratory thoracotomy or a wedge biopsy; those with a history of preoperative chemotherapy or radiotherapy; histologic diagnosis of small cell carcinoma; and those with incomplete data.
Demographic, clinical variables, preoperative functional status, tumor characteristics, intraoperative details, and postoperative course were obtained from the institutional database that included all patients who had undergone thoracic surgery. The following risk factors were evaluated: gender, smoking history, a history of previous thoracic surgery, previous diseases, pulmonary functions, patient health status, pathologic stage, type of surgery, and duration of surgery. The postsurgical (pathologic) stages of the patients were based on the seventh TNM Classification of Malignant Tumors. Those patients who were diagnosed and treated before 2009 were re-staged according to the revised TNM Staging System (9). Histologic typing occurred according to The World Health Organization Histologic Typing of Lung Tumors (10). In classifying the severity of patient comorbidities, each patient was scaled objectively on the Charlson Comorbidity Index (CCI) based on information collected from the patient medical records (11). Hypertension was not classified as co-morbidity. The five-grade classification of the American Society Anesthesiology (ASA) was used as a composite index of a patient’s overall health status. Never-smokers were defined as patients who had never smoked or had smoked fewer than 100 cigarettes in their lifetime. Postoperative complications were classified as minor (non-life-threatening) and major (potentially life-threatening), occurring within 30 days of surgery. Hospital mortality included all deaths during the first 30 days after operation, or during the postoperative hospital stay (12).
All patients were performed either by VATS or standard posterolateral thoracotomy under general anesthesia with single lung ventilation. Thoracoscopic lobectomy was performed without any rib spreading with the thoracoscope placed in the eighth intercostal space in the midaxillary line and a 3-4 cm anterior utility incision in the fifth intercostal space. The detailed technique of VATS lobectomy employed at our institution has been previously described elsewhere (13). Posterolateral thoracotomy in most patients was performed with division of the latissimus dorsi muscle and sparing of the serratus anterior muscle. All operations were performed by the same surgical team with extensive experience in thoracoscopic and open procedures. The decision to employ either a VATS or thoracotomy approach was made by the surgeon. The extended operation was defined as the resection of a pulmonary lobe associated with chest wall resection, additional parenchyma from an adjacent lobe, major vascular resection, or bronchoplastic procedure. After pulmonary resection, a complete systemic mediastinal lymph node dissection or sampling is performed. Patient controlled intravenous analgesia (PCIA) for postoperative pain relief was offered to all patients regardless of the planned operative approach.
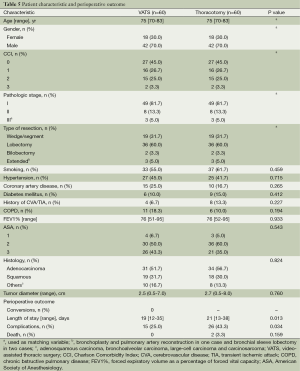
To determine if the utilization of VATS for lung resection for NSCLC in elderly patients’ results in decreased complications compared with thoracotomy, we then performed a matched case-control study to evaluate the perioperative outcomes after pulmonary resection by VATS versus thoracotomy. Cases were defined as patients undergoing VATS pulmonary resection, while controls were those patients having a traditional thoracotomy. Controls were individually matched to cases according to five baseline variables by ratio 1:1. (I) Age: up to 2 years older or younger; (II) gender: male, female; (III) the CCI: 0, 1, 2, 3; (IV) pathologic stage: I, II, IIIa; (V) pulmonary resection types: wedge resection or segmentectomy, lobectomy, bilobectomy, extended resection. The perioperative outcomes of two groups were compared.
A logistic regression model was used in univariate and multivariate analyses to identify risk factors for postoperative complications. The data are presented as frequency and percentage for categoric variables and as median and range for continuous variables. The Wilcoxon rank test were used to compare continuous variables and the χ2 or Fisher exact tests were used for categorical variables and a P value less than 0.05 was considered to be significant. Variables with a P value less than 0.2 in univariate analysis were entered into a multivariate analysis. The statistical software SPSS 13.0 (SPSS Inc, Chicago, IL, USA) was used for all analyses.
