
A stitch in time: age impacts survival in repair of atrioventricular septal defects
In recent years, survival for children with the spectrum of atrioventricular septal defects (AVSDs) has improved markedly (1-4). However, long-term function of the left atrioventricular valve (LAVV) remains the Achilles’ heel of AVSDs, with reoperation rates of approximately 10–20% at 20-year (1-3,5,6). Furthermore, there is ongoing debate regarding the optimal approach to children who present with heart failure under 3 months of age, namely whether to opt for primary complete repair or pulmonary artery banding (7-9).
Cai et al. (10) report their experience with 150 patients across the spectrum of AVSD who underwent complete repair at Fudan University between 2013 and 2021. They observed an early mortality of 10% in the complete AVSD group, 1.8% in the partial AVSD group and 0% in the transitional AVSD group. Moreover, they observed 80% freedom from LAVV regurgitation in the complete AVSD group at 5 years.
The early mortality of 1.8% for partial and 0% for transitional AVSD is in keeping with recent large studies which report an early mortality around 1% for this group (1,4). On initial reading, an early mortality of 10% for complete AVSD appears to be somewhat higher than the expected range of 1–3% (2,3,5,11) in the recent era. However, a deeper analysis reveals that there was a very high rate of preoperative moderate or greater LAVV regurgitation and pulmonary hypertension, which were two of the major factors associated with mortality. Moderate or greater LAVV regurgitation was present in 76.1% of patients with complete AVSD in this study (10), compared to 20% of our patients in Melbourne (2) and 30% in Texas (4). Both LAVV regurgitation and pulmonary hypertension were particularly common in patients under 3 months of age, who were also at increased risk of mortality. Additionally, Cai et al. demonstrated a bimodal distribution of pulmonary hypertensive crisis and mortality, most commonly occurring under 6 months of age and beyond 12 months of age. Together these suggest that the group from Fudan were dealing with a higher risk group of patients. It is always difficult to speculate why regional differences exist in the presentation of patients, but explanations could include lower rates of prenatal and neonatal detection, resulting in later referral, as well as preferential referral of those with severe symptoms, and decreased access to optimal medical management. Indeed, our anecdotal experience with the rare patients who present for complete AVSD repair beyond 1 year of age suggests the perioperative course is much more complicated.
Most centres today prefer to electively repair complete AVSD between 3 and 6 months, to prevent secondary changes in the LAVV and the onset of irreversible pulmonary vascular changes. It appears that a proportion of the patients in Cai et al.’s study missed out on this window of opportunity, having surgery after 9 months of age, and these patients appear to be at increased risk of pulmonary hypertensive crisis.
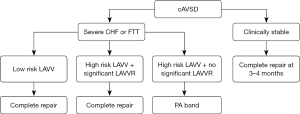
At the other end of the age spectrum, patients under 3 months of age were also at elevated risk. In this age group there is equipoise regarding surgical strategy: early complete repair or pulmonary artery banding. We have previously demonstrated that pulmonary artery banding is associated with a significant risk of mortality while awaiting complete repair (8). Thus we, and other groups (5), favour the approach taken by Cai et al. of early complete repair in patients who have heart failure despite maximum medical therapy. In the majority of these patients there is significant LAVV regurgitation contributing to heart failure, and in these patients achieving a balanced circulation without exacerbating LAVV regurgitation is challenging. Furthermore, we have not observed an increase in the rate of LAVV reoperation with early repair, even in those under 3.5 kg (12). Our proposed algorithm for choosing between complete repair and pulmonary artery banding is demonstrated in Figure 1. We prefer primary complete repair in the majority of cases, apart from those who do not have significant LAVV regurgitation and exhibit high risk features for post-operative LAVV regurgitation (e.g., non-syndromic, single papillary muscle, deficient mural leaflet), where pulmonary artery banding may be preferred. In these young patients the LAVV is fragile and must be treated with the greatest respect, for this reason we prefer a two-patch approach to decrease the risk of distortion of the bridging leaflets as much as possible.
The report by Cai et al. is a timely reminder of the challenges associated with pulmonary hypertension and LAVV regurgitation in patients with complete AVSD. They should be congratulated for achieving such respectable results in a high-risk group of patients. The lesson from this study is that patients with complete AVSD should be closely followed by cardiologists, provided with optimal medical therapy at the onset of heart failure, and undergo complete electively around 3 months of age or earlier if heart failure cannot be controlled. A proactive approach may help reduce the risk of surgery for AVSD.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Thoracic Disease. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1664/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Buratto E, McCrossan B, Galati JC, et al. Repair of partial atrioventricular septal defect: a 37-year experience. Eur J Cardiothorac Surg 2015;47:796-802. [Crossref] [PubMed]
- Buratto E, Lui A, Hu T, et al. Propensity Score Matched Analysis of Cleft Closure in Complete Atrioventricular Septal Defect Repair. Ann Thorac Surg 2022;113:1553-61. [Crossref] [PubMed]
- Mery CM, Zea-Vera R, Chacon-Portillo MA, et al. Contemporary Outcomes After Repair of Isolated and Complex Complete Atrioventricular Septal Defect. Ann Thorac Surg 2018;106:1429-37. [Crossref] [PubMed]
- Mery CM, Zea-Vera R, Chacon-Portillo MA, et al. Contemporary results after repair of partial and transitional atrioventricular septal defects. J Thorac Cardiovasc Surg 2019;157:1117-1127.e4. [Crossref] [PubMed]
- Ramgren JJ, Nozohoor S, Zindovic I, et al. Long-term outcome after early repair of complete atrioventricular septal defect in young infants. J Thorac Cardiovasc Surg 2021;161:2145-53. [Crossref] [PubMed]
- Buratto E, Ye XT, Bullock A, et al. Long-term outcomes of reoperations following repair of partial atrioventricular septal defect. Eur J Cardiothorac Surg 2016;50:293-7. [Crossref] [PubMed]
- Devlin PJ, Jegatheeswaran A, McCrindle BW, et al. Pulmonary artery banding in complete atrioventricular septal defect. J Thorac Cardiovasc Surg 2020;159:1493-1503.e3. [Crossref] [PubMed]
- Buratto E, Hu T, Lui A, et al. Early repair of complete atrioventricular septal defect has better survival than staged repair after pulmonary artery banding: A propensity score-matched study. J Thorac Cardiovasc Surg 2021;161:1594-601. [Crossref] [PubMed]
- Buratto E, Khoo B, Ye XT, et al. Long-Term Outcome After Pulmonary Artery Banding in Children With Atrioventricular Septal Defects. Ann Thorac Surg 2018;106:138-44. [Crossref] [PubMed]
- Cai Y, Chen R, Chen G, et al. Middle to long-term outcomes of surgical repair for atrioventricular septal defect: a single-center study. J Thorac Dis 2022;14:3706-18. [Crossref] [PubMed]
- St Louis JD, Jodhka U, Jacobs JP, et al. Contemporary outcomes of complete atrioventricular septal defect repair: analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. J Thorac Cardiovasc Surg 2014;148:2526-31. [Crossref] [PubMed]
- Goutallier CS, Buratto E, Schulz A, et al. Repair of complete atrioventricular septal defect between 2 and 3.5 kilograms: Defining the limits of safe repair. J Thorac Cardiovasc Surg 2022;164:1167-75. [Crossref] [PubMed]


