The growing impact of air quality on lung-related illness: a narrative review
Introduction
The study of ambient air quality and its deleterious effects on human health have been brought to the forefront in recent times. Poor air quality has been tied to multiple respiratory diseases, ranging from asthma and bronchitis to long-term heart and lung diseases (1-6). Outdoor air pollution constitutes one of the leading global health risks. Fine particulate matter (PM2.5) describes particles with an aerodynamic diameter of less than 2.5 mm. Environmental pollutants have been identified as being among the top five causes of death globally (7). In addition, PM2.5 has been demonstrated to cause epigenetic and micro-environmental alterations in the lung and is linked to the development of lung cancer (8,9). Radon gas and smoke from burning domestic fuels further elevate lung cancer risk when exposed over extended periods of time (10). We present a narrative review of the literature outlining the current work done on ambient air quality and lung diseases. We present this article in accordance with the Narrative Review reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-544/rc).
Methods
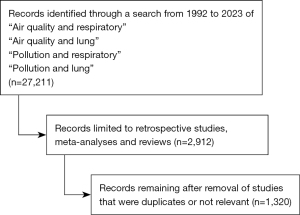
We reviewed all articles using terms via PubMed, MEDLINE, and Google Scholar. The eligible studies were searched from 1 March 1992 to 1 March 2023. Our search queried “Air quality and respiratory”, “air quality and lung”, “pollution and respiratory” and “pollution [and] lung”. Our search was limited to retrospective studies, meta-analyses, abstracts and reviews (Table 1). Reviews and meta-analyses were included only for cross-reference check. After removal of duplicates and studies that were not relevant, a total of 1,320 studies remained. These studies were reviewed, and in total 68 references were included in this narrative (Figure 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | March 15, 2023 |
| Databases and other sources searched | PubMed, MEDLINE, Google Scholar |
| Search terms used | “Air quality and respiratory”, “Air quality and lung”, “Pollution and respiratory”, “Pollution and lung” |
| Timeframe | 1992–2023 |
| Inclusion criteria | Retrospective studies, meta-analyses, abstracts and reviews |
| Selection process | All authors participated in the selection process. Consensus was obtained through group discussion |
Discussion
Air quality over time
The Clean Air Act of 1970 (CAA) has undoubtedly had a beneficial impact on air quality in the United States, setting national standards for pollution levels and requiring industries and transportation sources to lessen their emissions. The CAA also included a grant program that provided local and state governments the necessary funds to collaborate with the Environmental Protection Agency (EPA) in improving air quality (11). According to EPA data, concentrations of six major pollutants such as ozone, carbon monoxide, lead, PM, nitrogen dioxide (NO2) and sulfur dioxide (SO2) have all declined since this legislation was passed decades ago. These reductions range between 70 to 90 percent depending on location. This reduction was due mainly more efficient emission control systems and cleaner fuel alternatives (12). Nonetheless, warmer temperatures have led to an increase in pollutant levels and accumulation in toxic smoke from wildfires (13,14). While certain restrictions have been imposed on automobile emissions and factories, they still constitute some of the most common sources of contamination.
Regional differences in air quality
Urban vs. suburban
Urban air quality can be impacted by a wide range of causes, from industrial emissions to vehicle exhaust and construction activities. Structures in these areas, such as buildings and infrastructure, trap pollutants and further worsen air quality. This problem has been intensified by increased population densities in cities compared with their suburban or rural counterparts (15,16). In addition, industrial production and transportation are more prevalent in cities and further contribute to air pollution. Suburban air quality is typically better than urban areas due to lower population density and fewer sources of pollution (17). Nevertheless, emissions from industrial sites in the vicinity, vehicle exhausts from nearby roads and highways and topography may influence pollutant concentrations and PM2.5 levels in suburban areas (18).
