FDG PET-CT combined with TBNA for the diagnosis of atypical relapsing polychondritis: report of 2 cases and a literature review
Introduction
Relapsing polychondritis (RP) is a disease of unknown etiology characterized by recurrent non-infectious inflammation of cartilaginous and connective tissues. Previous studies have shown that autoimmunity may play a role in the pathogenesis of this disease (1,2). Clinical presentations of RP vary considerably from patient to patient, and the involvement of multiple organs has been reported. However, there is currently no specific diagnostic method available; as a result, the rates of misdiagnosis and missed-diagnosis are very high, particularly with regard to the early diagnosis of atypical RP.
To date, very few studies have reported the use of 18F-fluorodeoxyglucose positron emission tomography-computed tomography (FDG PET-CT) combined with transbronchial needle aspiration (TBNA) for the diagnosis of RP. Here, we have analyzed the clinical features of two cases of atypical RP that had been diagnosed in our hospital using FDG PET-CT combined with TBNA, and performed a literature review to evaluate the value of this approach in diagnosing RP and in shorting the time to diagnosis in patients with RP.
Methods
Data from two patients with atypical RP, which had been diagnosed in our hospital using FDG PET-CT combined with TBNA, were retrospectively analyzed. Articles published up to June 2014 were searched for in several databases, including the Cochrane Library, PubMed and EMBASE, using “RP” and “PET-CT” as keywords. Duplicated articles were excluded. Information concerning the patient’s age, sex, clinical symptoms, PET-CT features [abnormal uptake sites and the maximum standard uptake value (SUVmax)], and biopsy sites was extracted and analyzed.
Results
Case 1
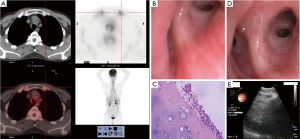
A 42-year-old male patient was admitted to our hospital in 2012 with symptoms of cough and intermittent fever for more than 2 months. The patient had not been diagnosed with any previous disorders, and reported no alcohol consumption or tobacco smoking. The patient had been experiencing cough, expectoration and fever during the preceding 2 months, without obvious predisposing causes. The highest temperature of the patient had been recorded as 39.0 °C. No other symptoms, including chest congestion and shortness of breath, were reported. After a trial of anti-inflammatory medication had resulted in no improvement, the patient had been admitted to our hospital for further diagnosis and treatment. On admission, the temperature of the patient was 36.7 °C, the heart rate 82 beats/minute, respiration 16 times/minute, and blood pressure 115/85 mmHg. No enlargement of the superficial lymph nodes was detected, and breath sounds were clear in the bilateral lungs. CT scanning of the chest was performed, and no abnormalities were found. Routine blood tests revealed a white blood cell count of 5.44×109/L, a neutrophil count of 3.33×109/L, a hemoglobin level of 99 g/L, and a platelet count of 305×109/L. Examination of a panel of tumor biomarkers showed that the levels of neuron-specific enolase, tumor specific growth factor (TSGF) and ferritin were 21.8 ng/mL, 72.4 U/mL and 811.6 ng/mL, respectively. Examination of a panel of lupus, blood transfusion and antineutrophil cytoplasmic antibodies identified no abnormalities. Blood culture, mycobacterium tuberculosis-specific gamma interferon release assays (T-spot), and ultrasound examination of the heart were also performed, and no abnormalities were detected. Increases in erythrocyte sedimentation rate (ESR, 124 mm/h) and C-reactive protein level (CRP, 14.89 mg/L) were found, while assessment of pulmonary function suggested an obstructive disturbance of ventilatory function. A bone marrow biopsy was performed, but the bone marrow smear and culture showed no abnormalities. As the underlying disease could not be diagnosed, FDG PET-CT scanning was performed. There were no abnormalities in the density and distribution of the radioactivity in the bilateral lungs, and no enlargement of the mediastinal and hilar lymph nodes. In addition, no lesions showing abnormal FDG uptake were found in the neck or the organs of the abdominal and pelvic cavities. In contrast, a symmetric increase in uptake was found in the costicartilage, trachea and bilateral bronchial walls, while no enhancement of uptake was identified in the skeletal system of other sites (Figure 1A), suggesting the possibility of chondritis. Therefore, tracheoscopic examination was performed; these revealed mucosal hypertrophy and slight bronchial stenosis, particularly stenosis of the bronchus in the right upper lobe (Figure 1B). The TBNA technique was used to obtain cartilage biopsies, and these showed infiltration of neutrophils, lymphocytes