
Uniportal vs. multiportal thoracoscopic segmentectomy: a north American study
Highlight box
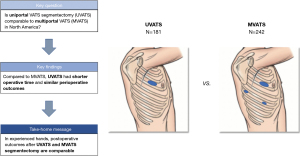
Key findings
• Uniportal video-assisted thoracoscopic surgery (UVATS) segmentectomy had shorter operative time compared to multiportal approach.
• We found no difference in perioperative outcomes.
What is known and what is new?
• Uniportal VATS segmentectomy is gaining worldwide acceptance, but experience in North America is still limited.
• We report the first multicenter North American study comparing perioperative outcomes between the two techniques.
What is the implication, and what should change now?
• In experienced hands, postoperative outcomes after Uniportal VATS and multiportal VATS segmentectomy are comparable.
• Further research is needed to confirm oncologic comparative effectiveness.
Introduction
Uniportal video-assisted thoracoscopic surgery (UVATS) was first described by Rocco in 2004 (1) and subsequently popularized by Gonzalez-Rivas (2). With the evolution of the technique and more refined instruments, experienced surgeons now perform even complex anatomic pulmonary resections through a single incision (3). Uniportal surgery has gained popularity worldwide however, adoption in North America has been slow (4).
The first UVATS segmentectomy was reported in 2012 (5) and since then, a few series were published supporting its feasibility and safety (6-9). Some investigators have compared outcomes between UVATS and multiportal VATS (MVATS) including both lobectomy and segmentectomy with small advantages to the uniportal approach (10-12). There is a paucity of data comparing both techniques for segmentectomy, and published experience seems almost exclusively from East Asian countries (13-17). Therefore, the aim of the present study was to report the first multicenter North American study comparing perioperative outcomes between UVATS and MVATS segmentectomy. We present the following article in accordance with the TREND reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-780/rc).
Methods
We conducted a retrospective chart review on a prospectively collected database from two North American tertiary academic centers; The University of Minnesota and the Institut Universitaire de Cardiologie et de Pneumonlogie de Quebec. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was independently assessed at the University of Minnesota (No. STUDY00016087), and the Institut Universitaire de Cardiologie et de Pneumologie de Quebec (No. 2018-2943, 21553) and deemed Institutional Review Board (IRB)-exempt. Individual patient’s consent was waived since the risk of loss of privacy for individuals was minimal, and the research could not practicably be conducted without the waiver.
We included all VATS segmentectomy patients from January 2012 to December 2020 in the analysis. We staged patients according to the eighth edition of the American Joint Commission on Cancer TNM staging system for non-small cell lung cancer. We utilized computerized tomography, positron emission tomography, brain imaging and invasive mediastinal staging according to international guidelines.
We defined UVATS segmentectomy according to the uniportal VATS interest group (UVIG) consensus report (18): (I) working incision length of ≤4 cm, (II) no use of a rib spreader at any stage of the operation and (III) pleural tube placed through the same incision at the end of the case. We classified MVATS as any patient with more than one skin incision. Data was analyzed in an intention to treat basis.
Demographics and clinical data included age, sex, body mass index (BMI), forced expiratory volume in 1 second (FEV1), diffusion capacity of the lung for carbon monoxide (DLCO), previous anatomic lung resection, tumor location, clinical and pathologic stage, histopathology, and smoking status. Invasive mediastinal staging was defined as histologic evaluation of mediastinal lymph nodes obtained by either transbronchial needle biopsies or mediastinoscopy. Comorbidities were graded utilizing the Charlson Comorbidity index (19). Perioperative outcomes included estimated blood loss, operating time, conversion to thoracotomy, duration of chest tube drainage, postoperative complications, length of hospital stay, 30-day readmission and 30-day mortality. Patient-reported pain scores were not included in the study since the postoperative pain control strategy was not equal at each center, a different pain assessment scale was used, and pain-related data was collected at different intervals. We recorded conversion to thoracotomy when the incision extended beyond 4 cm or when a rib spreader was used. Perioperative complications were defined and categorized according to the Clavien-Dindo classification (20). Prolonged air leak was defined as more than 5 days postoperatively. We did not have complete data on unplanned conversion to lobectomy in one of the centers since that information was captured as VATS lobectomy in the database. We classified specimens as R0 resection when a microscopically margin-negative resection was achieved. We recorded nodal upstaging when a clinically negative N1 or N2 lymph node had evidence of microscopic or gross metastatic disease on final pathology. We considered death from any cause in the first 30 days postoperatively a surgical death.