Results
Review of the prospective database of thoracic surgical cases performed from January 2003 to December 2013 identified 476 patients who were greater than or equal to 70 years old at the time of surgery and underwent lung resection for NSCLC. Of these 410 patients ultimately underwent thoracotomy, and 66 patients had a successful VATS approach. There were 376 males and 100 females, ranging in age from 70 to 87 years (median age of 73). Nineteen (4.0%) patients were octogenarians.
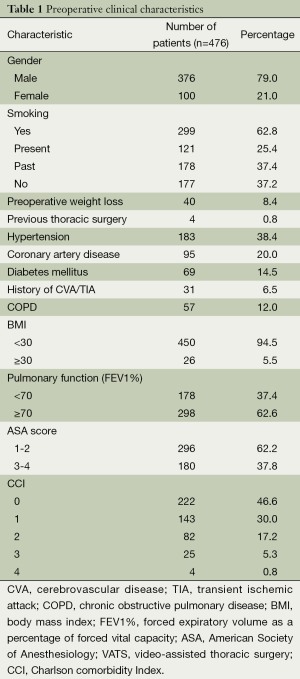
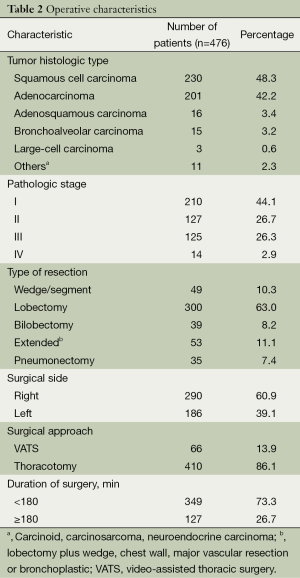
Demographic and preoperative clinical characteristics are shown in Table 1. There were 299 (62.8%) smokers or ex-smokers and 177 (37.2%) non-smokers. The comorbidity rate was 53.4% (254 of 476 patients) and CCI scores of 1, 2, 3, or 4 were assigned to 143, 82, 25 and 4 patients, respectively. Operative characteristics are listed in Table 2. Squamous cell carcinoma was the most common histologic type of cancer (48.3%), followed by adenocarcinoma (42.2%). Pulmonary resection was performed mainly for early disease stages (stage I, 44.1%; stage II, 26.7%; stage III, 26.3%; stage IV, 2.9%). The following types of pulmonary resections were performed: wedge resections or segmentectomies (10.3%), lobectomies (63.0%), bilobectomies (8.2%), extended resections (11.1%), and pnumonectomies (7.4%).
Full table
Full table
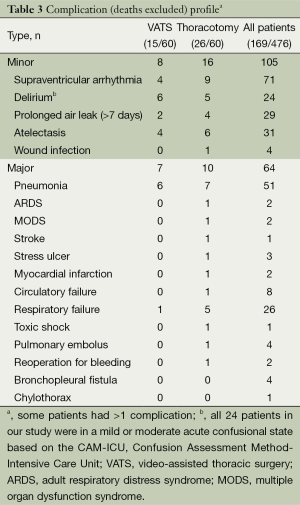
Overall operative mortality was 2.3% (11 patients). The causes of death were respiratory failure (4 patients), circulatory failure (3 patients), pulmonary embolus (3 patients), and toxic shock (1 patient). The mortality rate for lobectomy was 1.0% (3 of 300 patients), extended 7.5% (4 of 53 patients), and pneumonectomy 11.4% (4 of 35 patients, two left sided and two right sided). The number of deaths was too low to identify any significant risk factors. Postoperative complications are demonstrated in Table 3. The overall morbidity was 35.5% (169 patients). Minor complications occurred in 105 patients (22.1%) and major complications developed in 64 patients (13.4%). Two complications were seen in 41 patients (8.6%), and 20 patients (4.2%) developed three or more complications. The most common complications were supraventricular arrhythmia (14.9%) and pneumonia (10.7%). Only two patients underwent reoperation for postoperative bleeding.
