
The history of Japanese lung transplantation: the unique pathway to establishing the program and its initial success
Introduction
On October 16, 1997, organ transplantation from brain-dead donors (BDDs) was finally legalized in Japan when the “Organ Transplant Law” was enacted after an extensive national debate concerning the ethics of the notion of brain death as human death with regard to donation of organs for transplantation. The enactment of this law was an epoch-making event in the Japanese history of organ transplantation, developed through a very difficult and unusually long process not seen in other countries. Organ transplantation from BDDs was finally realized with the implementation of this law, albeit over than 15 years behind the US and European countries.
Fukuoka University joined the Japanese lung transplantation project in 2005 as a late-entrance institute to establish a lung transplant system in Kyushu, located in the southern region of Japan. We herein review the unique development history of Japanese lung transplantation, including the details of the Fukuoka University lung transplant story, and discuss why Japan’s lung transplantation results were able to reach a level comparable to those in other countries in such a relatively short period of time.
The history of the development of the Japanese Lung Transplant System
The Wada heart transplantation
The main cause of the delay in developing an organ transplantation system in Japan is believed to be the negative impact of the event known as the “Wada heart transplant” in 1968. This historic heart transplant was carried out just 1 year after the world’s first heart transplantation performed in South Africa, but it was too early for the unprepared Japanese public to understand and accept brain death as human death or the concept of organ transplantation medicine as a whole. The Wada heart transplant was technically successful, with the recipient surviving the perioperative period. However, Dr. Wada was later accused of murder by a citizen group who charged that the donor, a 20-year-old male, may not have been brain dead when the heart was removed (1). This transplant, which ultimately ended in failure (the recipient died on day 83 posttransplant), planted a deep-rooted sense of distrust toward the legitimacy of brain death and organ donation in Japanese society.
During the latter half of the 1980s, organ transplantation from BDDs became a reality in Europe and the US and was recognized as a breakthrough lifesaving treatment option for patients once considered “incurable” by conventional treatments other than organ transplantation. In Japan as well, strong and continuous efforts were made by aspiring transplant physicians and surgeons to realize organ transplant medicine. However, opponents, including religious, intellectual, academic, and even medical professionals, voiced their opposition to brain-dead organ donation. Under these circumstances, Japanese transplant advocates first needed to dispel the public distrust concerning transplant medicine.
In the process of enacting the “Japanese Organ Transplant Law”, there was also a deep-seated opposition in the national assembly to the idea that “brain death is human death”, so the enactment of the law was the result of a long and intense debate on bioethics. Since the “Japanese Organ Transplant Law” was enacted through such a complex process, those involved in transplant medicine had to perform organ transplantation under the strict gaze of society, even after transplantation from BDDs was legalized. Japanese organ transplant practitioners, including lung transplantation surgeons, developed their new transplant system in the face of severe social pressure and high expectations.
Japanese Organ Transplant Law 1997 and the revision of the Act in 2010
The Japanese Organ Transplant Law [1997] is similar to the “Uniform Determination of Death Act (UDDA) [1981]” in the US, which stipulates that “an irreversible cessation of the function of the entire brain, including the brainstem, constitutes death”. However, the Japanese Organ Transplant Law had an implication different from that of the UDDA, in that the judgment of brain death was valid only for individuals willing to donate their organs who had provided their written intent to donate their organs prior to death (via a Donor Card). In addition, the law stated that only persons ≥15 years old could legally express an intent to donate. Thus, organ donation from pediatric donors was impossible.