Different parts of the United States
The United States is composed of a wide array of air quality levels, from highly polluted urban areas to very clean rural regions. The northeastern region of the United States is a densely populated area with numerous industrial and transportation sources that contribute to air pollution. Cities such as New York, Boston and Philadelphia face some of the most serious challenges in dealing with elevated PM2.5, nitric oxide (NO2) and ozone levels (19-21). Major cities in the southeast, including Atlanta, Charlotte, and Houston, are heavily populated and have a warm, humid climate that often contributes to air pollution (22). These cities experience high levels of ozone, PM2.5 and NO2 from industrial activities and transportation sources. The Midwest region of the United States has a powerful agricultural and industrial infrastructure which unfortunately produces copious amounts of air pollution, particularly PM2.5 and NO2 (23). Major cities like Chicago, St. Louis, and Detroit can be especially vulnerable to adverse levels of these pollutants in the summer. The western region of the United States has been marred by alarming concentrations of air pollutants, such as PM2.5, NO2 and ozone. These contaminants are mainly derived from vehicular exhaust emissions, industries, and wildfires in cities like Los Angeles, San Francisco, and Seattle. These contaminants pose a serious threat to both public health and environmental integrity (24).
Different parts of world
The results of air pollutants have extended beyond certain regions and had a global impact. The Canadian Air and Precipitation Monitoring Network (CAPMoN) has observed a marked improvement in air quality in Canadian cities during the past two decades, in spite of ongoing challenges from industrial emissions, transportation-associated pollutants and wildfires. Comparable improvements have been made in air quality throughout Europe, mostly from regulations passed by various governments. These regulations were enacted to curb emissions from commercial sites, automobiles and energy production sources. According to the European Environment Agency, there have been significant reductions in PM2.5 and NO2 concentrations throughout Europe. Urban sectors generally face higher pollution rates than rural localities, however, mainly in cities where traffic density is considerable (25). The Health Effects Institute’s 2020 State of Global Air Report confirmed that outdoor air pollutants led to 4.5 million fatalities globally in 2019. Most of these mortalities occurred in Asian countries. The Global Air Report also revealed that 84% of the worldwide population resides where PM2.5 levels exceeded recommended limits by the World Health Organization (WHO) (26). Africa is frequently disregarded in discussions about air quality. But many African cities are facing significant issues with air pollution due to the burning of solid fuels for home use, vehicles emitting exhaust fumes and emissions from industries. The United Nations Environment Programme reported that air pollution has taken its toll on Africa’s population, now responsible for over 700,000 premature deaths every year. Children, elderly individuals and people with chronic diseases suffer more significantly after being exposed to increased pollutant levels (27).
Climate change
Human activities that emit large volumes of greenhouse gases into the atmosphere are the fundamental driver of climate change. These pollutants absorb and retain solar heat, rising global temperatures, modify precipitation patterns, affect wind speeds and have severe implications for ecosystems and people around the planet. Rising sea levels, melting glaciers and fatal severe weather events are all negative consequences of climate change. As a result, climate change has the potential to affect air quality dramatically by escalating the levels of pollutants and allergens in the atmosphere. Higher temperatures can boost ground-level ozone as well as pollen production. Natural disasters such as fires have become more common and severe as a result of climate change. These disasters often result in a substantial amount of PM2.5 being discharged into the air (28).
Reasons for change in air quality
Manufacturing
The emission of numerous contaminants into the environment during manufacturing operations has a severe effect on air quality. The combustion of fossil fuels such as coal or oil, for example, can emit a range of pollutants including SO2, NO2, and PM2.5. Furthermore, the use of chemicals and solvents can release volatile organic compounds (VOCs) into the air, which can then react with other pollutants and form ground level ozone. The energy consumed by facilities can result in emissions of greenhouse gases, such as carbon dioxide (29). In particular, daily and chronic occupational exposures place workers at increased risk of developing respiratory diseases (30-34). By reducing emissions from these manufacturing operations, employees would be exposed to less polluted work environments and the overall air quality would improve for everyone.
Traffic density
Traffic density can affect air quality due to harmful emissions from automobiles. These pollutants include carbon monoxide, nitrogen oxides, and small particles, all of which can damage human health and the environment. The number of cars on the road and the amount of air pollution increases with greater traffic density. In metropolitan regions with high vehicle and human densities, traffic density is often heavy. Those individuals who live or work close to major roads or highways are therefore more likely to be exposed to pollution. Additionally, changes in temperature, precipitation patterns, and meteorological events brought on by the release of greenhouse gases can have a variety of detrimental effects on air quality (15).