Full table
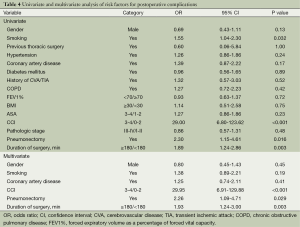
On univariate analysis using the predictors listed in Table 4, smokers (P=0.032), CCI scores of 3-4 (P=0.001), pneumonectomy (P=0.016), and a prolonged surgery (P=0.003) were significantly associated with the occurrence of complications. Gender, previous thoracic surgery, hypertension, diabetes, congestive heart failure, coronary artery disease, history of cerebrovascular disease (CVA)/transient ischemic attack (TIA), chronic obstructive pulmonary disease (COPD), pulmonary functions, body mass index (BMI), ASA, and pathologic stage were not significant predictors of complications. After multiple logistic regression, three independent risk factors for postoperative complications were identified: CCI scores ≥3 (OR =29.95, 95% CI, 6.91-129.88), pneumonectomy (OR =2.26, 95% CI, 1.09-4.71), and prolonged surgical time (OR =1.93, 95% CI, 1.24-3.00).
Full table
After matching for age, gender, the CCI, pathologic stage, and the type of resection, there were 120 patients eligible for analysis, 60 patients in each group. There were no conversions to thoracotomy in the VATS group. The patients in each group were well-matched with respect to preoperative characteristics (Table 5). The median age of patients was 75 years, and there were a higher proportion of men (70%). With respect to smoking status, previous diseases, pulmonary functions, ASA, histologies, and tumor size, no significant difference was noted (Table 5).
Full table
Perioperative outcomes are listed in Table 5. Patients in the VATS group had a shorter length of stay compared with those in the thoracotomy group (median 19 days, range 12 to 35 days versus median 21 days, range 13 to 38 days, P=0.013). In addition, the VATS group had a significantly lower rate of complications compared with the thoracotomy group (25.0% vs. 43.3%, P=0.034). When separated into severity of complications, VATS patients had a decreased incidence of major complications (13.3%) compared with open thoracotomy patients (26.7%). There was no significant difference in the incidence of minor complications. There were no perioperative deaths in the VATS group, whereas there were two deaths (3.3%) in the thoracotomy group although this difference was not statistically significant (P=0.159). One patient died of toxic shock and one died of respiratory failure.
Discussion
This study demonstrates that pulmonary resection can be performed for NSCLC in patients older than 70 with acceptable overall morbidity and mortality (2.3% and 35.5%, respectively). These results are in the range of those published from other multiinstitution and single-institution series (14-16).
Our findings support those of previously published reports that have suggested that age should not be the sole determinant when considering surgery as a treatment option for lung cancer (4,5). In addition, chronologic age is not an absolute risk factor for morbidity and mortality after lung resection. In the present study age was also not a significant risk factor for complications. A number of recent studies have indicated that in carefully selected elderly patients, pulmonary resection can be performed safely with mortality rates similar to that seen in their younger counterparts (14,16-18) The favorable data demonstrated that elderly lung cancer patients should not be denied the curative surgery based on their chronologic age.
The most common reported complications are arrhythmia (range, 4% to 14%) and air leak (range, 7% to 11%) (4,14,17,19), while the most frequently complications in our study were arrhythmia (14.9%) and pneumonia (10.7%). The incidence of air leak lasting more than 7 days was 6.1%. The different diagnostic criteria may partially explain the difference. According to previous literature, prolonged air leakage was defined as that persisting for more than 5 days (17) or 14 days (20), whereas the criteria for persistent air leak in our study was more than 7 days. Extreme variability in terms of incidence of pneumonia after lung resection was reported in both retrospective and prospective studies, with values ranging from 2% to 40% (21). The incidence of postoperative pneumonia in our series was in agreement with the previously published studies. Such variability probably depends on the characteristics of studied populations, antibioprophylaxis, the type of resection, and postoperative management.
The operative mortality rate of 2.3% is well within the range published by other investigators, who reported a hospital mortality ranging from 1.2% to 12.8% (14,17,19). The number of deaths was too low to identify any significant risk factors. We consider that selection bias may have played a role in our favorable results. That is because patients who had a history of neoadjuvant therapy were excluded and these patients most probably represent a group with advanced stage non-small lung cancer.
The CCI in general has been found to be an important prognostic factor in patients operated for cancer (11). Several studies have demonstrated that a Charlson comorbidity grade of 3 to 4 was significantly associated with major complications of surgery in NSCLC patients (7,17). In this study we also found that the CCI is a strong predictor of complications of surgery than individual risk factor in NSCLC elderly patients.