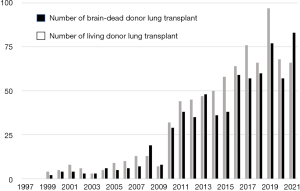
These strict conditions for the adoption of the law were put in place due to the long history of negative public opinion regarding brain death and organ donation. Since <10% of the population actually owned a donor card when the law was enacted, there was some concern that the number of organ donations would be trivial. Indeed, the number of brain-dead organ donations remained fewer than 10 cases per year in Japan during the first 10 years, and the average annual number of brain-dead donor lung transplantation (BDDLT) procedures was fewer than 5 cases from 1999 to 2007 (Figure 1). Despite this, the number of patients desiring organ (lung) transplantation continued to climb. Therefore, the waiting period for BDDLT soon exceeded 2 years, resulting in an increased number of deaths among wait-listed candidates (2).
Such a tragic situation led to an “increased number of living donor transplantation” procedures for organs for which living organ donation was deemed possible (e.g., lung or liver). Furthermore, the recognition that organ transplantation within Japan was difficult drove an unacceptable number of wait-listed patients to search abroad for potentially life-saving transplantation. In light of this situation, the Transplantation Society (TTS) released the Istanbul Declaration in 2008, calling on each country to strengthen its medical and political structures to save, the lives of its own citizens through transplantation.
In response to the TTS principles, the issue was discussed in 2009 in the Japanese Diet, and a bill for a revised Organ Transplant Act was passed and promulgated with some additional clauses. The revised and added clauses were as follows: (I) even if an individual’s intention is unclear, donation of their organs is possible with the family’s consent; (II) written consent to organ donation is not necessary, so donation from individuals under 15 years old is possible, but only with the family’s consent; and (III) priority allocation for family members of the donor is possible if they express their desire to donate their organs for this purpose before their death. Following these revisions of the law in 2010, the number of organ donations after brain death dramatically increased as the number of scenarios in which organs were donated by family agreement increased (Figure 1).
Development of the Japanese National Lung Transplant System
The Japanese National Lung Transplant System was established immediately after the enactment of the Japanese Transplant Law based on the following three philosophies: (I) an institutional certification system based on strict standards; (II) a rigorous central monitoring system for transplant results; and (III) a third-party review system to determine eligibility for patient registration. The purpose of these philosophies was to avoid any ethical deviations of individual members at various lung transplant institutes and to achieve a high quality of lung transplantations.
Certification system for lung transplant institute
Only institutes authorized by the National Council of Academic Societies for Lung Transplantation are permitted to perform BDDLT in Japan. The selection criteria are very strict with respect to the clinical, surgical, and ethical proficiency of the lung transplantation team. Initially, only four institutes (Tohoku, Kyoto, Osaka, and Okayama Universities) were selected as qualified facilities in 1997. Early transplant results from those four institutes satisfied international standards, so three additional institutes including Fukuoka University, were approved in 2005 after which three more institutes were approved, reaching a total of 10 institutes officially serving as lung transplant institutes in Japan as of 2022.
Rigorous national data monitoring for quality control
All lung transplant institutions are required to report detailed data of all patients regarding lung transplantation. In the event of death within 1 month after lung transplantation, or in case of particular incidents, the institutes are requested to report the detail to the national academic council board for lung transplantation. This information is then shared and discussed with all lung transplant institutes to increase the quality of lung transplantation.
Third-party review system for determining the eligibility for transplant indication
Candidates for BDDLT are evaluated for their indication for lung transplantation by a national evaluation board for lung transplant indication that is independent from each transplant institute. Lung transplant indications of individual candidates are basically screened according to the selection criteria of the International Society for Heart and Lung Transplantation (3). When the suitability for lung transplantation is deemed reasonable, the patients are approved for registration to the Japan Organ Transplant Network (JOTNW) waiting list for BDDLT.
The allocation of organs for transplantation is strictly performed in the order of registration date within the range of lung size, lymphocyte crossmatch results, and blood type compatibility. Adjusting the priorities based on the predicted prognosis or the severity of the disease, as is done in other programs in the US or Europe, is not practiced in Japan. If a patient on the waiting list becomes a top priority for a donor lung based on the above rules, the final decision to accept or reject the lung graft is entrusted to the patient, and if the patient decides not to accept, the organ will be then allocated to the patients with the next-highest priority.