Segmentectomy criteria
Our criteria for segmentectomy include patient selection and anatomical feasibility. Patients with primary and secondary lung malignancy, subsolid nodules increasing in size or with a developing solid component, and solid indeterminate pulmonary nodules are considered for segmentectomy. Then, the chest computed tomography is carefully examined by the operating surgeon to assess: (I) location in the outer third of the lung parenchyma, (II) location within one or two adjacent bronchopulmonary segments (III) ensure a safety margin of 2 cm or tumor diameter can safely be achieved. We do not reserve parenchymal sparing surgery for patients with limited pulmonary reserve.
Surgical technique
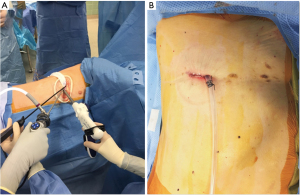
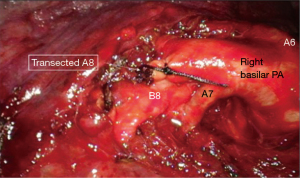
UVATS segmentectomy (Figure 1): we conduced surgery under general anesthesia with a double lumen endotracheal tube. The patient was positioned in lateral decubitus. We made a 3 to 4 cm skin incision located at the 5th or 6th intercostal space in the anterior-axillary line. We used a wound protector for exposure and utilized standard thoracoscopic instruments in conjunction with uniportal instruments for dissection. The technique used to perform segmentectomies was followed as described in detail by Okada and colleagues (21). We transected the segmental pulmonary veins and pulmonary arteries using either a vascular stapler, bipolar energy or between silk ligature depending on their size (Figure 2). The segmental bronchi were divided with either a surgical stapler or suture closed with vicryl. The delineation of the intersegmental plane was done by a combination of following the intersegmental veins, and by selective ventilation to create an inflation-deflation demarcation line. The parenchyma was divided with a surgical stapler. For lung cancer cases, we used intraoperative frozen exam routinely for regional N1 lymph nodes, and selectively for bronchial and parenchymal margins, to confirm absence of metastatic disease. If N1 lymph nodes were positive for malignancy, a completion lobectomy was performed.
MVATS segmentectomy: patients underwent similar anesthetic and patient positioning to UVATS. A 4 cm utility incision was made in the 4th or 5th intercostal space, one 12 mm port in the 8th intercostal space (posterior axillary line), and a 5 mm port just below the tip of the scapula. The technique used to perform segmentectomy was conducted in a similar fashion to UVATS, although uniportal instruments were not required for MVATS.
We routinely performed regional anesthesia to aid in postoperative pain control, using an erector spinae block, paravertebral catheter, or liposomal bupivacaine at the discretion of the operating team. We cared for patients in a step-down unit using a standardized enhanced recovery after surgery protocol for thoracic surgery, which was specific to each academic institution although they did not differ significantly in content.
Adoption of uniportal technique
The operations were performed by board certified thoracic surgeons, three of them were uniportal surgeons and eight of them multiportal surgeons. At the beginning of the study in 2012, both centers were performing MVATS exclusively. At one center, one surgeon (PU) adopted UVATS in 2014. At another center, one surgeon (RA) adopted UVATS in 2016, and another surgeon (ID) in 2018. By the time the surgeons adopted UVATS, they had different levels of experience with MVATS; 3 years (ID), 10 years (RA) and 15 years (PU). Once they became uniportal surgeons, they performed this technique exclusively. For the MVATS surgeons, their level of experience ranged from 5 to 20 years and did not differ significantly between centers.
Both groups were contemporary during the study period rather than sequential. The UVATS group was compared not only to the MVATS cases that were performed by uniportal surgeons prior to conversion, but to the other eight thoracic surgeons that were performing MVATS concurrently, and equally gaining experience with time.
Statistical analysis
Descriptive statistics were calculated and presented by groups, using median and interquartile range (IQR) for continuous variables and frequency and percentage for categorical variables. Continuous variables were compared between groups using Wilcoxon rank sum test and for categorical variables we used Chi-squared test or Fisher’s exact test if any cell count was 5 or less. Given the nonrandom treatment assignment and to minimize selection bias, we matched 1:1 uniportal patients and multiportal patients using propensity score matching methods. We performed a multivariate logistic model to calculate propensity scores for each patient accounting for the following covariates: age, sex, tumor location (upper or lower), Charlson Comorbidity Index, previous lung surgery, clinical tumor size (not pathologic), smoking status, BMI, and FEV1%. Standardized mean differences were assessed before and after matching. No differences were found after matching, when comparing demographics and baseline characteristics between the matched groups. We performed a post-match balance assessment and generated 2 groups with 156 patients in each cohort. Data was analyzed before and after propensity score matching and used SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). We considered P values less than 0.05 as statistically significant.
