Incidence and diagnostic validity of difficult airway in emergency departments in China: a cross-sectional survey
Highlight box
Key findings
• We found a high incidence of difficult bag-valve mask ventilations but relatively low rates of difficult intubations in emergency departments in China.
• Assessments for difficult airways applied to the Chinese population but had improvement space.
What is known and what is new?
• There is no standard difficult airway evaluation in emergency departments.
• We provided the validity of difficult airway assessments in emergency departments in China.
What is the implication, and what should change now?
• Continuous attention to the difficult airway problems and optimizing airway assessment are required.
Introduction
Difficult airways are a challenge for those who perform endotracheal intubations. The incidence of the difficult airway is lower in surgical patients (1) but is higher in non-preoperative (e.g., emergency department, ED) patients. The consequences of the worst-case difficult airway, the “cannot intubate and cannot ventilate” situation, can be catastrophic (2). Understanding and anticipating the difficult airway is of paramount importance for intubators, including emergency medicine physicians. However, the incidence of difficult airways in EDs in China is still unknown.
Airway assessment before intubation is recommended in multiple difficult airway management guidelines (3) and may allow those intubating to prepare sufficient devices, staff, and contingent strategies prior to induction. Nevertheless, inconsistent evaluation methods are often utilized with relatively low accuracy (4). Furthermore, most previous studies were performed on surgical patients, not patients admitted to EDs (5). Fast and concise physical examinations to detect a difficult airway that are widely used in Chinese EDs include neck mobility limitation, airway stenosis, outlook, and the “3-3-2” evaluation. However, their diagnostic value(s) are still unknown.
This study aimed to identify the incidence of difficult airways in mainland Chinese EDs, as well as the diagnostic validity of the commonly used physical examination techniques. Understanding the incidence of difficult airways can help identify problems in difficult airway management and provide directions for follow-up research. While the assessment of a difficult airway is an important step in determining pre-intubation preparation and intubation procedures. The second purpose of this study was to explore the applicability of evaluation methods commonly used in the domestic emergency department for emergency intubation patients.
We hypothesized that the incidences of difficult airways in emergency departments in China were high. The commonly used methods to predict difficult airways may apply to domestic. We present the following article in accordance with the STARD reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-199/rc).
Methods
This study recruited a total of 41 tertiary hospitals from 19 provinces in all seven geographical regions of the country. These hospitals are general hospitals and treat all types of emergency patients. Emergency physicians at participating hospitals were able to perform intubation independently. It utilized a multicentral questionnaire conducted in mainland China from March 1, 2021, to March 31, 2021. Electronic questionnaires were designed on the REDCap (Research Electronic Data Capture) platform (6) and were issued after online group training on March 1st (questionnaire in the Appendix 1). This study was registered with the Chinese Clinical Trials Registry (ChiCTR2100043745) and was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Peking Union Medical College Hospital (No. JS-2718), and informed consent was taken from all the patients.
Adult patients intubated in the emergency departments during the research period were screened for inclusion in this study. Patients with important information missing, data entry mistakes, or intubated outside the ED were excluded. Investigators recorded information in the survey instrument and did not intervene in the clinical treatment process. Double-check was performed by the person in charge of each hospital and the general investigator to mitigate the bias.
The difficult airway is a broad concept (7), which includes difficult face mask ventilation, glottic exposure, tracheal intubation, or difficult front of neck access. This paper only focused on difficult airway patients under non-invasive management. Difficult face mask ventilation is defined as the inability to ventilate with a face mask by one operator (i.e., needing two physicians or a change in ventilation techniques). Glottic exposure is a traditional prerequisite for tracheal intubation, and its classification under direct laryngoscopy can be divided into four grades. Grades III and IV (unable to see the glottic opening) imply difficulty (8). However, the recent guideline did not emphasize the equipment used for evaluation (3). As for the difficult tracheal intubation, the widely accepted definition is a failed intubation after multiple attempts. To quantify the criteria, we defined it as requiring more than two attempts (9). Elective perioperative case with proper planning and airway preparedness versus emergent airway for an emergency department admission with borderline physiology. Authors defined difficult intubation as those needing more than two attempts, which may be suitable for the study but a little too generous to be labeled for difficult intubation.
The primary outcome was the incidence of difficult airways, including the difficult face mask ventilation, laryngoscope exposure, and intubation. Secondary outcomes were the sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio of commonly used airway evaluation methods in China related to the latter two difficult airway situations.