General results of lung transplantation in Japan
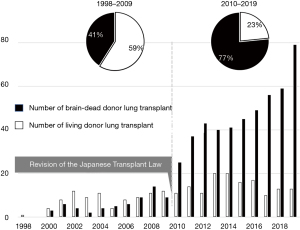
During the initial period after the Japanese lung transplant project began, transplants were performed mainly as living-donor lung transplantation (LDLT) rather than BDDLT, as the number of BDDs was tragically limited. In fact, the first lung transplantation was performed as an LDLT at Okayama University in 1998, whereas BDDLT was first performed in 2000. According to the first National Registry Report of 2008, a total 87 lung transplantations were performed as either BDDLT (n=30) or LDLT (n=57) during the first 9 years [1998–2006], so more than 60% of lung transplantations were performed as LDLT. The 5-year survival rates were reported as 57% and 77% for BDDLT and LDLT, respectively, indicating the outstanding results of LDLT in the early days of Japanese lung transplantation (4).
Japan was the only country in which LDLT accounted for the majority of transplants during the early period of lung transplantation development. Therefore, various advances in LDLT have been achieved in Japan, mainly by Professor Date’s group at Okayama and Kyoto Universities. Date et al. reported in their early study that LDLT is indicated for a variety of end-stage lung diseases, including primary pulmonary hypertension (PPH) (5). LDLT is typically performed as a bilateral lobar transplant using the left and right lower lobes from 2 individual living donors, and the total forced vital capacity (FVC) of the 2 lower lobe grafts should be more than 50% of the predicted FVC of the recipient (5). However, some patients are ineligible for LDLT because of a predicted insufficiency of the graft’s pulmonary function. To resolve this issue, various transplant procedures, such as sparing the native lobes, the right-to-left inversion transplant technique, or the combination of both procedures, have been applied (6-8). In addition, the segmental lung transplantation technique was recently developed to expand the lung transplant indications and to also include extremely young pediatric patients (9).
The number of BDDs increased after the revision of the Organ Transplant Law in 2010, which made organ donation possible with the family’s consent, even if the intent of the individual donor was unclear. As a result of this revision, the annual number of BDDLTs overtook the number of LDLTs after 2010 (Figure 2). By the end of 2022, a total of 752 BDDLTs and 284 LDLTs had been performed at 10 registered lung transplant institutes in Japan, and the 5-year survival rates of BDDLT and LDLT were reported to be 73.9% and 73.5%, respectively (10).
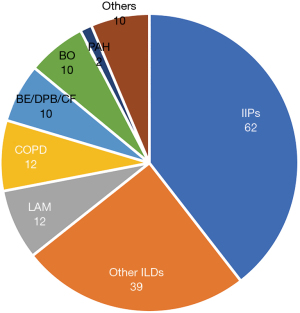
Lung transplantation in Japan differs significantly in a number of aspects from the in the US and European countries. Regarding the indication for lung transplantation, the most common primary disease for BDDLT in Japan is idiopathic interstitial pneumonia (IIP) (25.5%) and other interstitial lung diseases (ILD) (15.2%), followed by PPH (14.4%), lymphangioleiomyomatosis (LAM) (13.6%), and chronic obstructive lung disease (COPD) (8.2%) (10). In contrast, COPD (30.1%) is the most common indication for BDDLT in the ISHLT registry, followed by IPF (29.0%) and cystic fibrosis (14.2%), according to information from the most recent cohort of 2010 to 2018 (11). LDLT is indicated mainly for bronchiolitis obliterans (29.2%) in Japan, especially after hematopoietic stem cell transplantation, followed by IIPs (23.9%) and PPH (17.6%). Another obvious characteristic of lung transplantation in Japan is that many more procedures are performed for LAM and PPH than in Western countries (10).
