|
Original Article
Prognostic value of the ratio of ground glass opacity on computed tomography in small lung adenocarcinoma: A meta-analysis
Xiao-Hui Miao1, Yan-Wen Yao1, Dong-Mei Yuan1, Yan-Ling Lv2, Ping Zhan3, Tang-Feng Lv1, Hong-Bing Liu1, Yong Song1
1Department of Respiratory Medicine, Jinling Hospital, Nanjing University School of Medicine, Nanjing 210002, China; 2Department of Respiratory Medicine, Jinling Hospital, Clinical School of Southern Medical University, Nanjing 210002, China; 3First Department of Respiratory Medicine, Nanjing Chest Hospital, Nanjing, 210029, China
Corresponding to: Yong Song, MD, PhD. Department of Respiratory Medicine, Jinling Hospital, Nanjing University School of Medicine, 305 East Zhongshan Road, Nanjing 210002, China. Tel/Fax: +86-25-8086-3591. Email: yong_song6310@yahoo.com.
|
|
Abstract
Introduction: Lung cancer is the leading cause of cancer-associated death. In many countries, adenocarcinoma is the most common histologic type in lung cancer. Previously, few factors are identified to be prognostic indicators for the patients with small lung adenocarcinoma. Recently, the ground glass opacity (GGO) area found on high-resolution computed tomography (HRCT) scanning was identified as a prognostic indicator in some studies. But no clear consensus has been defined.
Methods: The PubMed/MEDLINE, EMBASE, Cochrane library and SpringerLink electronic databases were searched for articles related to ground glass opacity on computed tomography in patients with small lung adenocarcinoma. Data was extracted and analyzed independently by two investigators. An estimate of the hazard ratio (HR) for comparing high GGO ratio with low GGO ratio was extracted. The respective HRs was combined into a pooled HR, and 95% confidence interval (CI) was calculated for each study. The publication heterogeneity was assessed graphically using performing Beggs’ funnel plot. All the statistical tests used in our meta-analysis were performed with STATA version 11.
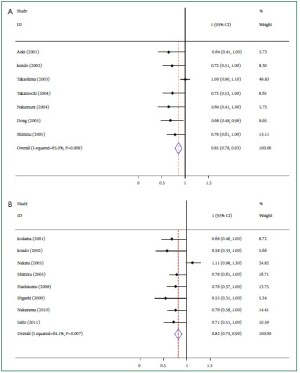
Results: Thirteen studies, encompassing 2,027 patients, were included in our meta-analysis. Ten of these studies revealed that the GGO ratio in small lung adenocarcinoma is a good prognostic indicator. Seven studies were combined in a meta-analysis using overall survival (OS) as the end point of interest. The weighted HR of 7 studies was 0.85, with relative 95% CI ranging from 0.78 to 0.93 (P=0.009). For the surgical patient population, the primary endpoint of relapse-free survival (RFS) was superior with high GGO area on computed tomography (The combined HR 0.82, 95% CI 0.74-0.90; P=0.007).
Conclusions: The result of our meta-analysis suggested that the GGO area measured on HRCT had a prognostic value of overall survival and relapse-free survival in small lung adenocarcinoma. The GGO ratio may be an independent prognostic factor for small lung adenocarcinoma.
