Non-intubated complete thoracoscopic bronchial sleeve resection for central lung cancer
Introduction
Bronchial sleeve resection of lung tumors has emerged as an effective approach which not only removes the lesion but also avoids pneumonectomy, thereby reducing surgical mortality and maximizing lung function and long-term survival (1). Chen et al. reported a video-assisted thoracic surgery (VATS) lobectomy for lung cancer under non-intubated epidural anesthesia, which demonstrated acceptable safety and feasibility (2). However, there are no reports describing bronchial sleeve resection under non-intubated anesthesia. Here, we describe a case of complete endoscopic bronchial sleeve resection of right lower lung cancer under non-intubated epidural anesthesia.
Case report
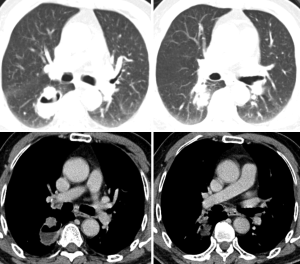
A 70-year-old man presented with a mass in the right lower lung during physical examination. Lung function tests showed forced vital capacity (FVC) of 73.1% and forced expiratory volume in 1 s (FEV1) of 71.5%. Computed tomography (CT) showed a mass at the dorsal segment of the lower right pulmonary lobe (Figure 1), measuring approximately 3×4 cm2, as a thick-walled eccentric cavity. On November 11, 2013, the patient underwent complete thoracoscopic resection under non-intubated epidural anesthesia. Intramuscular midazolam (0.07 mg/kg) and atropine (0.01 mg/kg) were administered at 30 min before anesthesia. Epidural puncture was performed at the T7-8 intervertebral space, with the epidural catheter tip pointed towards the head and fixed after confirming successful placement. Following epidural injection of 0.375% ropivacaine and a test dose of 2 mL ropivacaine, the patient was observed for 5 min for signs of total spinal anesthesia. If total spinal anesthesia was not achieved, two more injections of 0.375% ropivacaine were administered, totaling 8 mL.
With a mask to supply oxygen and remove nitrogen, 2 μg/mL of intravenous propofol was given via target-controlled infusion (TCI) in combination with 0.2 μg/kg intravenous infusion of sufentanil. When adequate sedation was achieved, a laryngeal mask airway (LMA) was inserted and the anesthesia machine was connected to provide simultaneous intermittent mandatory ventilation (SIMV). Arterial catheterization was performed at the right internal jugular vein and the radial artery on the non-operative side.
Epidural injection of 4 mL 0.375% ropivacaine was administered at an interval of 60 min. Continuous intravenous infusion of 1.0-1.5 μg/mL propofol was performed via TCI. Continuous infusion of remifentanil 0.03 μg/kg·min and dexmedetomidine hydrochloride 0.5-1.0 μg/kg·h was administered to maintain sedation. An intraoperative spectrum analyzer was used to monitor the sedative effect, with the bispectral index (BIS) maintained at 40-60. The sedation depth was adjusted according to the monitored parameters. Spontaneous breathing was maintained, with a respiratory rate of 12-20 beats/min.
To suppress the cough reflex caused by lung tissue stretch during the thoracoscopic operation, the intrathoracic vagus nerve was blocked. Under direct vision in thoracoscopy, 3-5 mL of 0.375% ropivacaine was injected near the vagus nerve inferior to the mediastinal pleura above the azygos arch adjacent to the trachea.
