Primary intravascular large B-cell lymphoma of the lung: a review and case report
Background
Intravascular large B-cell lymphoma (IVLBCL) of lung is a rare type of extranodal large B-cell lymphoma (LBCL) characterized by the selective growth of lymphoma cells within the lumina of vessels, particularly within capillaries, with sparing of larger arteries and veins. The clinical presentation is highly variable due to occlusion of small vessels or capillaries in different organ systems. This is an aggressive lymphoma with poor prognosis that in part reflects frequent delays in diagnosis due to above variable symptoms. The most common clinical manifestations involve central nervous system (CNS) presentations, cutaneous lesions, fever, or hemophagocytic syndrome. Although autopsy findings have revealed that pulmonary involvement is common in this disease, primary presentation in the lungs is distinctly uncommon and has been rarely described. Here we report a case with its predominant clinical manifestation as interstitial lung disease, which was finally diagnosed as IVLBCL by biopsy. The clinical features, histopathological characteristics, and differential diagnosis of primary IVLBCL were also discussed in this article. Our patient was diagnosed with the help of the bronchial lung biopsy (TBLB). The clinical features, histopathological characteristics, and differential diagnosis of primary IVLBCL were also discussed in this article.
Case presentation
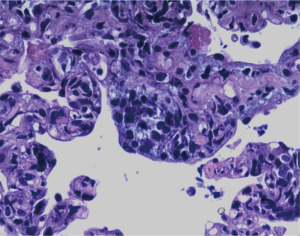
A 35-year-old, previously healthy woman presented to our hospital, with one-month history of cough, breathlessness and fever for two weeks. At a local hospital, based on the radiological findings, she was tentatively diagnosed with pulmonary infection and treated with various antibiotics and an intermittent use of methylprednisolone (40 mg/d). Her fever remained constant, and her breathlessness was worsening even after treatment. She was a housekeeper and lived in Beijing for ten years. She denies any dust exposure or illicit drug use. At her initial presentation (day 1), she appeared well, and vital signs showed blood pressure of 106/54 mmHg, temperature 38.6 °C, heart rate 112 beats/min, respiratory rate 23 breaths/min and oxygen saturation 92-95% (FIO2 =5 L/min). Physical examination showed emaciation and no inspiratory fine crackles and superficial lymphadenopathy was noted. Serum laboratory examinations showed a mild decrease in leucocyte count (3,600 μL); hemoglobin (72 g/L) and marked elevation of lactate dehydrogenase (LDH; 1,554 IU/L), C-reactive protein (175 U/L), procalcitonin (0.331 ng/mL), β2 microglobulin (5.22 mL) and antinuclear antibodies, and antineutrophil cytoplasmic antibodies were negative. Blood gas analysis showed pH 7.406, PaCO2 33.5 mmHg, PaO2 64.2 mmHg. Chest CT-scan showed diffuse interstitial shadows (Figure 1). Lung function test showed decline in diffusion and a mild restrictive ventilatory disorder.
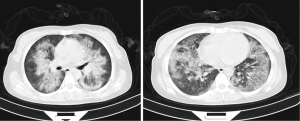
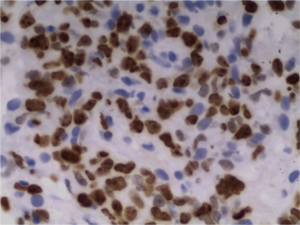
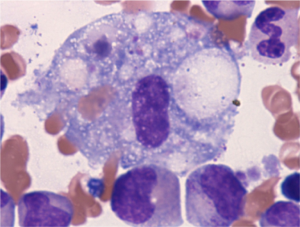
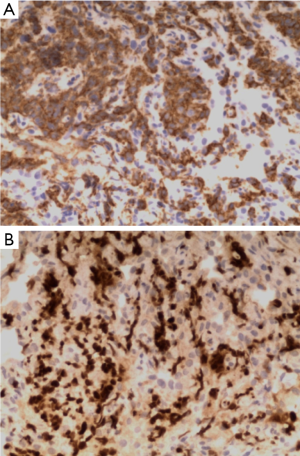
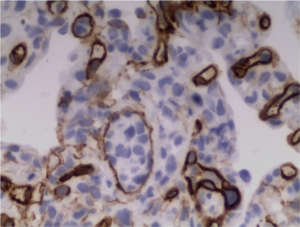
Echocardiography showed moderate pulmonary hypertension (mean pulmonary artery pressure of 43 mmHg). After admission, prophylactic treatment was given, but her fever persisted intermittently (temperature range, 37-39 °C), with oxygen saturation fluctuations in the 92-95% (nasal 5 L/min). A TBLB was immediately performed. On HE staining, the biopsied specimen showed accumulation of abundant atypical lymphocytes in the capillary vessels (Figure 2). Immunohistochemical (IHC) staining showed cells were positive for CD20, Pax5 (Figure 3A,B), BCL2, BCL6 and MUM-1 and negative for CD3, CD10, CD2, CD30, CD34 (Figure 4), CD5, CD56, CD68, EBER, Syn, TTF-1, Granzyme B, and P63. The mean Ki-67 proliferation rate was 60% (Figure 5), indicating the tumour was in an active growing status. Bone marrow biopsy specimen revealed hyperplastic bone marrow, and atypical lymphocytes (9%) were also found (Figure 6).
Based on thorough history and investigation, the patient was diagnosed with IVLBCL. She was treated with R-CHOP (rituximab 600 mg, the day before chemotherapy, cyclophosphamide 1.0 g on day 1 + doxorubicin 60 mg on day 1 and day 2 + leurocristime 2 mg on day 1 + prednisone 60 mg from day 1 to day 9, daily) for one cycle.
Due to severe respiratory failure, the patient died from multiple organ failure a week after the diagnosis.