The present study demonstrated that the duration of surgery was one independent significant risk factor for complications. Licker et al. showed that prolonged surgery (≥120 min) was independently associated with an increased risk for postoperative complications (22). In our series, the morbidity rate was higher in patients with surgery time ≥180 min (46.5%) than in patients with surgery time <180 min (31.5%). Surgery time can be influenced by the patient’s status, the complexity of surgery, the surgical approach, and the surgeon’s skill-level. In addition, patients with severe adhesions or incomplete fissures would require longer operating times. We therefore suggest that operations for elderly patients should be performed by a skillful and experienced surgical team and the surgery duration should be limited to the shortest possible time.
The incidence of postoperative complications and the mortality rate in patients who underwent pneumonectomies (morbidity rate, 54.3%; mortality rate, 11.4%) were clearly more than patients who had undergone lesser lung resections (wedge resections and segmentectomies), lobectomies, bilobectomies, or extended resections. Several previous studies have reported that pneumonectomy, especially right-sided pneumonectomy, is associated with higher incidence of postoperative complications when compared with limited resections (12,23). However, Ginsberg et al. (24) showed a lower mortality rate in pneumonectomies in elderly patients (5.9%) compared with lobectomies (7.3%). Also in our series no significant difference was observed between right-sided pneumonectomy and left-sided pneumonectomy. Patient selection bias and low statistical power may account for this observation. Thus, it is still advisable that pneumonectomy should be undertaken with caution, but not avoided if a curative resection can be achieved.
VATS has been proven to be associated with low morbidity and mortality (25). In addition, some authors have reported that postoperative pulmonary function after VATS is better compared with the traditional thoracotomy (26). However, relatively few studies have been done to evaluate the use of VATS in elderly patients (27), or in octogenarians (28). Few studies have showed that a minimally invasive surgery to pulmonary resection results in fewer complications in elderly patients (29), or in octogenarians (30). In the present study we observed that the VATS group had a lower rate of complications and a shorter median length of stay compared with the thoracotomy group. Moreover, VATS patients had a decreased incidence of major complications compared with patients undergoing thoracotomy. However, Koizumi and his colleagues failed to show any difference in morbidity or mortality between VATS and standard thoracotomy in elderly patients (28). This was partially due to a low statistical power (17 thoracoscopy, 15 thoracotomy).
There are strengths and limitations to every study. The main strength of this study is that, compared with other studies, we performed a matched case-control study to eliminate selection bias as rigorously as possible outside of the setting of a randomized, prospective study. Although it is impossible to completely control selection bias in a retrospective study, we attempted to control for all knows contributors. The main limitation of this study is the retrospective nature. Although the data in this study were collected prospectively, the analysis was performed retrospectively. Therefore, unknown confounding variables and inherent selection biases could exist.
Conclusions
In conclusion, pulmonary resection for non-small cell lung carcinoma is justified in patients older than 70 years and its morbidity and mortality are acceptable. On the basis of our findings we concluded that those patients with CCI scores ≥3, those who undergo pneumonectomy, and those with a prolonged surgery are more likely to suffer postoperative complications and therefore need to be closely monitored. Compared with standard thoracotomy, a thoracoscopic approach is associated with a lower incidence of postoperative complications and may prove to be preferable for the elderly patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Stewart BW, Wild CP. eds. World Cancer Report 2014. Lyon: International Agency for Research on Cancer, 2014.
- Gridelli C. Chemotherapy of non-small cell lung cancer in the elderly. Lung Cancer 2002;38 Suppl 3:S67-70. [PubMed]
- World Health Organization. Cancer: fact sheet no. 297. World Health Organization website. 2011. Available online: http://www.who.int/mediacentre/factsheets/fs297/en, accessed September 10.