Results
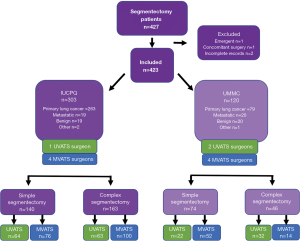
We performed a total of 427 VATS segmentectomies during the study period. We excluded emergent cases (n=1), segmentectomy performed in conjunction with another type of lung resection (n=1), and patients with incomplete records (n=2), leaving a total of 181 UVATS (42.7%) vs. 242 MVATS (57.2%) (Figure 3). Only two patients (1.1%) in the UVATS group were converted to MVATS due to technical difficulties. For the entire cohort the median age was 66 (59 to 71) years old, 272 patients were female (64.3%), and 151 patients were male (35.7%). The median FEV1 was 86% of predicted (74 to 99), median DLCO 89% of predicted (74 to 103) and median BMI was 27 (24 to 31). Indications for surgery were primary lung cancer (n=339), metastatic (n=41), benign disease (n=40), and other (n=3). We staged 85.1% of patients preoperatively with PET-CT scan.
Prior to matching, current smokers (P=0.05) and female patients (P=0.04) were more common in the UVATS group. There were no significant differences in all other baseline characteristics. Following propensity score matching the groups were balanced in all covariates and these differences were eliminated. Table 1 outlines the patient demographics and clinical data before and after propensity score matching. Table 2 describes the perioperative outcomes and Table 3 illustrates the distribution of simple vs. complex segmentectomy for the entire population.
Table 1
| Characteristics | Before matching | After matching | |||||
|---|---|---|---|---|---|---|---|
| UVATS, N=181 | MVATS, N=242 | P value | UVATS, N=156 | MVATS, N=156 | P value | ||
| Age (years) | 66 [58–71] | 66 [60–71] | 0.84 | 67 [60–71] | 66 [61–71] | 0.78 | |
| Female gender | 126 (69.6%) | 146 (60.3%) | 0.04 | 105 (67.3%) | 106 (67.9%) | 0.90 | |
| Charlson comorbidity index | 5 [4–6] | 5 [4–6] | 0.60 | 5 [4–6] | 5 [4–6] | 0.55 | |
| FEV1 (% pred) | 85 [73–99] | 87 [74–99] | 0.45 | 86 [74–99] | 88 [75–100] | 0.42 | |
| DLCO (% pred) | 91 [75–103] | 88 [73–103] | 0.63 | 91 [77–103] | 86 [73–102] | 0.36 | |
| Smoking status | 0.05 | 0.85 | |||||
| Never | 24 (13.3%) | 32 (13.2%) | 21 (13.5%) | 24 (15.4%) | |||
| Previous | 96 (53.3%) | 154 (63.6%) | 88 (56.4%) | 84 (53.8%) | |||
| Current | 60 (33.3%) | 56 (23.1%) | 47 (30.1%) | 48 (30.8%) | |||
| BMI (kg/m2) | 27 [23–31] | 27 [24–31] | 0.37 | 27 [23–30] | 27 [24–31] | 0.80 | |
| Tumor size (mm) | 15 [11–19] | 15 [12–19] | 0.29 | 16 [11–20] | 15 [12–18] | 0.81 | |
| Diagnosis | 0.83 | 1 | |||||
| Primary lung cancer | 145 (80.1%) | 197 (81.4%) | 127 (81.4%) | 127 (81.4%) | |||
| Metastatic | 18 (9.9%) | 21 (8.7%) | 14 (9.0%) | 14 (9.0%) | |||
| Benign | 16 (8.8%) | 23 (9.5%) | 13 (8.3%) | 14 (9.0%) | |||
| Other | 2 (1.1%) | 1 (0.4%) | 2 (1.3%) | 1 (0.6%) | |||
Data are presented in median [interquartile range] and n (%). UVATS, uniportal video-assisted thoracoscopic segmentectomy; MVATS, multiportal video-assisted thoracoscopic segmentectomy; BMI, body mass index; DLCO, diffusion capacity of the lungs for carbon monoxide; FEV1, forced expiratory volume in 1 second.