We collected patient characteristics, including sex, age, intubation indications, the names of physicians’ affiliated departments, physicians’ past intubation experience, selected intubation equipment, and intubation context (whether it was emergent or not). The primary variable was the incidence of difficult airways. The secondary variables, including four physical examinations, were performed at the time of intubation [neck mobility, airway stenosis, facial appearance, and the “3-3-2” evaluation (mouth opening greater than three fingers, chin to mandibular hyoid bone more than three fingers, and mandibular hyoid bone to superior thyroid fossa more than two fingers)], and patients were divided into two categories based on the ease of the intubation process. To facilitate the evaluation process, we provided graphic illustrations in the questionnaire regarding the four examinations.
Most junior staff performed the intubation with video laryngoscopy in emergency departments in China. Preoxygenation was carried on in non-crash situations, and bag and mask ventilation was the most commonly used technique for preoxygenation patients before intubation.
This is a supplementary analysis of another study on Tracheal Intubation in Emergency Departments in China (10). Its size calculation is based on the 12% adverse event for intubation, allowable error of 2%, α=0.05, 1−β=0.8, two-tailed test. 1,063 subjects are required for the study.
Statistical analysis
SPSS version 27 (IBM Corp., Armonk, New York, USA) was used to collate and analyze the data. Categorical variables were presented as frequencies with percentages. Values and 95% confidence intervals (CI) for sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were calculated. The probability of diagnosis was calculated and illustrated as ROC (receiver operator characteristic) curves. The AUC (area under the curve) and P values were analyzed to evaluate diagnostic validity.
Results
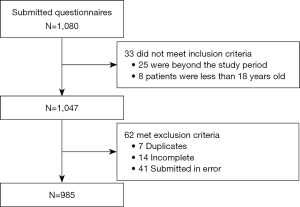
We received a total of 1,080 surveys during the investigation period. Nine hundred and eighty-five left after screening for eligibility criteria, duplicates, incompletes, and errors in submission (Figure 1).
Six hundred and sixty-three (67.3%) of 985 patients intubated in March were male. Elderly patients aged 60 to 80 years old accounted for 46.2% (455 of 985) of all cases. Intubation indications varied. The most common reasons were central nervous system diseases in 349 cases (35.4%), followed by cardiopulmonary arrest in 242 (24.6%), respiratory diseases in 204 (20.7%), and circulatory failure in 185 (18.8%). Emergency medicine physicians conducted most ED intubations 919 (93.3%). 766 patients (77.8%) were intubated immediately upon arriving at the ED (Table 1).
Table 1
| Characteristic | N (%) |
|---|---|
| Sex | |
| Male | 663 (67.3) |
| Age, years | |
| 18–40 | 82 (8.3) |
| 40–60 | 296 (30.1) |
| 60–80 | 455 (46.2) |
| 80–100 | 152 (15.4) |
| Cause | |
| Respiratory failure | 204 (20.7) |
| Circulatory failure | 185 (18.8) |
| CNS disease | 349 (35.4) |
| Cardiopulmonary arrest | 242 (24.6) |
| Others | 5 (0.5) |
| Intubation department | |
| Emergency department | 919 (93.3%) |
| Anesthesiology department | 66 (6.7%) |
| Intubation experience | |
| >50 | 637 (64.7) |
| 30–50 | 144 (14.6) |
| 10–30 | 147 (14.9) |
| <10 | 57 (5.8) |
| Emergency intubation | 766 (77.8) |
CNS, central nervous system.
Airway opening maneuvers
Opening the airway is the first step in airway management. However, 36 (3.7%) patients missed this step. Eight hundred and thirty-four (84.7%) and 149 (15.1%) of the patients had chin tilt or jaw thrust maneuvers performed, respectively. Oropharyngeal airways were inserted in 225 (22.8%).
Difficulty in bag-valve mask ventilation
Five hundred and thirty-four (54.2%) patients underwent bag-valve mask ventilation before the intubation. Among them, 44 (8.2%) patients had difficulty ventilating with a bag-valve masks.