Regarding the transplant procedure for BDDLT, single (unilateral) lung transplantation is selected more often than bilateral lung transplantation in Japan to maximize the number of transplantation procedures by sharing the relatively scarce donor resource. Indeed, 231 (51.7%) lung transplants were performed as single lung transplantation procedures among a total of 447 BDDLTs as of the end of 2018 (12).
Fukuoka University lung transplant program
In this section, the development of the Lung Transplant Program of Fukuoka University, a mid-sized but upcoming institute in Japan, is introduced to present the characteristics of a representative facility performing Japanese lung transplantation.
Development of lung transplantation in Kyushu
Kyushu is the southernmost major island of Japan, and Fukuoka is located in its northern part (Figure 3). Fukuoka University, along with Nagasaki University, which became a registered institute for lung transplantation at the same time as Fukuoka University in 2005, is responsible for delivering lung transplant-related medical attention in the Kyushu area. The Kyushu area had almost no experience in the field of lung transplant medicine until the aforementioned two institutes joined the lung transplant project. Thus, the first challenge undertaken at Fukuoka University was the education and enlightenment of both local citizens and pulmonary physicians concerning lung transplant medicine. We established the Kyushu Lung Transplant Study Group (KLTSG) to support the delivery of lung transplant healthcare among local medical professionals. The KLTSG consists of 11 university hospitals in Kyushu, including Fukuoka and Nagasaki University, as well as other major regional hospitals. First, the KLTSG helped raise awareness for and identify lung transplant candidates among patients with severe respiratory failure and supported their registration to the BDDLT waiting list when lung transplant was indicated. The number of patients registered to the waiting list increased steadily, especially after the revision of the Transplant Law in 2010. The listed patients received lung transplants sequentially after a long wait for a suitable donor.

The number of lung transplants at Fukuoka University increased after 2015, and subsequently, the number of posttransplant patients returning to their hometowns increased as well. The necessity and importance of a strong regional clinical network for appropriate posttransplant follow-up was finally realized in the Kyushu area (Figure 4). The KLTSG has since come to function as an effective patient care network helping recently returned patients following lung transplant. Currently, the KLTSG is acting as the backbone of a wide-ranging medical care network for lung transplantation medicine in Kyushu.

Patient background characteristics in the Fukuoka program
From 2005 to April 2022, a total of 157 candidates were registered on the BDDLT waiting list from Fukuoka University. The primary indications for lung transplantation were IIP in 62 (39.5%), other ILDs in 39 (24.8%), LAM in 12 (7.7%), COPD in 12 (7.7%), and bronchiectasis (BE)/diffuse panbronchiolitis (DPB)/cyctic fibrosis (CF) in 10 (6.4%). The most common indication for lung transplantation was IIP or other ILDs, accounting for 64.3% of candidates wait-listed for these diseases (Figure 5). The disease distribution of lung transplant candidates at Fukuoka University is similar to Japanese national data, which show that the majority of transplants are indicated for ILD. PPH is rarely found as a transplant indication at Fukuoka University, despite it being the third-most common indication according to Japanese national data (12).
Long waiting period and high waiting mortality
From 2005 to April 2022, a total of 51 lung transplantation procedures were performed, including 49 BDDLT and 2 LDLT, after being registered for BDDLT. An additional four patients underwent LDLT without registering for the BDDLT waiting list; thus, a total of 55 lung transplants, including 49 BDDLT and 6 LDLT, were performed at Fukuoka University. The details of the patients who underwent BDDLT or LDLT at Fukuoka University are shown in Table 1. The average waiting time for BDDLT was 752 days (approximately 2 years and 1 month) after listing. During this period, 64 (40.7%) wait-listed patients died from exacerbation of their underlying disease or other reasons without being able to receive BDD allocation. The mean waiting times for BDDLT and waiting mortality rates are similar to the Japanese national data. Patients with IIP or other ILDs in particular showed a relatively high waiting mortality of 52.4% at Fukuoka University.