Table 2
| Outcome variable | Thoracoscopic segmentectomy | Simple segmentectomy | Complex segmentectomy | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| UVATS, N=156 | MVATS, N=156 | P value | UVATS, N=77 | MVATS, N=89 | P value | UVATS, N=79 | MVATS, N=67 | P value | |||
| Primary diagnosis | 1 | 0.06 | 0.32 | ||||||||
| Primary lung cancer | 127 (81.4%) | 127 (81.4%) | 69 (89.6%) | 70 (78.7%) | 58 (73.4%) | 57 (85.1%) | |||||
| Metastatic | 14 (9%) | 14 (9%) | 7 (9.1%) | 10 (11.2%) | 7 (8.9%) | 4 (6%) | |||||
| Benign | 13 (8.3%) | 14 (9%) | 1 (1.3%) | 8 (9%) | 12 (15.2%) | 6 (9%) | |||||
| Other | 2 (1.3%) | 1 (0.6%) | 0 | 1 (1.1%) | 2 (2.5%) | 0 | |||||
| Operating time (min) | 130 [106–170] | 161 [124–206] | <0.0001 | 133 [115–167] | 173 [122–220] | 0.0025 | 127 [102–175] | 148 [125–190] | 0.009 | ||
| EBL (mL) | 50 [20–118] | 50 [25–150] | 0.57 | 50 [20–150] | 50 [20–100] | 0.56 | 50 [20–100] | 100 [25–150] | 0.12 | ||
| Thoracotomy conversion | 5 (3.2%) | 6 (3.8%) | 1 | 2 (2.6%) | 5 (5.6%) | 0.45 | 3 (3.8%) | 1 (1.5%) | 0.62 | ||
| R0 resection | 134 (95.7%) | 144 (99.3%) | 0.07 | 69 (95.8%) | 89 (100.0%) | 0.09 | 65 (95.6%) | 59 (98.3%) | 0.62 | ||
| Nodal upstaging | 16 (11.3%) | 14 (9.7%) | 0.65 | 7 (9.6%) | 12 (14.5%) | 0.35 | 9 (13.2%) | 2 (3.3%) | 0.02 | ||
| Incidence of Clavien-Dindo III–IV | 19 (12.2%) | 12 (7.7%) | 0.18 | 8 (10.4%) | 8 (9.0%) | 0.76 | 11 (13.9%) | 4 (6.0%) | 0.17 | ||
| Hospital LOS (days) | 3 [2–5] | 3 [3–5] | 0.24 | 3 [2–5] | 3 [3–4] | 0.58 | 3 [2–5] | 4 [3–5] | 0.02 | ||
| Patients discharged POD#1 | 10 (6.4%) | 5 (3.2%) | 0.18 | 3 (3.9%) | 4 (4.5%) | 1 | 7 (8.9%) | 1 (1.5%) | 0.07 | ||
| 30-day readmission | 12 (7.7%) | 8 (5.1%) | 0.35 | 7 (9.1%) | 7 (7.9%) | 0.77 | 5 (6.3%) | 1 (1.5%) | 0.21 | ||
| 30-day mortality | 1 (0.6%) | 0 | 1 | 0 | 0 | 1 (1.3%) | 0 | 1 | |||
Data are presented in median (interquartile range) and n (%). UVATS, uniportal video-assisted thoracoscopic segmentectomy; MVATS, multiportal video-assisted thoracoscopic segmentectomy; EBL, estimated blood loss; LOS, length of stay; POD, postoperative day.
Table 3
| Segmentectomy | UVATS | MVATS | P value |
|---|---|---|---|
| Simple | N=86 (47.5%) | N=128 (52.8%) | 0.15 |
| Left upper lobe | |||
| Lingulectomy (S4, S5) | 15 | 21 | |
| Trisegmentectomy (S1+2, S3) | 18 | 23 | |
| Left lower lobe | |||
| Superior segmentectomy (S6) | 17 | 34 | |
| Basilar segmentectomy (S8–S10) | 8 | 4 | |
| Right lower lobe | |||
| Superior segmentectomy (S6) | 20 | 41 | |
| Basilar segmentectomy (S7–S10) | 8 | 5 | |
| Complex | N=95 (52.4%) | N=114 (47.1%) | 0.15 |
| Right upper lobe | |||
| S1 | 11 | 8 | |
| S2 | 20 | 29 | |
| S3 | 5 | 8 | |
| S1, S2 | 4 | 5 | |
| S1, S3 | 2 | 1 | |
| S2, S3 | 1 | – | |
| Right lower lobe | |||
| S6, S10 | 1 | 1 | |
| S7 | – | 3 | |
| S7, S8 | 3 | 4 | |
| S8 | 1 | 4 | |
| S8, S9 | – | 1 | |
| S9, S10 | 4 | 1 | |
| S10 | 1 | 1 | |
| Right middle lobe | |||
| S4 | 1 | – | |
| Right upper + lower lobe | |||
| S2, S6 | 3 | – | |
| S2, S7 | – | 1 | |
| Left upper lobe | |||
| S1+2 | 23 | 25 | |
| S3 | 1 | 2 | |
| S4 | 3 | 3 | |
| Left lower lobe | |||
| S6, S9, S10 | 1 | – | |
| S8 | 4 | 5 | |
| S8, S9 | 1 | 2 | |
| S9, S10 | 4 | – | |
| S10 | – | 3 | |
| Left upper + lower lobe | |||
| S1+2, S6 | – | 2 | |
| S1+2, S8 | – | 1 | |
| S1+2, S3, S6 | – | 2 | |
| S4, S5, S8 | – | 1 | |
| S4, S5, S8, S9, S10 | 1 | – | |
| S4, S8 | – | 1 |
MVATS, multiportal video-assisted thoracoscopic surgery; UVATS, uniportal video-assisted thoracoscopic surgery.