Difficulty in glottic exposure
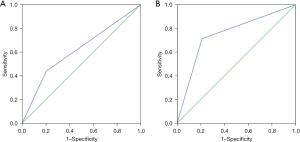
The incidence of difficult glottic exposure was 6.9% (68 of 985). In addition, we utilized several kinds of simple examination methods (neck mobility, narrow oral opening, “3-3-2” evaluation, external look) to predict the possibility of difficulty. Among all four tests, any one of them showed low sensitivity and relatively high specificity (see Table 2). We then combined all four tests and considered the combined test positive for a likely difficult airway if one or more of the four component tests was positive. The combined test had a sensitivity of 0.44 (95% CI: 0.32–0.57), specificity of 0.79 (95% CI: 0.77–0.82), LR+ (positive likelihood rate) of 2.2 (95% CI: 1.6–2.9), and LR− (negative likelihood rate) of 0.70 (95% CI: 0.57–0.87) (see Table 2). In addition, the AUC was 0.62 (95% CI: 0.54–0.69) and P<0.01 (see Figure 2A).
Table 2
| Physical examination | TP | TN | FP | FN | Sensitivity (95% CI) | Specificity (95% CI) | LR+ (95% CI) | LR− (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Neck mobility limitation | 11 | 877 | 40 | 57 | 0.16 (0.09–0.28) | 0.96 (0.94–0.97) | 3.7 (2.0–6.9) | 0.88 (0.79–0.97) |
| Airway stenosis | 9 | 888 | 29 | 59 | 0.13 (0.07–0.24) | 0.97 (0.95–0.98) | 4.2 (2.1–8.5) | 0.90 (0.82–0.98) |
| Outlook | 9 | 853 | 64 | 59 | 0.13 (0.07–0.24) | 0.93 (0.91–0.95) | 1.9 (1.0–3.6) | 0.93 (0.85–1.02) |
| 3-3-2 evaluation | 17 | 804 | 113 | 51 | 0.25 (0.16–0.37) | 0.87 (0.85–0.90) | 2.0 (1.3–3.2) | 0.86 (0.75–0.98) |
| Any one of the above positive | 30 | 729 | 188 | 38 | 0.44 (0.32–0.57) | 0.79 (0.77–0.82) | 2.2 (1.6–2.9) | 0.70 (0.57–0.87) |
TP, true positive; TN, true negative; FP, false positive; FN, false negative; CI, confidence interval; LR+, positive likelihood rate; LR−, negative likelihood rate.
Given that different intubation devices may cause different ease of arriving at a satisfactory glottic exposure, we divided patients into two groups: those who underwent video laryngoscopy vs. those who received traditional direct laryngoscopy. The related parameters between the two groups were a sensitivity of 0.48 vs. 0.38, specificity of 0.81 vs. 0.74, AUC of 0.64 vs. 0.56 and a P value <0.01 vs. 0.37, respectively (see Table 3).
Table 3
| Validity | Video laryngoscopy group | Direct laryngoscopy group |
|---|---|---|
| Sensitivity | 0.48 (0.33–0.63) | 0.38 (0.19–0.61) |
| Specificity | 0.81 (0.78–0.83) | 0.74 (0.66–0.80) |
| LR+ | 2.5 (1.8–3.5) | 1.5 (0.8–2.7) |
| LR− | 0.65 (0.49–0.85) | 0.84 (0.60–1.18) |
| AUC | 0.64 | 0.56 |
LR+, positive likelihood rate; LR−, negative likelihood rate; AUC, area under the curve.
Difficult intubation
This trial found 21 (2.1%) patients who had difficult ED intubations. The prognostic value of the four physical examination maneuvers were like the findings for glottic exposure. The combined test had a sensitivity of 0.71 (95% CI: 0.47–0.89), a specificity of 0.79 (95% CI: 0.76–0.81), a LR+ of 3.4 (95% CI: 2.5–4.6), a LR− of 0.36 (95% CI: 0.18–0.71) (see Table 4), and an AUC of 0.75 (95% CI: 0.64–0.87, P<0.01) (see Figure 2B). Furthermore, compared with video laryngoscopy, direct laryngoscopy had a sensitivity of 0.70 vs. 0.73, specificity of 0.75 vs. 0.80, AUC of 0.73 vs. 0.76 and a P value of 0.02 vs. P<0.01, respectively (see Table 5).