and plasma cells around hyaline cartilage (Figure 1C). These findings helped us to diagnose RP in this patient. Careful re-taking of the medical history revealed that the hearing of the patient had deteriorated during the past 6 months; a hearing test was then performed, and this showed moderate neural hearing loss in both ears. No symptoms or signs of chondritis were evident in the ears and nose, and pain was not elicited by pressure on the costicartilage. Intravenous injections of methylprednisolone (40 mg, qd) were given for 7 days; at the end of this treatment, the temperature of the patient had returned to a normal level, only an occasional cough remained. Intravenous methylprednisolone was then replaced by oral prednisone (10 mg, tid); no fever was identified, and the patient was discharged showing substantial improvement. Follow-up assessments were performed 6 weeks after discharge: no symptoms or discomfort were reported, and tracheoscopic examination showed substantial improvement of the mucosal congestion and edema, with no tracheal stenosis (Figure 1D). In addition, endobronchial ultrasound examination demonstrated normal cartilaginous rings and no thickening of the bronchial wall (Figure 1E).
Case 2
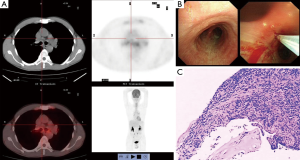
A 51-year-old male patient was admitted to our hospital in 2013, with symptoms of a relapsing cough, expectoration and fever for more than 1 month. Prior to admission, the patient had not been diagnosed with any previous disorders, and no predisposing causes for the symptoms had been identified. The patient had a 20-year history of smoking approximately 1 pack per day. The highest temperature of the patient had been recorded as 38.5 °C. No other symptoms, including chest tightness and shortness of breath, were present. The patient had been admitted to our hospital after the failure of anti-infectious treatments administered in a local hospital. On admission, the temperature of the patient was 37.0 °C, the heart rate 84 beats/minute, respiration 18 times/minute, and blood pressure 110/74 mmHg. There was no enlargement of the superficial lymph nodes, and the breath sounds were clear in the bilateral lungs. CT scanning of the chest demonstrated increased lung markings and enlarged mediastinal lymph nodes. The white blood cell count was 10.64×109/L, the neutrophil count 6.36×109/L, the hemoglobin level 129 g/L, and the platelet count 419×109/L. Abdominal ultrasound examination suggested the presence of a hepatic cyst and gallbladder polyps. Ultrasound examination of the heart found no abnormalities. Other investigations were also performed to evaluate the levels of rheumatoid factor, serum procalcitonin, anti-tuberculosis antibody and 24-hour urinary calcium, but the results were negative. Examinations of panels of blood transfusion, thyroid function, lupus, and antineutrophil cytoplasmic antibodies showed no abnormalities. Blood culture and T-spot also showed no abnormalities. The ESR (57 mm/h) and CRP (15.06 mg/L) of the patient were increased. Examination of the levels of a panel of tumor biomarkers demonstrated that the ferritin level was 697.8 ng/mL. FDG PET-CT scanning was performed to further clarify the diagnosis. No lesions showing abnormal uptake were found in the neck, and the density and distribution of the radioactivity in the bilateral lungs was not abnormal. Although the mediastinal lymph nodes were enlarged, no abnormal uptake of radioactivity was found. In addition, no lesions showing abnormal uptake were found in the organs of the abdominal and pelvic cavities. Increased uptake was found in costicartilage near the xiphisternum, the trachea, and the walls of the bilateral main bronchi. No enhancement of uptake was evident in the skeletal system of other sites. These findings suggested the possibility of chondritis (Figure 2A). As the symptoms of the patient were atypical, and enlargement of the mediastinal lymph nodes was found, bronchoscopic biopsy was performed to exclude malignancy: there were no obvious abnormalities in the cartilaginous rings, whereas congestion and edema of the tracheal mucosa was found, as well as slight bronchial stenosis. The TBNA technique was used to biopsy the S8 lymph nodes (3) (Figure 2B): inflammatory cell infiltration was evident around the cartilage, but tumor cells or granulomatous inflammation were not found (Figure 2C). On the basis of the findings, the patient was diagnosed with RP. The medical history of the patient was carefully re-visited, and additional physical examinations performed; however, no other positive signs were found. After a 10-day course of oral prednisone (10 mg, qd), the temperature of the patient had returned to a normal level, although an occasional cough remained. Follow-up assessments performed 6 months later found no positive signs.