For the entire cohort, 123 patients (29%) had a total of 185 complications (Table 4). The most common postoperative morbidity was related to respiratory problems (62.6%), followed by cardiovascular (16%), genitourinary (7.4%), other (7.4%) and iatrogenic (6.7%) (Figure 4). The median follow-up was 18 months (range 7 to 38).
Table 4
| Complications | UVATS, n=181 | MVATS, n=242 | Total |
|---|---|---|---|
| Respiratory | |||
| Pleural effusion | 1 (0.6%) | 4 (2.5%) | 5 (3.1%) |
| ARDS | 3 (1.8%) | 0 | 3 (1.8%) |
| Pneumothorax | 6 (3.7%) | 7 (4.3%) | 13 (8%) |
| Mucus plug | 2 (1.2%) | 0 | 2 (1.2%) |
| Pneumonia | 11 (6.7%) | 8 (4.9%) | 19 (11.7%) |
| Bronchospasm | 1 (0.6%) | 1 (0.6%) | 2 (1.2%) |
| Empyema | 1 (0.6%) | 4 (2.5%) | 5 (3.1%) |
| Lung abscess | 1 (0.6%) | 0 | 1 (0.6%) |
| Persistent air leak | 18 (11%) | 30 (18.4%) | 48 (29.4%) |
| Pulmonary hemorrhage | 0 | 1 (0.6%) | 1 (0.6%) |
| Hemothorax | 0 | 2 (1.2%) | 2 (1.2%) |
| Bronchial dehiscence | 0 | 1 (0.6%) | 1 (0.6%) |
| Total | 44 (27%) | 58 (35.6%) | 102 (62.6%) |
| Cardiovascular | |||
| Cardiac arrhythmia | 16 (9.8%) | 10 (6.1%) | 24 (14.7%) |
| Pulmonary artery pseudoaneurysm | 1 (0.6%) | 0 | 1 (0.6%) |
| Cerebrovascular accident | 0 | 1 (0.6%) | 1 (0.6%) |
| Total | 17 (10.4%) | 11 (6.7%) | 26 (16%) |
| Genitourinary | |||
| Urinary tract infection | 3 (1.8%) | 3 (1.8%) | 6 (3.7%) |
| Acute renal failure | 2 (1.2%) | 4 (2.5%) | 6 (3.7%) |
| Total | 5 (3.1%) | 7 (4.3%) | 12 (7.4%) |
| Other | |||
| Wound infection | 1 (0.6%) | 7 (4.3%) | 8 (4.9%) |
| Chylothorax | 1 (0.6%) | 0 | 1 (0.6%) |
| Upper GI bleeding | 1 (0.6%) | 0 | 1 (0.6%) |
| Narcotic overdose | 1 (0.6%) | 0 | 1 (0.6%) |
| Malignant hyperthermia | 0 | 1 (0.6%) | 1 (0.6%) |
| Total | 4 (2.5%) | 8 (4.9%) | 12 (7.4%) |
| Iatrogenic | |||
| Vascular laceration | 1 (0.6%) | 3 (1.8%) | 4 (2.5%) |
| Recurrent laryngeal nerve palsy | 2 (1.2%) | 3 (1.8%) | 5 (3.1%) |
| Phrenic nerve palsy | 0 | 1 (0.6%) | 1 (0.6%) |
| Esophageal tear | 1 (0.6%) | 0 | 1 (0.6%) |
| Total | 4 (2.5%) | 7 (4.3%) | 11 (6.7%) |
Data are presented in number (%). UVATS, uniportal video-assisted thoracoscopic surgery; MVATS, multiportal video-assisted thoracoscopic surgery; ARDS, acute respiratory distress syndrome; GI, gastrointestinal.
Unmatched analysis
In the unmatched patient group analysis, hospital length of stay favored the UVATS group when compared to MVATS {3 [2–5] vs. 3 [3–5] days, P=0.03}, and operating time was significantly lower in the UVATS group, respectively {129 [107–169] vs. 161 [125–215] min, P<0.0001}. There were no differences in all other outcomes measured.