Table 4
| Physical examination | TP | TN | FP | FN | Sensitivity (95% CI) | Specificity (95% CI) | LR+ (95% CI) | LR− (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Neck mobility limitation | 6 | 919 | 45 | 15 | 0.29 (0.12–0.52) | 0.95 (0.94–0.97) | 6.1 (2.9–12.8) | 0.75 (0.57–0.98) |
| Airway stenosis | 8 | 934 | 30 | 13 | 0.38 (0.19–0.61) | 0.97 (0.96–0.98) | 12.2 (6.4–23.4) | 0.64 (0.46–0.89) |
| Outlook | 6 | 897 | 67 | 15 | 0.29 (0.12–0.52) | 0.93 (0.91–0.95) | 4.1 (2.0–8.4) | 0.77 (0.59–1.0) |
| 3-3-2 evaluation | 8 | 842 | 122 | 13 | 0.38 (0.19–0.61) | 0.87 (0.85–0.89) | 3.0 (1.7–5.3) | 0.71 (0.51–0.99) |
| Any one was positive | 15 | 761 | 203 | 6 | 0.71 (0.47–0.89) | 0.79 (0.76–0.81) | 3.4 (2.5–4.6) | 0.36 (0.18–0.71) |
TP, true positive; TN, true negative; FP, false positive; FN, false negative; CI, confidence interval; LR+, positive likelihood rate; LR−, negative likelihood rate.
Table 5
| Validity | Video laryngoscopy group | Direct laryngoscopy group |
|---|---|---|
| Sensitivity | 0.73 (0.39–0.93) | 0.70 (0.35–0.92) |
| Specificity | 0.80 (0.77–0.83) | 0.75 (0.68–0.81) |
| LR+ | 3.6 (2.4–5.3) | 2.8 (1.7–4.5) |
| LR− | 0.34 (0.13–0.90) | 0.4 (0.15–1.03) |
| AUC | 0.76 | 0.73 |
LR+, positive likelihood rate; LR−, negative likelihood rate; AUC, area under the curve.
Discussion
This multicentral survey of mainland Chinese EDs reflected the current incidence of difficult airways. It showed a relatively high incidence of bag-valve mask ventilation difficulties, but a low incidence of difficult airways during intubation. The four common physical evaluation methods we investigated in this study all had relatively low sensitivity and high specificity but did improve when combined. The results of this study apply to ED patients in China. It also has a certain reference value for Eds in other regions using the same evaluation index.
When looking at difficult bag-valve mask ventilation in this study, it happened more often than in other studies (8.2% in this study vs. 1.4–5% in previous studies) (11,12). Bag-valve mask ventilation before intubation is supposed to improve pre-intubation oxygen storage and lower the incidence of hypoxia during intubation (13). Bag-valve masks are relatively affordable medical devices, and are thus commonly used in the ED. Nevertheless, difficult bag-valve mask ventilation may reduce ventilation efficiency and lead to oxygen desaturation. Nowadays, commonly used evaluation parameters include: obesity, age over 55 years, snoring, lack of teeth, having facial hair, a Mallampati Class > II, and abnormal mandibular protrusion. Since many patients who need emergent intubation in the ED have one or more of these characteristics (e.g., age >55 was very common in our study), it is not surprising that the highest rate of difficulty in our study was with bag-valve mask ventilation. Further research effort is needed for better screening methods for difficult bag-valve mask ventilation (14).
In contrast, difficult intubation rates in the literature have suggested a 10% rate is common (5), which was higher than our results. This rate can vary between different hospital departments and has shown a descending trend with time (15,16). These may be connected to the increasing use of enhanced visualized equipment during intubation. In our study, 80.6% of intubators selected video laryngoscopy as their means to intubate. Video laryngoscopy is the recommended device when encountering difficult airways (17,18).
Despite the low incidence of difficult airways, adequate evaluation still plays an essential role before intubation. This study chose the four physical examination techniques commonly taught in Chinese emergency medicine residencies for screening for difficult airways. Some of the four have been checked for their diagnostic value or had been previously recommended in other studies (19,20). A secondary outcome of this study was to test the characteristics of combining the four physical examination techniques to hopefully improve the overall testing sensitivity for a difficult airway.
This study showed the diagnostic value of this assessment formula under challenging airway conditions in Chinese EDs. Our results identified a sensitivity of 0.44 and a specificity of 0.75 for the combined assessments compared with previous studies’ 0.22–0.67 sensitivity and 0.8–0.95 specificity for difficult laryngoscopy. This suggests that the combined test is on-par with other studies but does not seem particularly better or worse as far as its sensitivity. As for difficult intubation, our data showed a sensitivity of 0.71 and a specificity of 0.79. In contrast, other assessments ranged from 0.24 to 0.51 in sensitivity and 0.87 to 0.91 in specificity (21). This suggests a better sensitivity to the combined technique for finding difficult airways without sacrificing too much specificity. In addition, the predictive value (AUC) in difficult laryngoscopy (0.62) and intubation (0.79) presented certain value but were not ideal when compared with recent evidences (15,22). More standardized teaching strategies for Chinese ED practitioners who intubate may help improve the utility of these airway assessments. Also, a new evaluation index should be attempted on emergency patients for further improvement.