Increase in billions of gallons used each year
The burning of fossil fuels results in an alarming quantity of pollutants being launched into the atmosphere, with contaminants such as carbon monoxide, NO2 and PM2.5. These emissions can have negative consequences for human health and long-term environmental damage. Greater use of these fuels has led to a surge in greenhouse gas emissions that can affect air quality, temperatures, precipitation levels and atmospheric patterns. In regions with excessive automobile traffic, vehicle exhaust is a prime contributor to this airborn pollution. Industries that are heavily dependent upon fossil fuels to generate energy will amplify atmospheric pollution as demand for fuel increases. This development is further compounded by the fact that there will be a corresponding spike in emissions from these operations (35).
Natural events and weather
Natural occurrences such as wildfires, dust storms, volcanic eruptions and changes in weather patterns can also impact air quality. One illustration is stagnant air conditions, which can trap pollutants near the earth surface and increase the amounts of pollutants like ozone and PM2.5 in the atmosphere. Strong winds can spread contaminants and enhance air quality (36).
Disparities in asthma incidence and mortality
Urban vs. suburban
As researchers have identified social determinants of health to be critical in understanding disparities in asthma incidence and mortality. Of these social determinants of health, one of the most critical is housing (37). Compared to their suburban counterparts, urban housing has been found to have higher incidences of indoor asthma-triggering allergens like mold, pest and dust mite allergens (38). In a study of urban homes, a pooled analysis found that housing conditions including water leaks, the presence of cracks and holes in walls, and homes built prior to 1951 were associated with a higher risk of exposure to asthma allergens (39). Additionally, in a low-income urban setting, homeowners are limited by the cost burden of the repairs that would decrease allergen exposure and renting tenants have limited control over the maintenance of their homes (40,41). Low-quality housing influences the incidence of asthma, and racial and ethnic minorities in these homes are disproportionately affected. This structural racism over multiple decades stems from historical discriminatory housing practices (42,43).
Race and other social determinants vs. asthma incidence and outcome
Race and ethnicity are social determinants of health that have been shown to affect asthma burden (44,45). Reviews have shown that rates of uncontrolled asthma are higher in African American and Hispanic children. Also, minority children seen by minority-serving providers are less likely to receive inhaled steroids from community health clinics and hospital clinics. Additionally, a report has attributed disparities in race and ethnicity to socioeconomic status. Hughes and colleagues found that even when controlling for socioeconomic status, non-Hispanic black households were more likely to have children with an asthma diagnosis and have asthma-related emergency department visits (46). Regarding outcomes, African American and Hispanic children have more indicators of poorly controlled asthma including higher rates of emergency room visits, rescue medication usage and lower use of inhaled corticosteroids for maintenance therapy (47). A large national-level study showed that when combining both inpatient and outpatient mortality, Black and Hispanic children were at increased risk of mortality (48,49). These associations highlight the disparities in asthma care in the outpatient and pre-hospital settings.
Relationship of air quality with asthma
The World Health Organization (WHO) has set firm standards for air quality and unfortunately, nearly 99% of the planet’s population lives with air pollution that surpasses these guidelines (50). Air contamination can take on two distinct forms—gaseous or PM—which together negatively affect both outdoor and indoor air quality. Sources of this hazardous contamination include fires, cigarette smoke, and most notably fuel-burning activities such as cars on the road (51). It is therefore crucial to mitigate these pollutants in order to ensure safe living spaces now and in the future. Additionally, exposure to traffic-related air pollutants has been linked to the development of asthma in children. Yet, its effects on adult asthma remain unknown. However, it is believed that inhaling outdoor pollutants can lead to increases in both asthma symptoms and hospitalizations in a very direct fashion; longer exposure and a greater level of pollution only exacerbate the condition (52).
Lung cancer incidence and trend over the last 40 years
The American Cancer Society reports that there were 236,740 new cases of lung cancer in the United States in 2022. Of these cases, 117,910 cases occurred in males and 118,830 cases occurred in females (53). The estimated number of deaths from lung cancer in 2022 was 130,180. In the last 40 years, there has been an overall decline in both the incidence and mortality from lung cancer. The decline in lung cancer incidence has primarily been attributed to decreases in smoking rates. Changes in lung cancer incidence among non-smokers remain unclear.