Propensity-matched analysis
After propensity-score matching, 156 patients who underwent UVATS and 156 patients who underwent MVATS were examined. Hospital length of stay was shorter in the UVATS group however, this difference did not persist after matching (P=0.24). Operating time was significantly lower in the UVATS group compared to the MVATS group {130 [106–170] vs. 161 [124–206] min, P<0.0001}. We found no difference in estimated blood loss, conversion to thoracotomy, nodal upstaging, incidence of Clavien-Dindo class III-IV complications, hospital length of stay, 30-day readmission or 30-day mortality. The rate of R0 resection before matching was 96.2% and 98.2% for UVATS and MVATS respectively (P=0.2), and after matching was 95.7% and 99.3% (P=0.07). Table 2 summarizes comparisons between the two groups.
Simple vs. complex segmentectomy
After propensity-score matching, the patients were stratified in two groups based on simple vs. complex segmentectomy, and perioperative outcomes were examined. For simple segmentectomy, operative time was shorter for UVATS {133 [115–167] min} compared to MVATS {173 [122–220] min, P=0.002}.
When complex segmentectomy was examined, we found shorter operating time, reduced hospital length of stay and increased nodal upstaging for UVATS (Table 2). No other differences in outcomes were found.
Discussion
We report a large cohort of UVATS segmentectomy from 2 North American centers over an 8-year period and demonstrated comparable perioperative outcomes compared to conventional MVATS. To our knowledge this is the first study from western countries comparing the two techniques. The three UVATS surgeons who participated in this study have different levels of experience ranging from 3 to 15 years and adopted the UVATS technique at different stages of their career. The eight MVATS surgeons had similar experience, ranging from 5 to 20 years, and did not differ significantly between centers. We believe that cumulative experience was not a significant confounding factor since the two groups were contemporary. Albeit the uniportal learning curve can have a negative effect on operating time and perioperative complications (22,23), we did not find a difference in perioperative outcomes. Furthermore, once the UVATS technique was adopted by the three uniportal surgeons, this approach was used exclusively thereafter which could explain the shorter operating time found in our series. Other investigators have also found shorter operating time for UVATS segmentectomy (16,17), although a larger series by Xie et al. failed to confirm this finding (17). We believe that our shorter operative times reflect improved efficiency with time and cumulative experience rather than an advantage of the uniportal technique itself. In any case, a median difference of 31 minutes between the two techniques is unlikely to have any clinical significance.
Table 5 summarizes the surgical outcomes of published series comparing UVATS vs. MVATS segmentectomy. We found no difference in intraoperative or postoperative complications with a median LOS of only 3 days. Our results contribute to the body of literature that confirms the safety and feasibility of UVATS segmentectomy. Moreover, the effectiveness of the UVATS technique is also supported by our findings of comparable rates of R0 resection, lymph node harvest and nodal upstaging. Prior to propensity score matching, the R0 resection rate for UVATS was 96.2%, which is comparable to a rate of 97.9% for MVATS found in a large National Cancer Data Base study (24). Following propensity score matching, there was a trend to lower R0 resection rate for UVATS although it did not reach statistical significance (P=0.07). To our knowledge, surgical margin status has not been reported previously for uniportal segmentectomy, and this requires further research with long-term follow-up to establish oncologic efficacy.
Table 5
| First author | Year | Country/region | Study type | N= (UVATS vs. MVATS) | Outcomes | Comment |
|---|---|---|---|---|---|---|
| Han (14) | 2016 | Korea | Single-center retrospective | 34 vs. 11 | Lower morbidity and shorter LOS in UVATS | Low power, relatively long LOS |
| Shih (13) | 2016 | Taiwan | Single-center retrospective, PSM | 54 vs. 46 (58 matched 1:1 after PSM) | Wound length smaller in UVATS. No difference in all other outcomes | Pre and post PSM groups differ considerably |
| Lee (15) | 2019 | Korea | Single-center retrospective | 33 vs. 51 | Lower EBL, shorter chest tube duration and LOS in UVATS | Single surgeon experience. Nonintubated anesthesia used in 72% of UVATS vs. 2% of MVATS |
| Chen (16) | 2020 | Taiwan | Single-center retrospective, PSM | 122 vs. 57 (56 matched 1:1 after PSM) |
Shorter chest tube duration and LOS in UVATS | Included only complex segmentectomy |
| Xie (17) | 2021 | China | Single-center retrospective, PSM | 537 vs. 519 (454 matched 1:1 after PSM) | UVATS: shorter chest tube duration and operating time in simple segmentectomy, longer operating time in complex segmentectomy. No difference in DFS or OS | Compared only two-port vs. single-port |
| Staging not clearly defined | ||||||
| Diaz-Gutierrez* | 2022 | USA/Canada | Two-center retrospective, PSM | 181 vs. 242 (156 matched 1:1 after PSM) | UVATS: shorter operating time in simple segmentectomy, shorter operating time, reduced LOS and increased nodal upstaging in complex segmentectomy |
*, current series. UVATS, uniportal video-assisted thoracoscopic surgery; MVATS, multiportal video-assisted thoracoscopic surgery; LOS, length of stay; PSM, propensity score matching; EBL, estimated blood loss; DFS, disease-free interval; OS, overall survival.