The clinical manifestations of both patients were fever, cough and expectoration, while no other symptoms were reported. Hearing loss was identified in one patient after the medical history was carefully re-taken. Increases in ESR, CRP and ferritin were found in both patients, while the other examinations demonstrated no abnormalities. In both patients, FDG PET-CT revealed increased FDG uptake in costicartilage and/or the trachea, as well as in the walls of the bilateral main bronchi. Although enlargement of the mediastinal lymph nodes was also found in the second case, FDG PET-CT scanning did not show evidence of enhanced FDG uptake in these lymph nodes. The findings of these two cases demonstrate that targeted biopsy of the lesion with TBNA, performed after FDG PET-CT scanning, could facilitate the diagnosis of RP. The time to final diagnosis in these two patients was about 1.5 months.
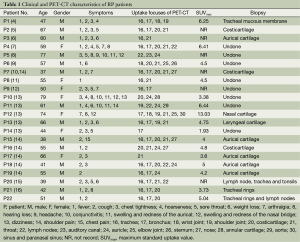
Twelve articles (4-15), involving 20 cases, were identified that reported the diagnosis of RP using PET-CT. Thus, a total of 22 cases (15 males and 7 females; mean age, 55.5 years) of RP, diagnosed using PET-CT, have been reported, including the two cases described in the present study. The main clinical symptoms of these patients included fever and cough. Common features of the PET-CT images included symmetric involvement of cartilage and joints, evident as 18F-FDG hypermetabolic lesions. The SUVmax was recorded for 16 of the 22 cases; it ranged from 1.93 to 13.03, with a mean value of 5.14. Table 1 showed the clinical characteristics and PET-CT features of the 22 patients.
Full table
Discussion
RP is a relapsing degenerative disease of cartilaginous tissues characterized by the involvement of multiple organs and vessels, including the nose, ears, throat, trachea, eyes, joints and cardiac valves; however, the etiology of RP is still not fully understood. Previous studies have suggested that autoimmunity may be associated with the pathogenesis of RP. No ethnicity, sex or age differences have been reported for RP, but most patients with RP are between 40 and 60 years of age (1,2). Currently, most medical practitioners and researchers apply the criteria proposed by Damiani et al. (17) for the diagnosis of RP.
As RP is a rare disease with clinical manifestations that vary from patient to patient, it is very hard to diagnose, especially in patients with atypical symptoms. The early diagnosis of RP is even more challenging (1). The clinical symptoms of the two cases reported here were fever and cough, and no other abnormalities were found. After the diagnosis of RP, the clinical history of each patient was carefully re-taken. In the first case, hearing loss was identified as an additional symptom in the first patient, but there was no involvement of the cartilage of the ears, joints, nose and eyes. FDG PET-CT scanning showed inflammation of the costicartilage, trachea and bilateral main bronchi. In the second case, no involvement of the cartilage of the ears, joints, nose and eyes was identified, and there were no lesions in the cochlea and ear vestibules. FDG PET-CT scanning suggested inflammation in the costicartilage near the xiphisternum, as well as in the trachea and the walls of the bilateral main bronchi. TBNA was used for biopsy of the sites showing increased FDG uptake in FDG PET-CT scans; the results obtained helped to determine the final diagnosis, and no obvious complications occurred. Glucocorticoids were used to treat both of the patients, and effectively alleviated the symptoms. The findings in these two patients suggested that FDG PET-CT could play an important diagnostic role in patients with atypical RP.