Relationship of air quality with other lung-related illnesses
The quality of indoor and outside air is often harmed by various pollutants and has been associated with the development of multiple lung-related illnesses. Previous literature has established a connection between unfavorable air conditions and COPD exacerbations (54). In addition to its long-term impact, air pollution can have short-term negative health consequences. Furthermore, air pollution may be responsible for increasing the likelihood of respiratory infections, both upper and lower respiratory illnesses, by altering the lung microbiome (55). It has been widely accepted that poor air quality and elevated levels of PM2.5 can have severe adverse effects on a variety of lung diseases. Idiopathic pulmonary fibrosis and cystic fibrosis are two respiratory diseases that have been linked to poor environmental factors (56,57). However, research into the relationship between air pollution and pneumoconiosis or benign lung tumors is still inconclusive. Further research is required to gain a thorough understanding of the potential long-term health impacts associated with airborne pollutants (58).
Relationship of air quality with lung cancer
While smoking and tobacco use are the main risk factors for lung cancer, air pollutants and PM2.5 were classified as a class 1 human carcinogen by the International Agency for Research on Cancer in 2013 (59). Particularly amongst non-smokers, air pollutants are of great interest as a mechanism of lung cancer development. Several epidemiological, observational research and meta-analyses have validated this link (60-62). Particulate matter smaller than 2.5 µm have generated special concern as a carcinogen due to their very porous surface, which allows them to transmit cancer-causing substances into the respiratory system. One prospective study revealed that exposure to environmental pollution may work in concert with a genetic propensity to cause lung cancer (63). Furthermore, a recent article by Xue and colleagues emphasizes the numerous air contaminants that have been related to the occurrence of cancer as well as the pathophysiological processes that include oxidative stress, epigenetic modifications and direct DNA damage (64). There are also numerous international studies that support an association between air quality and lung cancer (65,66).
Small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC) are two of the more prevalent pulmonary neoplasms, and both are associated with a variety of ecological factors. SCLC is occasionally linked to long-term exposure to hazardous substances like asbestos fibers and radon gas. Prolonged exposure to pollutants such as PM2.5 and NO2 have a direct correlation to NSCLC incidence, increasing relative risk by 1.54 compared to those not exposed (59). Interestingly, exposure to PM2.5 even within the first 2 months after undergoing lung cancer resection may drastically reduce the survival of patients with lung cancer (67). Collectively, these results illustrate the association of air pollution and lung cancer.
Conclusions
Air pollution is an environmental hazard that is associated with the development of lung-related illnesses. Improving air quality will reduce the incidence of these diseases. Raising awareness is a pivotal step in safeguarding both the environment and public health. Future research should continue to investigate the links and underlying causes between poor air quality and lung disease. Ultimately, improving air quality is a complicated process that demands a multifaceted approach and tailored solutions to be effective.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-544/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-544/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-544/coif). ICO serves as an unpaid editorial board member of Journal of Thoracic Disease from February 2023 to January 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Manisalidis I, Stavropoulou E, Stavropoulos A, et al. Environmental and Health Impacts of Air Pollution: A Review. Front Public Health 2020;8:14. [Crossref] [PubMed]