Key words
GGO ratio; prognostic factor; small lung adenocarcinoma; meta-analysis
J Thorac Dis 2012;4(3):265-271. DOI: 10.3978/j.issn.2072-1439.2012.05.09 |
|
Introduction
Lung cancer is the leading cause of cancer death in the world and non-small cell lung cancer (NSCLC) is the majority of lung cancer ( 1, 2). The 5-year survival rate of NSCLC is only 10-15% ( 3). Studies have revealed that survival of patients is strongly associated with the stage of lung cancer. Expect stage and performance status, no other prognostic factors have been definitively established for lung cancer. Clinical features including gender, age, weight loss and serum markers have also been studied but are found to be not sufficiently accurate for individual patients. Few indicators are identified to be able to assist in predicting therapy response and outcome ( 4). The detection rate of small lung adenocarcinoma has been increased due to the widely use of high-resolution computed tomography (HRCT) and computed tomography (CT) screening for lung cancer. The small nodules have been identified in clinic as less than 3 cm in diameter and with the ground glass
opacity (GGO) area. Small lung adenocarcinoma could be
classified as either ‘air-containing type’ or ‘solid-density type’
according to tumor shadow disappearance rates (TDR) on
mediastinal window images or GGO ratio ( 5). Air-containing
type is defined as having areas where tumor opacity on
mediastinal window images (TOM) is half or less than half the
size of those noted on lung window images. Solid-density type is
defined as having areas where TOM is greater than half the size
of those noted on lung window images ( 6). Recently, more and more studies indicated that it was important
to identify the characteristics of the GGO lesions on small lung
adenocarcinoma, to determine the appropriate operative mode and
indicate the prognosis for each patient. Some findings indicated
that lung adenocarcinoma patients with air-containing types after
resection demonstrated a better prognosis ( 7). However, some
authors retrospectively analyzed peripheral lung adenocarcinoma
with GGOs and defined the GGO ratio as a limited prognostic
indicator ( 8). A pooled analysis of the current studies might
provide a better understanding of the GGO area in small lung
adenocarcinoma. Therefore, we carried out a systematic review
of published studies and a meta-analysis to combine the results
of these studies. |
|
Materials and methods
Data sources and keywords
PubMed/MEDLINE, EMBASE, Cochrane librar y and
SpringerLink electronic databases were searched with the
keywords ‘ground glass opacity’, ‘small lung adenocarcinoma
prognostic’ and ‘GGO’. Latest studies were updated to May 17th,
2011. Titles and abstracts of research articles were screened
for relevance according to predetermined inclusion criteria.
References of the included studies were also searched to identify
relevant articles that might be missed during the primary search.
Selection criteria
In order to define the eligibility for the meta-analysis, a study
had to meet the following inclusion criteria: (I) high-resolution
CT (HRCT) or thin-slide CT (TSCT) scanned prior to surgery,
(II) limited to small lung adenocarcinoma (less than 3 cm in
diameter), (III) patients underwent pulmonary lobectomy
or segmental resection, (IV) carried out postoperative
histopathological examination, (V) assessed the relationship
between the GGO areas measured on HRCT and patients
survival at least in univariate analysis. The studies have been
published as original articles in English and provided sufficient
data including hazard ratio (HR) and 95% confidence interval
(CI) or survival curve. Meeting proceedings and abstracts were
excluded as it cannot provide enough details to assess patient
survival information to perform the meta-analysis.
When authors reported on the same patient population or
updated data in several publications, only the recent or complete
study was included in the analysis to avoid the overlap of
information.
Data extraction and quality assessment
From the finally included studies, two investigators independently
extracted needed data, such as the first author, the year of
publication, journal name, sex and age of subjects, tumor
histology, retrospective or prospective set-up of the study. The
HR and associated 95% CI were collected from results of the
univariate and multivariate analysis. If the needed data was not
all reported in the texts, published survival curves would be used
to obtain the unreported HR or 95% CI. The survival rates could
also be analyzed from the survival curves; and finally, an adjusted
HR and 95% CI were searched.
Meanwhile, we assessed the quality of included studies
according to the Steele’s methods (European Lung Cancer
Working Party quality scale for biological prognostic factors
for lung cancer) ( 9). The overall score indicated the evaluation
of several dimensions of the methodology, grouped into the
following main categories: The scientific design, the description
of the examinations, the generalizability of the results, the
analysis of the study data and the association between GGO
ratio and patient survival. Each category had a maximum score
of 10 points, in which a value between 0 and 2 was attributed to
each item. Hence the overall maximum score was 40 points. Statistical analysis
We analyzed the survival distributions of high GGO ratio group
and low GGO ratio group to reveal the association between
GGO ratio and survival by hazard ratio (HR). The standard
statistical method is to retrieve the HR estimate and its variance
from the reported results, or to calculate them directly using
parameters given by the authors for the univariate analysis: the
95% CI for the HR, the log-rank statistic, or its p-value. A P value
below 0.05 was considered to be significance.
If the only available data of the survival distributions was in
the form of graphical representations, we extracted data from
the survival curves at different points to reconstruct the HR
estimate and its variance. If survival of three or more groups was
reported, some cutoff value was used to combine these groups
into GGO ratio less than 50% group and greater than 50% group
by reference to the statistical method from Williamson et al. ( 10).
The HR and 95% CI for survival comparison in studies evaluated
the prognostic value of GGO ratio on high-resolution CT. We assessed combined HRs was obtained by the use of fixed effects models in case of absence of heterogeneity and of randomeffects
models otherwise and the publication heterogeneity
between studies by using chi-squared (χ 2) test. Selection bias
was assessed graphically using performing Beggs’ funnel plot.