With the gradual popularization of visualization equipment, there are certain differences in the interpretation of the definition of the difficult airway (23,24). Risk predictors associated with direct laryngoscopy may not necessarily apply to video-laryngoscopy (25). Therefore, this study divided patients into a video laryngoscope and a direct laryngoscope intubation group. The results showed that the video laryngoscopy group had a higher predictive value, especially in predicting difficult endotracheal intubation. In the past, there were many studies on the predictive indicators of difficult airways under the condition of direct laryngoscopy intubation (26,27). In recent years, related researches are also increasing with the widespread application of video laryngoscopy (28,29). Although the evaluation indicators of the difficult airway of different types of laryngoscopes overlap, there are still differences. This phenomenon is consistent with the different predictive values of the two groups of evaluation indicators in this study.
Limitations
This was a multicentral survey-based study, which carries the limitations of survey research. The spectrum of difficult airway scenarios is unlikely to be captured over one month and ideally should be achieved via a long-term airway registry. This study and its results should be viewed as exploratory. Secondly, the experience and seniority of physicians performing difficult airway evaluation are uneven, and there may be some bias in the evaluation. However, the evaluation by front-line clinicians rather than the unified evaluation can reflect the real clinical situation to a certain extent, but it may underestimate the predictive value of the combined indicators. Thirdly, patients in different areas may have different facial features and combined disease, which may need extra airway examination. Fourthly, although the difficult bag-valve mask ventilation rate was relatively high, this study did not contain a prediction for it, which may be added to future studies. Finally, our study only selected four commonly used physical tests for difficult airway assessment. The sensitivity and predictive value might change if investigators used other determinants. Further study may extend the study period and include new valuable evaluation indicators.
Conclusions
This multicentral, cross-sectional survey of ED intubations in mainland Chinese EDs found a high incidence of difficult bag-valve mask ventilations, but relatively low rates of difficult intubations. The standard physical examination steps for prognosticating a difficult airway all had relatively low sensitivity and specificity, but improved when used in combination.
Acknowledgments
We are grateful to the CAMS (Chinese Academy of Medical Sciences) Innovation Fund for Medical Sciences grant for supporting this study. Also, we would like to thank to all participating hospitals for their help in collecting data for this study.
Funding: The CAMS (Chinese Academy of Medical Sciences) Innovation Fund for Medical Sciences Project number 2017-I2M-1-009).
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-199/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-199/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-199/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-199/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study received ethics approval from the ethics committee of Peking Union Medical College Hospital on December 22, 2020 (No. JS-2718). Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jayaraj AK, Siddiqui N, Abdelghany SMO, et al. Management of difficult and failed intubation in the general surgical population: a historical cohort study in a tertiary care centre. Can J Anaesth 2022;69:427-37. [Crossref] [PubMed]
- Joffe AM, Aziz MF, Posner KL, et al. Management of Difficult Tracheal Intubation: A Closed Claims Analysis. Anesthesiology 2019;131:818-29. [Crossref] [PubMed]
- Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 2022;136:31-81. [Crossref] [PubMed]
- Nørskov AK, Rosenstock CV, Wetterslev J, et al. Diagnostic accuracy of anaesthesiologists' prediction of difficult airway management in daily clinical practice: a cohort study of 188 064 patients registered in the Danish Anaesthesia Database. Anaesthesia 2015;70:272-81. [Crossref] [PubMed]