Table 1
| Variables | Value |
|---|---|
| Number of candidates listed for lung transplant [2005–2022] | 157 |
| Transplanted/wait death | 55/64 |
| Lung transplant procedures | |
| BDDLT (n=49) | |
| Bilateral | 17 |
| Unilateral | 32 |
| LDLT (n=6) | |
| Bilateral (lobar) | 3 |
| Unilateral (lobar) | 3 |
| Organ transport for BDDLT (graft ischemic time), min | |
| Charter flight for organ transport, n (mean ± SD) | 3 (470.0±60.6) |
| Commercial, n (mean ± SD) | |
| Air | 20 (520.3±119.7) |
| Bullet train | 17 (473.1±83.4) |
| In house donor | 2 |
| Others (ambulance, etc.), n (mean ± SD) | 7 (322.3±29.8) |
| Post-transplant survival | |
| 3 years | 74.5% |
| 5 years | 60.1% |
BDDLT, brain-dead donor lung transplantation; LDLT, living-donor lung transplantation; SD, standard deviation.
Forty-two patients are currently waiting for BDDLT in our facility as of December 2022. The 3- and 5-year survival rates of 55 patients after lung transplantation with either BDDLT or LDLT were 74.5% and 60.1%, respectively.
No charter flights for donor-lung transport
The entire organ donation process including allocation-harvest-transport is completely controlled by the JOTNW. Fukuoka (Kyushu) is a major city in the southern part of Japan, located 1,000 km away from the metropolitan center of Tokyo, where the population is most concentrated and thus brain-dead donations are most likely. Other major cities of Osaka and Nagoya are located between Tokyo and Fukuoka, while Sapporo, the northernmost city, is located 2,100 km away from Fukuoka (Figure 3). Kyushu is geographically the most distant area from the center of Japan. Therefore, in terms of organ transport, Kyushu was thought to be the most remote area, particularly for organs vulnerable to ischemia, such as the lung.
However, the commercial transportation network between those five major cities is highly developed, with frequent air and rail (including the “shinkansen” high-speed bullet train) services available. These transportation systems are widely recognized for their rapid speed and precise time schedules. Furthermore, the above five cities function as transport hubs connecting neighboring cities. This particular situation in Japan is extremely advantageous in terms of managing brain-dead organ transportation.
At the beginning of the organ transplant project, the JOTNW arranged emergency charter flights to transport donor lungs to Fukuoka. However, after experiencing several cases of organ allocation, the JOTNW realized that it was possible to transport donor lungs with an acceptable ischemic time using commercial transportation networks, even when donor lungs were transported extremely long distances, e.g., from Hokkaido in the far north to Kyushu in the far south. In fact, in the case of Fukuoka University lung transplants, emergency charter flights were used only for the first three BDDLT cases, with donor lungs transported using commercial transportation services in all cases from the fourth case onward. The actual average ischemic times in our BDDLT cases in which donor lungs were transported by commercial transport—either air or train—were 520.3±119.7 and 473.1±83.4 min, respectively (Table 1). Japan is an unusual country where almost all types of organs (other than heart) for transplant are urgently transported using the commercial transport system. The use of commercial transport for organs is valuable for reducing the cost of organ transplants which may help further expand this new treatment option.
Conclusions
Japan is a unique country concerning the early development of organ transplantation as well as the currently implemented system. The characteristics of Japanese lung transplantation may be summarized as follows: (I) long and difficult history concerning the development of the organ transplant system; (II) still limited numbers of brain-dead organ (lung) donations; (III) long waiting times and high waiting mortality of wait-listed patients; (IV) a significant number of LDLT procedures to compensate for the limited number of BDDLT procedures; and (V) an extremely efficient organ allocation and transport system for transplants.
Despite the complicated situation of lung transplant in the country, the Japanese national lung transplant team has been able to achieve results comparable to those of other countries in a relatively short period of time since its implementation. While the precise reason for this success is debatable, even among those involved in lung transplantation in Japan, the following points are considered important: (I) Japanese lung transplant was started under intense pressure, where failure was unacceptable; (II) only high-level institutes were selected for involvement in this project; and (III) transplant results were managed securely by quality control at the national level.