Interaction tests were performed using χ 2 tests. The χ 2 tests and
I-squared (variation in ES attributable to heterogeneity; I 2)
statistic were used to assess heterogeneity ( 11). An I 2 value greater
than 50% suggested a significant heterogeneity. All statistical
analysis in our meta-analysis was performed using STATA version
11 (StataCorp LP, College Station, Texas 77845, USA). |
|
Results
Eligible studies
Six hundred and eighty-six potentially relevant articles were
found by searching PubMed/MEDLINE, EMBASE, Cochrane
library and SpringerLink electronic databases with the listed
keywords. Studies were included according the inclusion criteria.
Results were also determined by another investigator. Total 15
articles published in March 2001 to May 2011 were enrolled in
the meta-analysis. The final articles for meta-analysis were also
screened to avoid the overlap of patients.
The principal characteristics of the 15 studies for the metaanalysis
are described in Table 1. The association between GGO
ratio and relapse-free survival or overall survival was reported on
each study. Most of the studies identified that high GGO ratio
was associated with a good prognosis. Three studies revealed the
opposite result that high GGO ratio predicted a poor prognosis.
| Table 1. Principal characteristics of 15 studies included in the meta-analysis. |
| Study |
Publication date |
nPts |
GGO ratio |
Computed tomography |
Histology |
Prognosis factor for
survival |
| Takatoshi Aoki et al. (12) |
2001 |
127 |
0.5 |
HRCT |
AC |
favorable |
| Ken Kodama et al. (13) |
2001 |
104 |
0.5 |
HRCT |
AC |
favorable |
| Tetsuro Kondo et al. (6) |
2002 |
137 |
0.5 |
HRCT |
AC |
favorable |
| Boming Dong et al. (14) |
2002 |
143 |
0.5 |
HRCT |
AC |
favorable |
| Shodayu Takashima et al. (15) |
2002 |
64 |
0.57 |
HRCT |
AC |
favorable |
| Shodayu Takashima et al. (16) |
2003 |
52 |
0.5 |
HRCT |
AC |
unfavorable |
| Kazuya Takamochi et al. (17) |
2004 |
189 |
0.8 |
HRCT |
AC |
favorable |
| Haruhiko Nakamura et al. (18) |
2004 |
100 |
0.5 |
HRCT |
AC+SCC |
favorable |
| Masao Nakata et al. (19) |
2005 |
146 |
0.5 |
HRCT |
AC |
unfavorable |
| Boming Dong et al. (20) |
2005 |
131 |
0.5 |
HRCT |
AC |
favorable |
| Kunihiko Shimizu et al. (21) |
2005 |
260 |
0.5 |
HRCT |
AC |
favorable |
| Toshihiko Hashizume et al. (22) |
2008 |
359 |
0.5 |
HRCT |
AC |
favorable |
| Kotaro Higashi et al. (23) |
2009 |
87 |
0.5 |
HRCT |
AC |
favorable |
| Haruhiko Nakayama et al. (24) |
2010 |
201 |
0.5 |
HRCT |
AC |
unfavorable |
| Haruhiro Saito et al. (25) |
2011 |
134 |
0.5 |
TSCT |
AC |
favorable |
| nPts, number of patients; GGO, ground glass opacity; HRCT, high-resolution computed tomography; TSCT, thin-section computed tomography;
AC, adenocarcinoma; SCC, squamous cell carcinoma. |
Consideration of overlaps between patient cohorts
Two studies in 15 publications were reported by Dong B et al.
( 14, 20). The patients from the first study were likely to be
included in the second one. Another two studies were reported
by Takashima S et al. ( 15, 16). Although the overlap was not
large, we included the late studies by Dong B et al. and
Takashima S et al. to avoid the excursion ( 16, 20). Thirteen
studies with total 2,027 patients were finally included in our
meta-analysis ( 6, 12, 13, 16- 25). Quality assessment and evaluable studies
Two independent investigators formally analyzed the quality of
studies referring to the Steele’s methods and variables that might
reflect the quality of studies were recorded. If a variable in a study
was not applicable, this theoretically attributable point would
not be taken into account in the total of the concerned category.
Higher value indicated a better methodological quality. The
final quality scores ranged from 55.0% to 75.5%, with a mean of
68.7%, which indicated that these studies were evaluable and all
publications included into a final meta-analysis.
Survival data aggregation
Thirteen studies with a total number of 2,027 patients were identified and included in the different subgroups analysis from
our previous search. Seven studies were enrolled in a metaanalysis
using overall survival (OS) as the end point of interest.