Laboratory investigations in these two cases revealed increased ESR and CRP, in accordance with previous studies (18); interestingly, we also found an increased ferritin level in both patients, consistent with the findings of Fujiki et al. (19) In addition, an elevated ferritin level had been found in 4 other cases of RP diagnosed recently in our hospital. These findings suggested that an increased ferritin level could also be valuable in the diagnosis of RP.
Previous studies have shown that FDG PET-CT is of great value in diagnosing diseases presenting as fever of unknown origin, with a sensitivity and specificity of 92% and 94%, respectively (20). FDG is a non-specific imaging agent that can be taken up by tumor tissues to result in an increased SUV; thus, FDG can play an important role in the diagnosis and staging of tumors, the planning of therapeutic strategies, the prediction of prognosis, and the evaluation of treatment efficacy in patients with cancer (21,22). FDG can also accumulate in tissues showing infective or non-infective inflammation, due to their high glucose metabolism and expression of cell surface glucose transporters; the resulting increase in SUV can play a critical role in diagnosing such inflammatory diseases (23-25). In our literature review, 12 articles were identified that described the diagnosis of RP with FDG PET-CT. The first case of RP diagnosed with FDG PET-CT was reported by Nishiyama et al. in 2007 (4); in 2013, we also reported the use of FDG PET-CT for the diagnosis of RP in a patient (16). In the cases reported previously, symmetric, multiple, hypermetabolic lesions were found in the cartilages of the trachea, bronchi, costicartilage, throat and lymph nodes. PET-CT revealed that 86.4% (19/22) of the patients with RP had airway involvement. The SUVmax was reported in 16 of these cases, and ranged from 1.93 to 13.03, with a mean of 5.14. These findings suggested the existence of chondritis, which had been acknowledged to be a reliable indicator of RP. Therefore, FDG PET-CT played an important role in the diagnosis of RP in all 22 of these cases.
Both of the cases reported here were diagnosed within 1.5 months of disease onset. Complete medical records were available in 17 of the 22 cases (including the present 2 cases) diagnosed using FDG PET-CT; the time to diagnosis in these 17 patients was within 6.9 months of onset, significantly shorter than the average time to diagnosis of 20 months (26). Such earlier diagnosis could potentially decrease the risk of the development of late complications. These findings demonstrated that FDG PET-CT could potentially play an important role in the diagnosis of RP, especially atypical RP, and effectively shorten the time to diagnosis.
In 10 of the 22 reported cases, FDG PET-CT was used for re-examination of the patient after treatment had been administered; these assessments showed that FDG uptake had decreased substantially or disappeared after treatment, and that no other hypermetabolic lesions were evident (5-8,11,14). This indicated that FDG PET-CT could also play an important role in the evaluation of treatment efficacy.
For atypical RP patients, the main biopsy sites are costicartilage, aurical cartilage and nasal cartilage. And the primary complication is infection and collapse of auricles (27). However, TBNA, as a minimally invasive and safe technique, has never presented with obvious complication in both adults and children (28,29). The clinical symptoms of the two cases reported here were not typical, and only a limited number of organs (including the cartilage of the trachea and bronchi) were involved. TBNA was used for biopsy of cartilage from the sites with increased FDG uptake, and yielded satisfactory pathologic results with minimal trauma and no complications. This would suggest that combining FDG PET-CT with TBNA could be an effective means with which to diagnose RP. In particular, TBNA might show particular promise for the diagnosis of RP in patients with atypical symptoms, especially those with airway involvement. To our limited knowledge, the present study is the first to report the application of TBNA for pathologic examinations of patients with RP, and the first to report the use of endobronchial ultrasound to examine the tracheal walls after treatment (this showed normal cartilaginous rings and no thickening of the tracheal wall). However, endobronchial ultrasound examination (30) was not performed in these two cases before treatment. In the second case reported here, there was enlargement of the mediastinal lymph nodes, a very rare finding in previous studies (7,14,15); moreover, biopsy of the mediastinal lymph nodes using TBNA technique played an important role in the differential diagnosis. In addition, the use of tracheoscopic examination to observe the airway and obtain biopsies of the tracheal mucosa may also prove valuable for the differential diagnosis of RP from bronchial asthma and other trachea-involving diseases (31,32). Besides bronchoscope and TBNA technique, the dynamic expiratory CT and three-dimensional image reconstructions are valuable for diagnosis and following up of RP involved bronchotracheal (33).