- Detsky ME, Jivraj N, Adhikari NK, et al. Will This Patient Be Difficult to Intubate?: The Rational Clinical Examination Systematic Review. JAMA 2019;321:493-503. [Crossref] [PubMed]
- Harris PA, Taylor R, Minor BLThe REDCap consortium, et al. Building an international community of software platform partners. J Biomed Inform 2019;95:103208. [Crossref] [PubMed]
- Heidegger T. Management of the Difficult Airway. N Engl J Med 2021;384:1836-47. [Crossref] [PubMed]
- Yentis SM, Lee DJ. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia 1998;53:1041-4. [Crossref] [PubMed]
- Lundstrøm LH, Møller AM, Rosenstock C, et al. A documented previous difficult tracheal intubation as a prognostic test for a subsequent difficult tracheal intubation in adults. Anaesthesia 2009;64:1081-8. [Crossref] [PubMed]
- Dai Y, Walline JH, Yu H, et al. Tracheal Intubation in Emergency Departments in China: A National Cross-Sectional Survey. Front Med (Lausanne) 2022;9:813833. [Crossref] [PubMed]
- Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology 2000;92:1229-36. [Crossref] [PubMed]
- Kheterpal S, Han R, Tremper KK, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology 2006;105:885-91. [Crossref] [PubMed]
- Casey JD, Janz DR, Russell DW, et al. Bag-Mask Ventilation during Tracheal Intubation of Critically Ill Adults. N Engl J Med 2019;380:811-21. [Crossref] [PubMed]
- Nørskov AK, Wetterslev J, Rosenstock CV, et al. Prediction of difficult mask ventilation using a systematic assessment of risk factors vs. existing practice - a cluster randomised clinical trial in 94,006 patients. Anaesthesia 2017;72:296-308. [Crossref] [PubMed]
- Srivilaithon W, Muengtaweepongsa S, Sittichanbuncha Y, et al. Predicting Difficult Intubation in Emergency Department by Intubation Assessment Score. J Clin Med Res 2018;10:247-53. [Crossref] [PubMed]
- Schroeder RA, Pollard R, Dhakal I, et al. Temporal Trends in Difficult and Failed Tracheal Intubation in a Regional Community Anesthetic Practice. Anesthesiology 2018;128:502-10. [Crossref] [PubMed]
- Liao CC, Liu FC, Li AH, et al. Video laryngoscopy-assisted tracheal intubation in airway management. Expert Rev Med Devices 2018;15:265-75. [Crossref] [PubMed]
- Suzuki K, Kusunoki S, Sadamori T, et al. Comparison of video and conventional laryngoscopes for simulated difficult emergency tracheal intubations in the presence of liquids in the airway. PLoS One 2019;14:e0220006. [Crossref] [PubMed]
- Artime CA, Roy S, Hagberg CA. The Difficult Airway. Otolaryngol Clin North Am 2019;52:1115-25. [Crossref] [PubMed]
- Pandit JJ, Irwin MG. Airway management in critical illness: practice implications of new Difficult Airway Society guidelines. Anaesthesia 2018;73:544-8. [Crossref] [PubMed]
- Roth D, Pace NL, Lee A, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst Rev 2018;5:CD008874. [Crossref] [PubMed]
- Aguilar K, Alferez GH, Aguilar C. Detection of difficult airway using deep learning. Mach Vision Appl 2020;31:4.
- Kauffman MB, Liu J, Urman RD, et al. A comparison of difficult intubation documentation practices with existing guidelines in the advent of video laryngoscopy. J Clin Anesth 2020;65:109807. [Crossref] [PubMed]
- Bradley JA, Urman RD, Yao D. Challenging the Traditional Definition of a Difficult Intubation: What Is Difficult? Anesth Analg 2019;128:584-6. [Crossref] [PubMed]
- Amaniti A, Papakonstantinou P, Gkinas D, et al. Comparison of Laryngoscopic Views betweenC-MAC™ and Conventional Laryngoscopy in Patients with Multiple Preoperative Prognostic Criteria of Difficult Intubation. An Observational Cross-Sectional Study. Medicina (Kaunas) 2019;55(:760.
- Mostafa M, Saeed M, Hasanin A, et al. Accuracy of thyromental height test for predicting difficult intubation in elderly. J Anesth 2020;34:217-23. [Crossref] [PubMed]
- Long B, Koyfman A, Gottlieb M. Factors Predicting Difficult Endotracheal Intubation. Acad Emerg Med 2019;26:1294-6. [Crossref] [PubMed]
- Joshi R, Hypes CD, Greenberg J, et al. Difficult Airway Characteristics Associated with First-Attempt Failure at Intubation Using Video Laryngoscopy in the Intensive Care Unit. Ann Am Thorac Soc 2017;14:368-75. [Crossref] [PubMed]
- Kim HJ, Kim HR, Kim SY, et al. Predictors of difficult intubation when using a videolaryngoscope with an intermediate-angled blade during the first attempt: a prospective observational study. J Clin Monit Comput 2022;36:1121-30. [Crossref] [PubMed]