Table 2 shows the 7 studies included in the meta-analysis with
the GGO ratio for OS analysis. Relapse-free survival (RFS)
data were available in eight studies ( Table 3). We combined the
individual HR into a pooled HR, and 95% confidence interval
(CI) were calculated for every study. Three studies provided
survivals of three or more groups, so these groups were divided
into GGO ratio less than 50% group and greater than 50% group
according to the statistical method from Williamson et al. ( 10).
| Table 2. Meta-analysis of GGO ratio for overall survival analysis on small lung carcinoma. |
| Study |
Publication date |
nPts |
HR |
95% CI |
| Takatoshi Aoki et al. (12) |
2001 |
127 |
0.64 |
0.41-1.00 |
| Tetsuro Kondo et al. (6) |
2002 |
52 |
0.72 |
0.51-1.00 |
| Shodayu Takashima et al. (15) |
2003 |
52 |
0.10 |
0.90-1.10 |
| Kazuya Takamochi et al. (17) |
2004 |
189 |
0.72 |
0.52-1.00 |
| Haruhiko Nakamura et al. (18) |
2004 |
100 |
0.64 |
0.41-1.00 |
| Boming Dong et al. (20) |
2005 |
131 |
0.68 |
0.48-0.96 |
| Kunihiko Shimizu et al. (21) |
2005 |
260 |
0.78 |
0.61-1.00 |
| nPts, number of patients; HR, hazard ratio; CI, confidence interval. |
| Table 3. Meta-analysis of GGO ratio for relapse-free survival analysis on small lung carcinoma. |
| Study |
Publication date |
nPts |
HR |
95% CI |
| Ken Kodama et al. (13) |
2001 |
104 |
0.68 |
0.46-1.00 |
| Tetsuro Kondo et al. (6) |
2002 |
137 |
0.58 |
0.33-1.00 |
| Masao Nakata et al. (19) |
2005 |
146 |
1.11 |
0.98-1.30 |
| Kunihiko Shimizu et al. (21) |
2005 |
260 |
0.78 |
0.61-1.00 |
| Toshihiko Hashizume et al. (22) |
2008 |
359 |
0.76 |
0.57-1.00 |
| Kotaro Higashi et al. (23) |
2009 |
87 |
0.55 |
0.57-1.00 |
| Haruhiko Nakayama et al. (24) |
2010 |
201 |
0.76 |
0.58-1.00 |
| Haruhiro Saito et al. (25) |
2011 |
134 |
0.71 |
0.51-1.00 |
| nPts, number of patients; HR, hazard ratio; CI, confidence interval. |
The final HR revealed a survival benefit of high GGO ratio for
small lung adenocarcinoma. The square size is proportional to
the number of patients included in the study. The weighted HR
of 7 studies at overall survival was 0.85, with a 95% confidence
interval ranging from 0.78 to 0.93 (P=0.009) ( Figure 1A). The
total of patients in 8 studies on relapse-free survival was 1,428.
As shown in Figure 1B, relapse-free survival did significantly
differ between the two groups (The weighted HR 0.82, 95% CI
0.74-0.90; P=0.007). Heterogeneity study
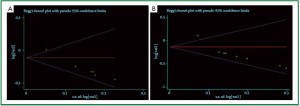
The funnel plot for the 7 reports on overall survival analysis
revealed an evidence of publication bias ( Figure 2A).
Heterogeneity χ 2 =17.15 (degrees of freedom, df.=6; P=0.009).
I 2=65.0%. As showed in Figure 2B, the funnel plot for the studies
on relapse-free survival analysis also showed the publication
bias. Heterogeneity χ 2=19.52 (df.=7; P=0.007). Again high
inconsistency was found across studies (I 2 statistics =64.1%). |
|
Discussion
We confirmed in our meta-analysis, with 13 original studies and
2,027 patients, that the GGO ratio was a prognostic indicator
for small lung adenocarcinoma. After combined the HR from
different studies, the final result suggested that high GGO ratio
in HRCT predicted a better OS and RFS with a significant
statistical value.
Recently, high-resolution computed tomography (HRCT)
scan for lung cancer mass has been reported to have an advantage
at defining tumors as small as 3 cm in diameter or less. The
optimal intervention of these patients can improve the lung
cancer survival rate and diminish the mortality.