In the near future, the number of brain-dead organ donations will hopefully increase to the international standard level, allowing lung transplantation procedures to become more reliable with an increased number of member institutes. It is hoped that the Japanese lung transplant system will be able to expand while maintaining excellent results.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Masaaki Sato) for the series “Why is the Outcome Good? Secrets of Lung Transplantation in Japan” published in Journal of Thoracic Disease. The article has undergone external peer review.
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1861/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1861/coif). The special series “Why is the Outcome Good? Secrets of Lung Transplantation in Japan” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Toshima H, Kawai C. Why is heart transplantation not performed in Japan? Refutation of Dr Yoshio Watanabe's arguments against heart transplantation. Jpn Heart J 1995;36:13-21. [Crossref] [PubMed]
- Japan Organ Transplant Network (JOTNW) / Organ Donation & Transplantation Data Book 2017 (Japanese). Available online: https://www.jotnw.or.jp/files/page/datas/databook/doc/11_lungtx.pdf
- Leard LE, Holm AM, Valapour M, et al. Consensus document for the selection of lung transplant candidates: An update from the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2021;40:1349-79. [Crossref] [PubMed]
- Bando T, Date H, Minami M, et al. First registry report: lung transplantation in Japan: The Japanese Society of Lung and Heart-Lung Transplantation. Gen Thorac Cardiovasc Surg 2008;56:17-21. [Crossref] [PubMed]
- Date H, Aoe M, Nagahiro I, et al. Living-donor lobar lung transplantation for various lung diseases. J Thorac Cardiovasc Surg 2003;126:476-81. [Crossref] [PubMed]
- Aoyama A, Chen F, Minakata K, et al. Sparing Native Upper Lobes in Living-Donor Lobar Lung Transplantation: Five Cases From a Single Center. Am J Transplant 2015;15:3202-7. [Crossref] [PubMed]
- Chen-Yoshikawa TF, Tanaka S, Yamada Y, et al. Intermediate outcomes of right-to-left inverted living-donor lobar lung transplantation. Eur J Cardiothorac Surg 2019;56:1046-53. [Crossref] [PubMed]
- Date H, Aoyama A, Hijiya K, et al. Outcomes of various transplant procedures (single, sparing, inverted) in living-donor lobar lung transplantation. J Thorac Cardiovasc Surg 2017;153:479-86. [Crossref] [PubMed]
- Nakajima D, Tanaka S, Ikeda T, et al. Living-donor segmental lung transplantation for pediatric patients. J Thorac Cardiovasc Surg 2023;165:2193-201. [Crossref] [PubMed]
- National registry of Japanese lung transplantation 2023 at the home page of Japanese Society of Lung and Heart-Lung Transplantation (Japanese). Available online: https://view.officeapps.live.com/op/view.aspx?src=http%3A%2F%2Fwww2.idac.tohoku.ac.jp%2Fdep%2Fsurg%2Fshinpai%2F_src%2F30889%2F%25E8%2582%25BA%25E7%25A7%25BB%25E6%25A4%258D%25E3%2583%25AC%25E3%2582%25B8%25E3%2582%25B9%25E3%2583%2588%25E3%2583%25AA%25E3%2583%25BC2023_ver.20230221.pptx&wdOrigin=BROWSELINK
- Perch M, Hayes D Jr, Cherikh WS, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-ninth adult lung transplantation report-2022; focus on lung transplant recipients with chronic obstructive pulmonary disease. J Heart Lung Transplant 2022;41:1335-47. [Crossref] [PubMed]
- Okada Y, Chida M, Nakajima J, et al. Current status of lung transplantation in Japan—report from Japanese lung transplant registry. J Vis Surg 2021;7:13. [Crossref]