Discussion
Pfleger and Tappeiner first described IVLBCL in 1958. It is characterized by tumor cells located almost entirely in the intravascular, peripheral blood and bone marrow which makes it difficult to correctly differentiate from other tumors and it is regarded as a source of endothelial cells of the tumor. With the development of immunohistochemical and monoclonal antibody technology, it has been classified as a special type of lymphoma. In 2008 WHO identified it as a rare type of non-Hodgkins lymphoma (NHL). The main characteristics of this type of lymphoma are diffuse, occlusive proliferation, especially in the capillaries, small arteries and veins (1). There’s also the involvement of different organs and tissues including the CNS, skin, lung, kidney, but rarely affects the liver, spleen and lymph nodes. The pathogenesis of IVLBCL is unclear, however the splitting and translocation of chromosome maybe related with the pathogenesis of this disease (2).
The clinical manifestations of IVLBCL were nonspecific. Fever, weight loss and sweating (3) were the most common presentations. The main clinical findings were cough, sputum, hypoxaemia and dyspnea when lung was involved. Some patients also presented with hypercalcemia, pulmonary embolism, pulmonary hypertension or hemophagocytic syndrome as initial symptoms (3-5). In this case, pulmonary arterial hypertension was the main presentation with bone marrow hemophagocyte found on histological examination.
An increased serum LDH, CRP and β2-microglobulin interleukin-2R (IL-2R) were found in most cases, and close relation between increased LDH levels and the differentiation of tumor cells was observed, accompanied with anemia, decreased platelets and white blood cell count (6,7). The abnormal lung function usually seen in such cases was limitation of ventilation and diffusion dysfunction (8).
Thoracic computed tomography (CT) findings of the lung involvement of IVLBCL patients were diverse, including ground glass opacity (GGO), multiple centrilobular nodules, interlobular septal thickening, interstitial shadows and thickening of bronchovascular bundles, suggesting lymphatic and or haematological spread (8). Recently, FDG-PET has emerged as a powerful functional imaging tool in the assessment of patients with this type of NHL. Several authors have reported FDG-PET is useful in the diagnosis of IVLBCL when this type of lymphoma is clinically suspected. FDG-PET is a powerful tool for the early diagnosis of IVLBCL with pulmonary involvement, when there is a suspected possibility of the presence of this disease in a patient with respiratory symptoms without abnormal findings by CT (9).
The diagnosis is often delayed due to varied clinical presentations and limited understanding of the entity. Histopathology remains the gold standard for diagnosis, showing the classic appearance of large malignant lymphocytes filling small vascular lumina particularly in cases involving the lung; TBLB was a useful method in our diagnosis. If it cannot be confirmed with TBLB, it is necessary to perform an open lung biopsy or a thoracoscopy (10).
Treatment recommendations are extrapolated from results of trials of more common subtypes of lymphoma. Most cases of IVL are associated with poor prognosis and should be treated systemically with an anthracycline-based regimen. Anthracycline-based chemotherapy has been associated with a 60% response rate and a 3-year overall survival rate of more than 30%. CHOP (cyclophosphamide, doxorubicin, vincristin, prednisone) and CHOP-like regimens are also considered to be effective. The treatment of cases with lung involvement is similar to that of diffuse LBCL. Takahashi et al. (11) found that the effect of rituximab combined with CHOP was better than just the single CHOP regimen, through analysis of the effect on 1,221 cases involving the various organs in patients with LBCL.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Swerdlow SH, Campo E, Harris NL, et al. eds. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue. Geneva: World Health Organization, 2008.
- Cui J, Liu Q, Cheng Y, et al. An intravascular large B-cell lymphoma with a t(3;14)(q27;q32) translocation. J Clin Pathol 2014;67:279-81. [PubMed]
- Sinha N, Lantigua L, Niazi M, et al. An elderly lady with Fever of unknown etiology and severe pulmonary hypertension: intravascular lymphoma-an elusive diagnosis. Case Rep Med 2013;2013:153798.
- Chinen Y, Nakao M, Sugitani-Yamamoto M, et al. Intravascular B-cell lymphoma with hypercalcemia as the initial presentation. Int J Hematol 2011;94:567-70. [PubMed]
- Fung KM, Chakrabarty JH, Kern WF, et al. Intravascular large B-cell lymphoma with hemophagocytic syndrome (Asian variant) in a Caucasian patient. Int J Clin Exp Pathol 2012;5:448-54. [PubMed]
- Anila KR, Nair RA, Koshy SM, et al. Primary intravascular large B-cell lymphoma of pituitary. Indian J Pathol Microbiol 2012;55:549-51. [PubMed]
- Ponzoni M, Ferreri AJ. Intravascular large B cell lymphoma: widespread but not everywhere. Acta Haematol 2014;131:16-7. [PubMed]
- Yu H, Chen G, Zhang R, et al. Primary intravascular large B-cell lymphoma of lung: a report of one case and review. Diagn Pathol 2012;7:70. [PubMed]
- Yamashita H, Suzuki A, Takahashi Y, et al. Intravascular large B-cell lymphoma with diffuse FDG uptake in the lung by 18FDG-PET/CT without chest CT findings. Ann Nucl Med 2012;26:515-21. [PubMed]
- Nishizawa T, Saraya T, Ishii H, et al. Antemortem diagnosis with multiple random skin biopsies and transbronchial lung biopsy in a patient with intravascular large B-cell lymphoma, the so-called Asian variant lymphoma. BMJ Case Rep 2014;2014.
- Takahashi H, Tomita N, Yokoyama M, et al. Prognostic impact of extranodal involvement in diffuse large B-cell lymphoma in the rituximab era. Cancer 2012;118:4166-72. [PubMed]