Previously, pathological type and lymph node status were
considered to be the most significant prognostic factors ( 26),
and some prognostic factors have been reported for patients
with surgically resected small lung adenocarcinoma. Most adenocarcinomas with a good prognosis showed in the
radiography as pure GGO or GGO mixed with a small area of
solid attenuation at high-resolution CT ( 27). Several studies have
reported that the ground glass opacity (GGO) at HRCT finally
proved to be lung adenocarcinomas in pathology ( 28). This
showed a significant association between the GGO and tumor
pathological type. However, the association between GGO ratio
in HRCT and survival of small lung carcinoma patients was not
identified. The GGO ratio and TDR possibly reflected grade of tumor malignancy. A tumor with a larger GGO component
is likely to be adenocarcinoma in situ or minimally invasive
adenocarcinoma, therefore to have low propensity for distant
spread. The lung adenocarcinoma smaller than 3 cm with
a GGO component of more than 50% at HRCT has a high
likelihood of being free of lymph node metastasis or vein
involvement. Although lobectomy with mediastinal lymph node
dissection is a standard operative procedure for lung cancer,
the small adenocarcinoma with more GGO might be managed
appropriately by limited resection to decreasing the operative
mortality and morbidity as well as improving the performance
status of the patients ( 29). Our meta-analysis still has several limitations. First, publication
bias is a well known problem in meta-analysis. Although we tried
to reduce the selection bias to small, this meta-analysis still had
a selection bias. This result was expected because the included
patients of most studies came from Asia. Therefore, the studies
have been published in the English language, which might have
induced a verification bias. In our meta-analysis, we included
13 articles in which 12 articles had a GGO ratio of 0.5, only
one reported as TDR of 0.8. The proportion of 24 patients with
squamous cell cancer histology only reported by Nakamura H
et al. was small. Second, since the GGO component has been
calculated by using a semi-quantitative method with physician
determination, the GGO areas on HRCT or TSCT scanning
would be reported with disparity.
Although with these limitations, our meta-analysis still
provide a positive and statistically significant result that high
GGO ratio in HRCT predicted a better OS and RFS for small
lung adenocarcinoma patients. |
|
Conclusions
Our meta-analysis indicated that the GGO ratio had a prognostic
value for small lung adenocarcinoma. The GGO ratio on HRCT
scan could be an important predictive factor for postsurgical
survival in patients with small lung adenocarcinoma. This result
revealed the predictive value of GGO ratio for clinic. To further
confirm these findings, large, prospective, randomized studies
are required. |
|
Acknowledgements
This research was supported by the Natural Science Fund of
Jiangsu Province (BK2011658) to Yong Song.
Disclosure: The authors declare no conflict of interest.
|
|
References
- Jemal A, Center MM, Desantis C, et al. Global patterns of cancer incidence
and mortality rates and trends. Cancer Epidemiol Biomarkers Prev
2010;19:1893-907.
- Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin
2010;60:277-300.
- Molina JR, Yang P, Cassivi SD, et al. Non-small cell lung cancer:
epidemiology, risk factors, treatment and survivorship. Mayo Clin Proc
2008;83:584-94.
- Sculier JP, Chansky K, Crowley JJ, et al. The impact of additional
prognostic factors on survival and their relationship with the anatomical
extent of disease expressed by the 6th Edition of the TNM Classification of
Malignant Tumors and the proposals for the 7th Edition. J Thorac Oncol
2008;3:457-66.
- Hasegawa M, Sone S, Takashima S, et al. Growth rate of small lung cancers
detected on mass CT screening. Br J Radiol 2000;73:1252-9.
- Kondo T, Yamada K, Noda K, et al. Radiologic-prognostic correlation in
patients with small pulmonary adenocarcinomas. Lung Cancer 2002;36:49-57.
- Ichiki Y, Hanagiri T, Baba T, et al. Limited pulmonary resection for peripheral
small-sized adenocarcinoma of the lung. Int J Surg 2011;9:155-9.
- Lee HY, Han J, Lee KS, et al. Lung adenocarcinoma as a solitary pulmonary
nodule: Prognostic determinants of CT, PET, and histopathologic findings.
Lung Cancer 2009;66:379-85.
- Steels E, Paesmans M, Berghmans T, et al. Role of p53 as a prognostic
factor for survival in lung cancer: a systematic review of the literature with a
meta-analysis. Eur Respir J 2001;18:705-19.
- Williamson PR, Smith CT, Hutton JL, et al. Aggregate data meta-analysis
with time-to-event outcomes. Stat Med 2002;21:3337-51.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis.
Stat Med 2002;21:1539-58.