In terms of nodal upstaging, our rates are slightly higher than other published data however, we hypothesize this could be a reflection of a thorough lymphadenectomy. It is possible that inadequate staging was a contributing factor although, we believe this is less likely since we staged 85.1% of patients preoperatively with PET-CT scan according to NCCN guidelines. Further studies are needed in lung cancer patients to explore patterns and determinants of local recurrence and survival for UVATS vs. MVATS segmentectomy.
The potential advantages of UVATS segmentectomy over MVATS are less clear. In our series, when a subgroup of complex segmentectomy was examined, we found shorter operating time, reduced hospital length of stay and increased nodal upstaging for UVATS. It is conceivable that these results are a reflection of subtle differences in surgical technique that are otherwise not seen when the entire cohort is analyzed, although only prospective data could confirm this suggestion. In a single-center retrospective study Shih found only the length of the wound favored UVATS group (3.7 vs. 4.3 cm), but not all other outcomes measured (13). In a small series by Han et al. morbidity and hospital length of stay were lower in the UVATS cohort (14). A single-surgeon study by Lee et al. found lower blood loss, chest tube duration and length of stay in the uniportal group however, the anesthetic differed significantly between both groups: nonintubated anesthesia was used in 72% of UVATS patients compared to 2% of MVATS patients (15). Chen and colleagues also found lower chest tube duration and length of stay (16). Finally, a large cohort by Xie et al. comparing two-port vs. single-port segmentectomy found no significant difference in perioperative outcomes, with shorter operating time and chest tube duration for UVATS simple segmentectomy. Operating time was longer in UVATS for complex segmentectomy. There was no difference in overall survival or disease-free survival although, staging was not clearly defined in that study (17).
Despite the theoretical advantage of UVATS in terms of pain control compared to MVATS, very few studies have explored this benefit (25,26). Moreover, the only prospective randomized study to date comparing uniportal (n=51) vs. multiportal (n=55) lobectomy showed no differences in pain scores, morphine use or perioperative outcomes (27). We did not have patient-reported pain scores recorded and we did not investigate this outcome variable in our series.
In summary, we believe UVATS segmentectomy is a safe and feasible technique that could be performed by experienced thoracic surgeons without compromising results compared to MVATS segmentectomy. Although only a prospective randomized trial would definitively answer if one procedure is superior to the other, it is likely that the clinical difference of 1 versus 3 or 4 incisions is at best very small. Currently, the main significance of the uniportal approach is advancement of surgical techniques and individual surgeon development. A growth mindset leads to innovation, and innovation begets more innovation (28). A field can only grow if we take on new challenges, and small incremental innovation eventually leads to improved patient care (29).
A word of advice: there is no question that UVATS is a more challenging approach from the technical standpoint. The surgeon interested in adopting uniportal technique should follow evidence-based principles rather than trial and error. Patient selection is critical in the earlier stages, and as more experience is gained and the operator becomes competent, more complex procedures can be taken on. For example, S10 segmentectomy is particularly challenging for the UVATS technique because of the angle of the stapler is quite difficult to obtain when dividing S10 from S9. When using an MVATS approach, the additional inferior port can be very useful to introduce the stapler from a caudal-cranial direction.
Our study is limited by selection bias inherent to retrospective studies. Despite mitigating this confounding factor with propensity score matching, it could not be eliminated. We did not have data on unplanned conversion to lobectomy in one of the centers and therefore it was not included in the study. Also, we did not investigate pain control differences between the two groups due to lack of patient-reported scores. The surgeries were performed at large referral centers by surgeons experienced in uniportal surgery, and results may not be generalizable to other centers.
Conclusions
Our experience from two North American centers indicates that, in experienced hands, postoperative outcomes after UVATS and MVATS segmentectomy are comparable.
Acknowledgments
This study was presented as a poster at European Society of Thoracic Surgeons 29th annual meeting, June 2021.