In summary, FDG PET-CT scanning was able effectively to display increased FDG uptake in the trachea, bronchi, costicartilage and joints; these findings could be used as reliable signs of joint cartilage involvement in RP. PET-CT revealed that 86.4% of the patients with RP had airway involvement, so we recommend that clinicians should improve their understanding of RP, and apply TBNA and targeted biopsy in the diagnosis of this disease in order to shorten the time to diagnosis.
Acknowledgements
We thanked Ling-Chuan Guo (Department of Pathology, The First Affiliated Hospital of Soochow University) for interpreting the pathological images.
Funding: This study was supported by Jiangsu provincial special program of medical science (No: BL2012023), youth science and technology project of Suzhou City (No: KJXW2012001), Clinical key speciality project of China, and National Natural Science Foundation of China (No: 81300026).
Disclosure: The authors declare no conflict of interest.
References
- Sharma A, Gnanapandithan K, Sharma K, et al. Relapsing polychondritis: a review. Clin Rheumatol 2013;32:1575-83. [PubMed]
- Chopra R, Chaudhary N, Kay J. Relapsing polychondritis. Rheum Dis Clin North Am 2013;39:263-76. [PubMed]
- Zhang Y, Wang KP. Evolution of transbronchial needle aspiration - a hybrid method. J Thorac Dis 2013;5:234-9. [PubMed]
- Nishiyama Y, Yamamoto Y, Dobashi H, et al. [18F]fluorodeoxyglucose positron emission tomography imaging in a case of relapsing polychondritis. J Comput Assist Tomogr 2007;31:381-3. [PubMed]
- De Geeter F, Vandecasteele SJ. Fluorodeoxyglucose PET in relapsing polychondritis. N Engl J Med 2008;358:536-7. [PubMed]
- Yokoyama T, Koyama N, Kodama K, et al. F-fluorodeoxyglucose positron emission tomography for relapsing polychondritis as a diagnostic approach and evaluation of disease activity. BMJ Case Rep 2009:1591.
- Sato M, Hiyama T, Abe T, et al. F-18 FDG PET/CT in relapsing polychondritis. Ann Nucl Med 2010;24:687-90. [PubMed]
- Cassone G, Lo Gullo A, Bajocchi G, et al. [18F]fluorodeoxyglucose positron emission tomography imaging in a case of relapsing polychondritis. Rheumatology (Oxford) 2012;51:1813. [PubMed]
- Czepczyński R, Guzikowska-Ruszkowska I, Wyszomirska A. Relapsing polychondritis detected in PET/CT. Eur J Nucl Med Mol Imaging 2012;39:1366-7. [PubMed]
- Deng H, Chen P, Wang L, et al. Relapsing polychondritis on PET/CT. Clin Nucl Med 2012;37:712-5. [PubMed]
- Blanc-Caille M, Beynat C, Blot M, et al. Isolated tracheobronchial involvement by atrophic polychondritis: role of PET scanning. Rev Mal Respir 2012;29:903-7. [PubMed]
- Honne K, Nagashima T, Onishi S, et al. Fluorodeoxyglucose positron emission tomography/computed tomography for diagnostic imaging in relapsing polychondritis with atypical manifestations. J Clin Rheumatol 2013;19:104-5. [PubMed]
- Yamashita H, Takahashi H, Kubota K, et al. Utility of fluorodeoxyglucose positron emission tomography/computed tomography for early diagnosis and evaluation of disease activity of relapsing polychondritis: a case series and literature review. Rheumatology (Oxford) 2014;53:1482-90. [PubMed]
- Wang J, Li S, Zeng Y, et al. 18F-FDG PET/CT is a valuable tool for relapsing polychondritis diagnose and therapeutic response monitoring. Ann Nucl Med 2014;28:276-84. [PubMed]
- Mahida RY, Bowman S, Naidu B, et al. Positron emission tomography aids diagnosis of relapsing polychondritis. BMJ Case Rep 2014:203367.