- Thomas P, Sielezneff I, Ragni J, et al. Is lung cancer resection justified in patients aged over 70 years? Eur J Cardiothorac Surg 1993;7:246-50; discussion 250-1. [PubMed]
- Jack CI, Lye M, Lesley F, et al. Surgery for lung cancer: age alone is not a contraindication. Int J Clin Pract 1997;51:423-6. [PubMed]
- Pagni S, Federico JA, Ponn RB. Pulmonary resection for lung cancer in octogenarians. Ann Thorac Surg 1997;63:785-9. [PubMed]
- Birim O, Maat AP, Kappetein AP, et al. Validation of the Charlson comorbidity index in patients with operated primary non-small cell lung cancer. Eur J Cardiothorac Surg 2003;23:30-4. [PubMed]
- Janssen-Heijnen ML, Houterman S, Lemmens VE, et al. Prognostic impact of increasing age and co-morbidity in cancer patients: a population-based approach. Crit Rev Oncol Hematol 2005;55:231-40. [PubMed]
- Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest 2009;136:260-71. [PubMed]
- The World Health Organization histological typing of lung tumours. Second edition. Am J Clin Pathol 1982;77:123-36.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. [PubMed]
- Myrdal G, Gustafsson G, Lambe M, et al. Outcome after lung cancer surgery. Factors predicting early mortality and major morbidity. Eur J Cardiothorac Surg 2001;20:694-9. [PubMed]
- Yu DP, Han Y, Zhao QY, et al. Pulmonary lobectomy combined with pulmonary arterioplasty by complete video-assisted thoracic surgery in patients with lung cancer. Asian Pac J Cancer Prev 2013;14:6061-4. [PubMed]
- Pagni S, McKelvey A, Riordan C, et al. Pulmonary resection for malignancy in the elderly: is age still a risk factor? Eur J Cardiothorac Surg 1998;14:40-4; discussion 44-5. [PubMed]
- Allen MS, Darling GE, Pechet TT, et al. Morbidity and mortality of major pulmonary resections in patients with early-stage lung cancer: initial results of the randomized, prospective ACOSOG Z0030 trial. Ann Thorac Surg 2006;81:1013-9; discussion 1019-20. [PubMed]
- Fan J, Wang XJ, Jiang GN, et al. Survival and outcomes of surgical treatment of the elderly NSCLC in China: a retrospective matched cohort study. Eur J Surg Oncol 2007;33:639-43. [PubMed]
- Birim O, Zuydendorp HM, Maat AP, et al. Lung resection for non-small-cell lung cancer in patients older than 70: mortality, morbidity, and late survival compared with the general population. Ann Thorac Surg 2003;76:1796-801. [PubMed]
- Cerfolio RJ, Bryant AS. Survival and outcomes of pulmonary resection for non-small cell lung cancer in the elderly: a nested case-control study. Ann Thorac Surg 2006;82:424-9; discussion 429-30. [PubMed]
- Ishida T, Yokoyama H, Kaneko S, et al. Long-term results of operation for non-small cell lung cancer in the elderly. Ann Thorac Surg 1990;50:919-22. [PubMed]
- Okami J, Higashiyama M, Asamura H, et al. Pulmonary resection in patients aged 80 years or over with clinical stage I non-small cell lung cancer: prognostic factors for overall survival and risk factors for postoperative complications. J Thorac Oncol 2009;4:1247-53. [PubMed]
- Schussler O, Alifano M, Dermine H, et al. Postoperative pneumonia after major lung resection. Am J Respir Crit Care Med 2006;173:1161-9. [PubMed]
- Licker M, Spiliopoulos A, Frey JG, et al. Management and outcome of patients undergoing thoracic surgery in a regional chest medical centre. Eur J Anaesthesiol 2001;18:540-7. [PubMed]
- van Meerbeeck JP, Damhuis RA, Vos de Wael ML. High postoperative risk after pneumonectomy in elderly patients with right-sided lung cancer. Eur Respir J 2002;19:141-5. [PubMed]
- Ginsberg RJ, Hill LD, Eagan RT, et al. Modern thirty-day operative mortality for surgical resections in lung cancer. J Thorac Cardiovasc Surg 1983;86:654-8. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Kaseda S, Aoki T, Hangai N, et al. Better pulmonary function and prognosis with video-assisted thoracic surgery than with thoracotomy. Ann Thorac Surg 2000;70:1644-6. [PubMed]
- Asamura H, Nakayama H, Kondo H, et al. Video-assisted lobectomy in the elderly. Chest 1997;111:1101-5. [PubMed]
- Koizumi K, Haraguchi S, Hirata T, et al. Lobectomy by video-assisted thoracic surgery for lung cancer patients aged 80 years or more. Ann Thorac Cardiovasc Surg 2003;9:14-21. [PubMed]
- Cattaneo SM, Park BJ, Wilton AS, et al. Use of video-assisted thoracic surgery for lobectomy in the elderly results in fewer complications. Ann Thorac Surg 2008;85:231-5; discussion 235-6. [PubMed]
- Mun M, Kohno T. Video-assisted thoracic surgery for clinical stage I lung cancer in octogenarians. Ann Thorac Surg 2008;85:406-11. [PubMed]