- Thurston GD, Kipen H, Annesi-Maesano I, et al. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J 2017;49:1600419. [Crossref] [PubMed]
- Schraufnagel DE, Balmes JR, Cowl CT, et al. Air Pollution and Noncommunicable Diseases: A Review by the Forum of International Respiratory Societies' Environmental Committee, Part 1: The Damaging Effects of Air Pollution. Chest 2019;155:409-16. [Crossref] [PubMed]
- De Matteis S, Forastiere F, Baldacci S, et al. Issue 1 - "Update on adverse respiratory effects of outdoor air pollution". Part 1): Outdoor air pollution and respiratory diseases: A general update and an Italian perspective. Pulmonology 2022;28:284-96. [Crossref] [PubMed]
- Huang Y, Zhu M, Ji M, et al. Air Pollution, Genetic Factors, and the Risk of Lung Cancer: A Prospective Study in the UK Biobank. Am J Respir Crit Care Med 2021;204:817-25. Erratum in: Am J Respir Crit Care Med 2022;205:1254. [Crossref] [PubMed]
- Stafoggia M, Oftedal B, Chen J, et al. Long-term exposure to low ambient air pollution concentrations and mortality among 28 million people: results from seven large European cohorts within the ELAPSE project. Lancet Planet Health 2022;6:e9-e18. [Crossref] [PubMed]
- Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017;389:1907-18. Erratum in: Lancet 2017;389:e15 Erratum in: Lancet 2018;391:1576. [Crossref] [PubMed]
- Li R, Zhou R, Zhang J. Function of PM2.5 in the pathogenesis of lung cancer and chronic airway inflammatory diseases. Oncol Lett 2018;15:7506-14. [Crossref] [PubMed]
- Hughes BD, Maharsi S, Obiarinze RN, et al. Correlation between air quality and lung cancer incidence: A county by county analysis. Surgery 2019;166:1099-104. [Crossref] [PubMed]
- Corrales L, Rosell R, Cardona AF, et al. Lung cancer in never smokers: The role of different risk factors other than tobacco smoking. Crit Rev Oncol Hematol 2020;148:102895. [Crossref] [PubMed]
- Ross K, Chmiel JF, Ferkol T. The impact of the Clean Air Act. J Pediatr 2012;161:781-6. [Crossref] [PubMed]
- Hankey S, Marshall JD. Urban Form, Air Pollution, and Health. Curr Environ Health Rep 2017;4:491-503. [Crossref] [PubMed]
- D'Amato G, Bergmann KC, Cecchi L, et al. Climate change and air pollution: Effects on pollen allergy and other allergic respiratory diseases. Allergo J Int 2014;23:17-23. [Crossref] [PubMed]
- D'Evelyn SM, Jung J, Alvarado E, et al. Wildfire, Smoke Exposure, Human Health, and Environmental Justice Need to be Integrated into Forest Restoration and Management. Curr Environ Health Rep 2022;9:366-85. [Crossref] [PubMed]
- Zhang K, Batterman S. Air pollution and health risks due to vehicle traffic. Sci Total Environ 2013;450-451:307-16. [Crossref] [PubMed]
- Liang L, Gong P. Urban and air pollution: a multi-city study of long-term effects of urban landscape patterns on air quality trends. Sci Rep 2020;10:18618. [Crossref] [PubMed]
- Larkin A, van Donkelaar A, Geddes JA, et al. Relationships between Changes in Urban Characteristics and Air Quality in East Asia from 2000 to 2010. Environ Sci Technol 2016;50:9142-9. [Crossref] [PubMed]
- Miller P. Health Impacts of Suburban Development Patterns. Dela J Public Health 2018;4:32-5. [Crossref] [PubMed]
- Thurston GD, Ito K, Kinney PL, et al. A multi-year study of air pollution and respiratory hospital admissions in three New York State metropolitan areas: results for 1988 and 1989 summers. J Expo Anal Environ Epidemiol 1992;2:429-50.
- Koutrakis P, Suh HH, Sarnat JA, et al. Characterization of particulate and gas exposures of sensitive subpopulations living in Baltimore and Boston. Res Rep Health Eff Inst 2005;1-65; discussion 67-75.