- Chen T, Jiang JH, Ling CH, et al. Relapsing polychondritis diagnosed by transbronchial needle aspiration and (18)F-fluorodeoxyglucose positron emission tomography/computed tomography. Chin Med J (Engl) 2013;126:3930. [PubMed]
- Damiani JM, Levine HL. Relapsing polychondritis – report of ten cases. Laryngoscope 1979;89:929-46. [PubMed]
- Keidel S, McColl A, Edmonds S. Sweet’s syndrome after adalimumab therapy for refractory relapsing polychondritis. BMJ Case Rep 2011;2011.
- Fujiki F, Tsuboi Y, Hashimoto K, et al. Non-herpetic limbic encephalitis associated with relapsing polychondritis. J Neurol Neurosurg Psychiatry 2004;75:1646-7. [PubMed]
- O’Doherty MJ, Barrington SF, Campbell M, et al. PET scanning and the human immunodeficiency virus-positive patient. J Nucl Med 1997;38:1575-83. [PubMed]
- Nogami Y, Iida M, Banno K, et al. Application of FDG-PET in cervical cancer and endometrial cancer: utility and future prospects. Anticancer Res 2014;34:585-92. [PubMed]
- Ito K, Shimoji K, Miyata Y, et al. Prognostic value of post-treatment 18F-FDG PET/CT for advanced head and neck cancer after combined intra-arterial chemotherapy and radiotherapy. Chin J Cancer Res 2014;26:30-7. [PubMed]
- Ying Z, Wang X, Song Y, et al. Prognostic value of interim 18F-FDG PET/CT in diffuse large B-cell lymphoma. Chin J Cancer Res 2013;25:95-101. [PubMed]
- Kumar R, Basu S, Torigian D, et al. Role of modern imaging techniques for diagnosis of infection in the era of 18F-fluorodeoxyglucose positron emission tomography. Clin Microbiol Rev 2008;21:209-24. [PubMed]
- Glaudemans AW, de Vries EF, Galli F, et al. The use of (18)F-FDG-PET CT for diagnosis and treatment monitoring of inflammatory and infectious diseases. Clin Dev Immunol 2013;2013:623036.
- Ananthakrishna R, Goel R, Padhan P, et al. Relapsing polychondritis – case series from South India. Clin Rheumatol 2009;28:S7-S10. [PubMed]
- O’Connor Reina C, Garcia Iriarte MT, Barron Reyes FJ, et al. When is a biopsy justified in a case of relapsing polychondritis? J Laryngol Otol 1999;113:663-5. [PubMed]
- Agarwal R, Aggarwal AN, Gupta D. Efficacy and safety of conventional transbronchial needle aspiration in sarcoidosis: a systematic review and Meta-analysis. Respir Care 2013;58:683-93. [PubMed]
- Goussard P, Gie RP, Kling S, et al. The diagnostic value and safety of transbronchial needle aspiration biopsy in children with mediastinal lymphadenopathy. Pediatr Pulmonol 2010;45:1173-9. [PubMed]
- Miyazu Y, Miyazawa T, Kurimoto N, et al. Endobronchial ultrasonography in the diagnosis and treatment of relapsing polychondritis with tracheobronchial malacia. Chest 2003;124:2393-5. [PubMed]
- Sato R, Ohshima N, Masuda K, et al. A patient with relapsing polychondritis who had been diagnosed as intractable bronchial asthma. Intern Med 2012;51:1773-8. [PubMed]
- Haas AR, Vachani A, Sterman DH. Advances in diagnostic bronchoscopy. Am J Respir Crit Care Med 2010;182:589-97. [PubMed]
- Nakazato Y, Mizoguchi F, Kohsaka H, et al. A case of relapsing polychondritis initially presenting with bronchial chondritis. Mod Rheumatol 2014. [Epub ahead of print]. [PubMed]


