Tracheal nodular lymphoid hyperplasia presenting dyspnea and obstructive sleep apnea
Nodular lymphoid hyperplasia (NLH) is a rare lymphoproliferative disorder, it so far has not been reported to involve the trachea (1). We recently came across a case of an adolescent female who presented with signs and symptoms of progressive airway obstruction and was initially diagnosed with obstructive sleep apnea (OSA). She was subsequently found to have an obstructing mass of the trachea and pathologic evaluation to be NLH. Exempt status was granted by the Guangzhou Medical University.
A previously healthy 12-year-old girl complained of difficulty breathing after minor activities (such as walking upstairs) and snoring over the past 2 months. She had been treated as asthma but with no improvement. Methacholine challenge was negative, but her pulmonary function test revealed flow-volume curves with plateauing in both the inspiratory and expiratory limbs, suggesting an airflow limitation caused by intrathoracic airway obstruction. Her symptoms worsened, and she developed wheezing and stridor during exertion, showing fluttering of the chest while lying on her back. Polysomnography (PSG) showed severe OSA with an apnea hypopnea index of 33/h, and oxygen desaturation down to 81%. The patient was then transferred to ENT department for treatment of OSA.
Her body mass index was 16 kg/m2, tonsils in the tonsillar pillar, and the residual adenoids not enlarged (Figure 1). Video laryngoscopy was performed by a pediatric otolaryngologist on the first day of admission and showed an intraluminal polypoid lesion originating inside from the right of the 1st tracheal cartilaginous ring, which almost completely occluded the proximal trachea in a ball-valve fashion along with her breathing (Figure 1A,B). The tracheal mass was removed by flexible bronchoscopy under general anesthesia with spontaneous respiration, her dyspnea and snoring disappeared since the first night following surgery. Pathologic study of the mass indicated NLH (Figure 2).
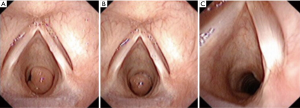
The flow–volume loop was normal, PSG performed at 3 months postoperatively indicated that her condition had improved, with an AHI of 0.9/h and oxygenation around 93%. At the time of writing, the patient had been symptom-free for 21 months with no additional treatment (Figure 1C).
The symptoms of primary tracheal tumors are largely dyspnea, coughing, wheezing, haemoptysis or obstructive pneumonia (2). Dyspnea can readily masquerade as onset asthma and evade timely diagnosis. In present case, the trachea tumor was observed without a hitch by an otolaryngologist, it must emphasize the fact that endoscopy is not only the gold standard but also the first choice in evaluation of the upper airway in children (3).
It was certain that the symptom of difficulty in breathing was disappeared after removal of the tracheal mass. To our surprise, OSA was cured only by removal of the tracheal obstruction in this case, indicating that the trachea alone was the site of obstruction. As we know, the development of OSA in children has been linked to a variety of predisposing factors, including obesity, nasal obstruction, adenoidal and/or tonsillar hypertrophy, craniofacial anomalies, and neuromuscular disorders, but all those factors were not found in present case. In literature, OSA developed after tracheal occlusion is shown only in canine experiments (4). However, those authors acknowledged a critical limitation in animal models—bypassing of the upper airways—which is of major importance in the development of human OSA (4). It is noteworthy that human OSA resulting from tracheomalacia alone (causing tracheal airflow limitation), without accompanying pharyngeal or laryngeal obstruction, has ever been reported (5). This case adds to the literature by showing that OSA (or snoring) may also be a symptom of tracheal tumor.
Tracheal lumen has a large functional reserve and tumors do not cause symptoms until they occlude 50–75% of the luminal diameter. Exertional dyspnoea will not develop until the trachea has narrowed to less than 8 mm, and once the lumen is less than 5 mm, dyspnoea will also occur at rest (3). The factors, including the site, the degrees, and the time of tracheal obstruction take place, which leads to the occurrence of OSA, need further study.
This case is “seemingly straightforward” and the management goes smoothly. Would this patient have consulted a bronchoscopist, but not a physician of otolaryngology-head and neck surgery, this case could have been one of the unremarkable medical practicing in China and have not prompted for our reflection, because her symptom of difficulty breathing resolved after removal of the tracheal mass. However, in the perspective of an otolaryngologist, it should be surprising to note that her OSA was cured simply by removal of the tracheal obstruction, which indicates that the trachea can be the sole site of airway obstruction in certain OSA patients. We have encountered with cases of tracheal neoplasms in the clinic, but never performed PSG for those patients. The present case implied a probable novel and unusual instance of pathophysiological mechanism showing that OSA may arise simply from a tracheal obstruction. The elucidation of the relationship between tracheal obstruction and OSA required accumulative analysis of more cases.
Acknowledgements
The authors are grateful to Prof. Yingying Gu for her pathological diagnosis and to Dr. Guangqiao Zeng for his critique of the manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hare SS, Souza CA, Bain G, et al. The radiological spectrum of pulmonary lymphoproliferative disease. Br J Radiol 2012;85:848-64. [Crossref] [PubMed]
- Wood RE. Evaluation of the upper airway in children. Curr Opin Pediatr 2008;20:266-71. [Crossref] [PubMed]
- Macchiarini P. Primary tracheal tumours. Lancet Oncol 2006;7:83-91. [Crossref] [PubMed]
- Muzumdar H, Nandalike K, Bent J, et al. Obstructive sleep apnea due to extrathoracic tracheomalacia. J Clin Sleep Med 2013;9:163-4. [PubMed]
- Kimoff RJ, Makino H, Horner RL, et al. Canine model of obstructive sleep apnea: model description and preliminary application. J Appl Physiol (1985) 1994;76:1810-7. [PubMed]