- Schwartz J, Dockery DW. Increased mortality in Philadelphia associated with daily air pollution concentrations. Am Rev Respir Dis 1992;145:600-4. [Crossref] [PubMed]
- Zhang JJ, Wei Y, Fang Z. Ozone Pollution: A Major Health Hazard Worldwide. Front Immunol 2019;10:2518. [Crossref] [PubMed]
- Clarke K, Manrique A, Sabo-Attwood T, et al. A Narrative Review of Occupational Air Pollution and Respiratory Health in Farmworkers. Int J Environ Res Public Health 2021;18:4097. [Crossref] [PubMed]
- Xie Y, Lin M, Decharme B, et al. Tripling of western US particulate pollution from wildfires in a warming climate. Proc Natl Acad Sci U S A 2022;119:e2111372119. [Crossref] [PubMed]
- Fowler D, Brimblecombe P, Burrows J, et al. A chronology of global air quality. Philos Trans A Math Phys Eng Sci 2020;378:20190314. Erratum in: Philos Trans A Math Phys Eng Sci 2021;379:20210113. [Crossref] [PubMed]
- Rodríguez-Urrego D, Rodríguez-Urrego L. Air quality during the COVID-19: PM(2.5) analysis in the 50 most polluted capital cities in the world. Environ Pollut 2020;266:115042. [Crossref] [PubMed]
- Fisher S, Bellinger DC, Cropper ML, et al. Air pollution and development in Africa: impacts on health, the economy, and human capital. Lancet Planet Health 2021;5:e681-8. [Crossref] [PubMed]
- Shivanna KR. Climate change and its impact on biodiversity and human welfare. Proc Indian Natl Sci Acad 2022;88:160-71.
- Rahman MM, Alam K, Velayutham E. Is industrial pollution detrimental to public health? Evidence from the world's most industrialised countries. BMC Public Health 2021;21:1175. [Crossref] [PubMed]
- De Matteis S, Jarvis D, Darnton L, et al. Lifetime occupational exposures and chronic obstructive pulmonary disease risk in the UK Biobank cohort. Thorax 2022;77:997-1005. [Crossref] [PubMed]
- Doiron D, de Hoogh K, Probst-Hensch N, et al. Air pollution, lung function and COPD: results from the population-based UK Biobank study. Eur Respir J 2019;54:1802140. [Crossref] [PubMed]
- Thurston GD, De Matteis S, Murray K, et al. Maximizing the Public Health Benefits from Climate Action. Environ Sci Technol 2018;52:3852-3. [Crossref] [PubMed]
- Hajat A, Hsia C, O'Neill MS. Socioeconomic Disparities and Air Pollution Exposure: a Global Review. Curr Environ Health Rep 2015;2:440-50. [Crossref] [PubMed]
- Rabbani G, Nimmi N, Benke GP, et al. Ever and cumulative occupational exposure and lung function decline in longitudinal population-based studies: a systematic review and meta-analysis. Occup Environ Med 2023;80:51-60. [Crossref] [PubMed]
- Perera F. Pollution from Fossil-Fuel Combustion is the Leading Environmental Threat to Global Pediatric Health and Equity: Solutions Exist. Int J Environ Res Public Health 2017;15:16. [Crossref] [PubMed]
- De Sario M, Katsouyanni K, Michelozzi P. Climate change, extreme weather events, air pollution and respiratory health in Europe. Eur Respir J 2013;42:826-43. [Crossref] [PubMed]
- Bryant-Stephens TC, Strane D, Robinson EK, et al. Housing and asthma disparities. J Allergy Clin Immunol 2021;148:1121-9. [Crossref] [PubMed]
- Institute of Medicine (US) Committee on the Assessment of Asthma and Indoor Air. Clearing the Air: Asthma and Indoor Air Exposures. Washington (DC): National Academies Press (US); 2000.
- Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med 2004;351:1068-80. [Crossref] [PubMed]
- Elliott L, Arbes SJ, Harvey ES, et al. Dust weight and asthma prevalence in the National Survey of Lead and Allergens in Housing (NSLAH). Environ Health Perspect 2007;115:215-20. [Crossref] [PubMed]
- Grineski SE, Hernández AA. Landlords, fear, and children’s respiratory health: an untold story of environmental injustice in the central city. Local Environ 2010;15:199-216.
- Woods LL 2nd, Shaw-Ridley M, Woods CA. Can health equity coexist with housing inequalities? A contemporary issue in historical context. Health Promot Pract 2014;15:476-82. [Crossref] [PubMed]
- Hirt S. The rules of residential segregation: US housing taxonomies and their precedents. Planning Perspectives 2015;30:367-95.
- Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol 2009;9:154-60. [Crossref] [PubMed]
- Grant T, Croce E, Matsui EC. Asthma and the social determinants of health. Ann Allergy Asthma Immunol 2022;128:5-11. [Crossref] [PubMed]
- Hughes HK, Matsui EC, Tschudy MM, et al. Pediatric Asthma Health Disparities: Race, Hardship, Housing, and Asthma in a National Survey. Acad Pediatr 2017;17:127-34. [Crossref] [PubMed]
- Crocker D, Brown C, Moolenaar R, et al. Racial and ethnic disparities in asthma medication usage and health-care utilization: data from the National Asthma Survey. Chest 2009;136:1063-71. [Crossref] [PubMed]
- Glick AF, Tomopoulos S, Fierman AH, et al. Disparities in Mortality and Morbidity in Pediatric Asthma Hospitalizations, 2007 to 2011. Acad Pediatr 2016;16:430-7. [Crossref] [PubMed]
- Moorman JE, Zahran H, Truman BI, et al. Current asthma prevalence - United States, 2006-2008. MMWR Suppl 2011;60:84-6.
- Ambient (outdoor) air pollution. (2022, December 19). World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health
- Khreis H, Kelly C, Tate J, et al. Exposure to traffic-related air pollution and risk of development of childhood asthma: A systematic review and meta-analysis. Environ Int 2017;100:1-31. [Crossref] [PubMed]
- Tiotiu AI, Novakova P, Nedeva D, et al. Impact of Air Pollution on Asthma Outcomes. Int J Environ Res Public Health 2020;17:6212. [Crossref] [PubMed]
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [Crossref] [PubMed]
- Marino E, Caruso M, Campagna D, et al. Impact of air quality on lung health: myth or reality? Ther Adv Chronic Dis 2015;6:286-98. [Crossref] [PubMed]
- Moelling K, Broecker F. Air Microbiome and Pollution: Composition and Potential Effects on Human Health, Including SARS Coronavirus Infection. J Environ Public Health 2020;2020:1646943. [Crossref] [PubMed]
- Shull JG, Pay MT, Lara Compte C, et al. Mapping IPF helps identify geographic regions at higher risk for disease development and potential triggers. Respirology 2021;26:352-9. [Crossref] [PubMed]
- Brugha R, Edmondson C, Davies JC. Outdoor air pollution and cystic fibrosis. Paediatr Respir Rev 2018;28:80-6. [Crossref] [PubMed]
- Simkovich SM, Goodman D, Roa C, et al. The health and social implications of household air pollution and respiratory diseases. NPJ Prim Care Respir Med 2019;29:12. [Crossref] [PubMed]
- Kurt OK, Zhang J, Pinkerton KE. Pulmonary health effects of air pollution. Curr Opin Pulm Med 2016;22:138-43. [Crossref] [PubMed]
- Loomis D, Huang W, Chen G. The International Agency for Research on Cancer (IARC) evaluation of the carcinogenicity of outdoor air pollution: focus on China. Chin J Cancer 2014;33:189-96. [Crossref] [PubMed]
- Raaschou-Nielsen O, Andersen ZJ, Beelen R, et al. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol 2013;14:813-22.
- Hamra GB, Guha N, Cohen A, et al. Outdoor PM exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect. 2014;122:906-911. [Crossref] [PubMed]
- Huang Y, Zhu M, Ji M, et al. Air Pollution, Genetic Factors, and the Risk of Lung Cancer: A Prospective Study in the UK Biobank. Am J Respir Crit Care Med 2021;204:817-25. Erratum in: Am J Respir Crit Care Med 2022;205:1254. [Crossref] [PubMed]
- Xue Y, Wang L, Zhang Y, et al. Air pollution: A culprit of lung cancer. J Hazard Mater 2022;434:128937. [Crossref] [PubMed]
- De Matteis S. Respiratory effects of air pollution: time to stop this deadly trajectory. Thorax 2023;78:635-6.
- Consonni D, Carugno M, De Matteis S, et al. Outdoor particulate matter (PM10) exposure and lung cancer risk in the EAGLE study. PLoS One 2018;13:e0203539. [Crossref] [PubMed]
- Liu C, Yang D, Liu Y, et al. The effect of ambient PM(2.5) exposure on survival of lung cancer patients after lobectomy. Environ Health 2023;22:23.