- Aoki T, Tomoda Y, Watanabe H, et al. Peripheral lung adenocarcinoma:
correlation of thin-section CT findings with histologic prognostic factors
and survival. Radiology 2001;220:803-9.
- Kodama K, Higashiyama M, Yokouchi H, et al. Prognostic value of groundglass
opacity found in small lung adenocarcinoma on high-resolution CT
scanning. Lung Cancer 2001;33:17-25.
- Dong B, Sato M, Sagawa M, et al. Computed tomographic image
comparison between mediastinal and lung windows provides
possible prognostic information in patients with small peripheral lung
adenocarcinoma. J Thorac Cardiovasc Surg 2002;124:1014-20.
- Takashima S, Maruyama Y, Hasegawa M, et al. Prognostic significance of
high-resolution CT findings in small peripheral adenocarcinoma of the
lung: a retrospective study on 64 patients. Lung Cancer 2002;36:289-95.
- Takashima S, Maruyama Y, Hasegawa M, et al. High-resolution CT
features: prognostic significance in peripheral lung adenocarcinoma with
bronchioloalveolar carcinoma components. Respiration 2003;70:36-42.
- Takamochi K, Yoshida J, Nishimura M, et al. Prognosis and histologic
features of small pulmonar y adenocarcinoma based on serum
carcinoembryonic antigen level and computed tomographic findings. Eur J
Cardiothorac Surg 2004;25:877-83.
- Nakamura H, Saji H, Ogata A, et al. Lung cancer patients showing pure
ground-glass opacity on computed tomography are good candidates for
wedge resection. Lung Cancer 2004;44:61-8.
- Nakata M, Sawada S, Yamashita M, et al. Objective radiologic analysis of
ground-glass opacity aimed at curative limited resection for small peripheral
non-small cell lung cancer. J Thorac Cardiovasc Surg 2005;129:1226-31.
- Dong B, Sato M, Sakurada A, et al. Computed tomographic images reflect
the biologic behavior of small lung adenocarcinoma: they correlate
with cell proliferation, microvascularization, cell adhesion, degradation
of extracellular matrix, and K-ras mutation. J Thorac Cardiovasc Surg
2005;130:733-9.
- Shimizu K, Yamada K, Saito H, et al. Surgically curable peripheral lung
carcinoma: correlation of thin-section CT findings with histologic
prognostic factors and survival. Chest 2005;127:871-8.
- Hashizume T, Yamada K, Okamoto N, et al. Prognostic significance of
thin-section CT scan findings in small-sized lung adenocarcinoma. Chest
2008;133:441-7.
- Higashi K, Sakuma T, Ito K, et al. Combined evaluation of preoperative
FDG uptake on PET, ground-glass opacity area on CT, and serum CEA
level: identification of both low and high risk of recurrence in patients
with resected T1 lung adenocarcinoma. Eur J Nucl Med Mol Imaging
2009;36:373-81.
- Nakayama H, Okumura S, Daisaki H, et al. Value of integrated positron
emission tomography revised using a phantom study to evaluate
malignancy grade of lung adenocarcinoma: a multicenter study. Cancer
2010;116:3170-7.
- Saito H, Kameda Y, Masui K, et al. Correlations between thin-section
CT findings, histopathological and clinical findings of small pulmonary
adenocarcinomas. Lung Cancer 2011;71:137-43.
- Anami Y, Iijima T, Suzuki K, et al. Bronchioloalveolar carcinoma (lepidic
growth) component is a more useful prognostic factor than lymph node
metastasis. J Thorac Oncol 2009;4:951-8.
- Noguchi M, Morikawa A, Kawasaki M, et al. Small adenocarcinoma of the
lung. Histologic characteristics and prognosis. Cancer 1995;75:2844-52.
- Kondo T, Yamada K, Noda K, et al. Radiologic-prognostic correlation in
patients with small pulmonary adenocarcinomas. Lung Cancer 2002;36:49-57.
- Schuchert MJ, Pettiford BL, Keeley S, et al. Anatomic segmentectomy
in the treatment of stage I non-small cell lung cancer. Ann Thorac Surg
2007;84:926-32; discussion 932-3.
Cite this article as: Miao XH, Yao YW, Yuan DM, Lv YL, Zhan P, Lv TF,
Liu HB, Song Y. Prognostic value of the ratio of ground glass opacity on
computed tomography in small lung adenocarcinoma: A meta-analysis. J
Thorac Dis 2012;4(3):265-271. doi: 10.3978/j.issn.2072-1439.2012.05.09
|