The approach for non-intubated epidural thoracoscopic surgery was the 3-port method. With the patient in a left lateral position, the endoscopic observation port was made in the 7th intercostal space at the anterior axillary line, the working port in the 5th intercostal space at the anterior axillary line, and the auxiliary port in the 7th intercostal space at the posterior axillary line. Using a 30° endoscope, the observation field covered the entire chest cavity. Using the connection between the operated side and the outer atmosphere and a gentle push on the lesion side, an iatrogenic pneumothorax was formed to collapse the right lung. After vagus nerve blockade, exploration of the dorsal side of the right lower lung was performed, where a mass measuring 4×5×5 cm3 was found, with evident pleural surface indentation. Johnson’s endoscopic automatic stapler was initially used to isolate the incomplete fissure, and the right lower pulmonary artery and vein were incised. The right lower lobular bronchus was then similarly transected, sent for frozen biopsy and shown to be “bronchial margin residual cancer”. While waiting for the pathological result, systematic lymphadenectomy was performed. To preserve the right and middle lung, bronchial sleeve resection was planned, and the surgery was continued without switching to intubation. The right middle lobe and the bronchi in the middle segment were transected at the root. The frozen pathology showed no residual lesions in the margin of the intermediate segment and the proximal middle bronchus. The right middle lobular bronchus was then joined with the right intermediate bronchus, and was continuously sutured with single 3-0 Prolene suture silk. After anastomosis, a pressurized balloon was applied in conjunction with laryngeal mask ventilation to expand the lungs, and no leakage was observed at the bronchial anastomosis. Upon confirmation of hemostasis, the operation was completed.
Results
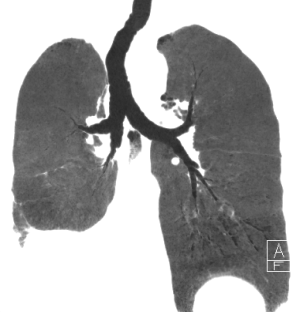
The operation time was 165 min, involving 25 min of bronchial anastomosis and 120 mL blood loss. Five groups of a total of 18 lymph nodes were dissected during surgery. Histopathology results were as follows: moderately differentiated squamous cell carcinoma of the right lower lung, stump carcinoma in situ of the lower lobe bronchus, no tumor in the proximal margins of the right middle lobe and intermediate bronchi, and no lymph node metastasis in any dissected group (0/18). The patient did not require assisted breathing postoperatively. He was able to drink and eat at 4 h postoperatively and was mobile at postoperative day 1. At postoperative day 3, the drainage was removed, and no leaks, pulmonary infection, atelectasis, bronchial fistula, or other complications were observed. He was discharged on postoperative day 6. Pulmonary CT at 1 month postoperatively showed no anastomotic strictures (Figure 2).
Comment
In the present case, since there was a stump residual tumor in the bronchus after lobular resection, we switched to the sleeve resection technique. Given that the patient was stable and the advantage of reduced operative time required for bronchial anastomosis, the non-intubated anesthetic approach was undertaken with the hope of avoiding further injury. Therefore, we performed bronchial sleeve resection under non-intubated anesthesia with satisfactory results, demonstrating that non-intubated anesthesia could be successfully used in not only conventional VATS lobectomy but also for complicated bronchial anastomosis.
To avoid perioperative respiratory failure, non-intubated epidural anesthesia is usually performed only in a select group of patients, with estimated operation time within 3 h and have ASA grade I-II, body mass index <25, and good lung function reserves. In such patients, SPO2 ≥90% can be maintained (2-4). In this patient, since we needed to open the airway for bronchial sleeve resection, which stopped the inhalation of oxygen from the nostrils, the inhaled oxygen concentration was reduced and the SPO2 briefly decreased to 80%. We therefore provided assisted ventilation with a laryngeal mask and balloon to increase the oxygen flow and ventilation, rapidly improving the SPO2 to a safe range of 90-95%, reversing the hypoxemia while reducing CO2 reabsorption. After completing bronchial anastomosis, the patient’s ventilation recovered immediately, and hypoxemia and hypercapnia improved significantly.
In conclusion, thoracoscopic bronchial resection under non-intubated epidural anesthesia can be performed, allowing successful removal of the tumor while retaining adequate functionality of the lung tissue. The patient recovered rapidly, awakened quickly postoperatively, began to eat and drink and was mobile soon after surgery, with a short hospital stay.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Schmid T, Augustin F, Kainz G, et al. Hybrid video-assisted thoracic surgery-robotic minimally invasive right upper lobe sleeve lobectomy. Ann Thorac Surg 2011;91:1961-5. [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [PubMed]
- Dong Q, Liang L, Li Y, et al. Anesthesia with nontracheal intubation in thoracic surgery. J Thorac Dis 2012;4:126-30. [PubMed]
- Chen KC, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lung resection: a 3-year experience with 285 cases in a single institution. J Thorac Dis 2012;4:347-51. [PubMed]