Funding: Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1-TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-780/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-780/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-780/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was independently assessed at the University of Minnesota (No. STUDY00016087), and the Institut Universitaire de Cardiologie et de Pneumologie de Quebec (No. 2018-2943, 21553) and deemed Institutional Review Board (IRB)-exempt. Individual patient’s consent was waived since the risk of loss of privacy for individuals was minimal, and the research could not practicably be conducted without the waiver.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49:i6-16. [Crossref] [PubMed]
- Yeung C, Gilbert S. The state of uniportal video-assisted thoracoscopic surgery in North America: a survey of thoracic surgeons. J Vis Surg 2018;4:19. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [Crossref] [PubMed]
- Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5:S226-33. [Crossref] [PubMed]
- Han KN, Kim HK, Lee HJ, et al. Single-port video-assisted thoracoscopic pulmonary segmentectomy: a report on 30 cases†. Eur J Cardiothorac Surg 2016;49:i42-7. [Crossref] [PubMed]
- Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. [Crossref] [PubMed]
- Xie D, Wang H, Fei K, et al. Single-port video-assisted thoracic surgery in 1063 cases: a single-institution experience†. Eur J Cardiothorac Surg 2016;49:i31-6. [Crossref] [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Mu JW, Gao SG, Xue Q, et al. A Matched Comparison Study of Uniportal Versus Triportal Thoracoscopic Lobectomy and Sublobectomy for Early-stage Nonsmall Cell Lung Cancer. Chin Med J (Engl) 2015;128:2731-5. [Crossref] [PubMed]
- Bin Yameen TA, Gupta V, Behzadi A. Uniportal versus multiportal video-assisted thoracoscopic surgery in the treatment of lung cancer: a Canadian single-centre retrospective study. Can J Surg 2019;62:468-74. [Crossref] [PubMed]
- Shih CS, Liu CC, Liu ZY, et al. Comparing the postoperative outcomes of video-assisted thoracoscopic surgery (VATS) segmentectomy using a multi-port technique versus a single-port technique for primary lung cancer. J Thorac Dis 2016;8:S287-94. [Crossref] [PubMed]
- Han KN, Kim HK, Choi YH. Comparison of single port versus multiport thoracoscopic segmentectomy. J Thorac Dis 2016;8:S279-86. [Crossref] [PubMed]
- Lee J, Lee JY, Choi JS, et al. Comparison of Uniportal versus Multiportal Video-Assisted Thoracoscopic Surgery Pulmonary Segmentectomy. Korean J Thorac Cardiovasc Surg 2019;52:141-7. [Crossref] [PubMed]
- Chen YY, Huang WL, Chang CC, et al. Uniportal versus Multiportal Thoracoscopic Complex Segmentectomy: Propensity Matching Analysis. Ann Thorac Cardiovasc Surg 2021;27:237-43. [Crossref] [PubMed]
- Xie D, Wu J, Hu X, et al. Uniportal versus multiportal video-assisted thoracoscopic surgery does not compromise the outcome of segmentectomy. Eur J Cardiothorac Surg 2021;59:650-7. [Crossref] [PubMed]
- Bertolaccini L, Batirel H, Brunelli A, et al. Uniportal video-assisted thoracic surgery lobectomy: a consensus report from the Uniportal VATS Interest Group (UVIG) of the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;56:224-9. [Crossref] [PubMed]
- Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245-51. [Crossref] [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Nomori H, Okada M. Illustrated anatomical segmentectomy for lung cancer. Springer Science & Business Media; 2012 Dec 22.
- Vieira A, Bourdages-Pageau E, Kennedy K, et al. The learning curve on uniportal video-assisted thoracic surgery: An analysis of proficiency. J Thorac Cardiovasc Surg 2020;159:2487-95.e2. [Crossref] [PubMed]
- Li S, Wu J, Wan Z, et al. The learning curve for uniportal video-assisted thoracoscopic anatomical segmentectomy. J Surg Oncol 2021;124:441-52. [Crossref] [PubMed]
- Khullar OV, Liu Y, Gillespie T, et al. Survival After Sublobar Resection versus Lobectomy for Clinical Stage IA Lung Cancer: An Analysis from the National Cancer Data Base. J Thorac Oncol 2015;10:1625-33. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49:i37-41. [Crossref] [PubMed]
- Ji C, Xiang Y, Pagliarulo V, et al. A multi-center retrospective study of single-port versus multi-port video-assisted thoracoscopic lobectomy and anatomic segmentectomy. J Thorac Dis 2017;9:3711-8. [Crossref] [PubMed]
- Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016;50:411-5. [Crossref] [PubMed]
- Andrade R, Bhargava A. No pain, no gain. Eur J Cardiothorac Surg 2018;54:969-70. [Crossref] [PubMed]
- Andrade R. Commentary: Why do uniportal video-assisted thoracoscopic lobectomy? J Thorac Cardiovasc Surg 2020;159:2496-7. [Crossref] [PubMed]


