
Placental transmogrification of the lung: CT findings with pathologic correlation in six patients
Highlight box
Key findings
• Our study is the first to include all three computed tomography (CT) imaging patterns of placental transmogrification of the lung (PTL): bullous emphysema pattern, cystic lesion and nodule pattern, and solitary nodule pat-tern. And we also observed nodular interlobular septal thickening and clustered interstitial nodules and vascular dilatation.
What is known and what is new?
• It is known that PTL typically presents as cystic lesions confined to a unilateral lung. Pulmonary nodules with or without cystic lesions can also be seen.
• This study observed nodular interlobular septal thickening and clustered interstitial nodules and dilated pulmonary vasculatures of the involved lung.
What is the implication, and what should change now?
• This study highlights the importance of recognizing this condition as a possible cause of unilateral cystic lung lesions and suggest additional CT finding. Further research is needed to better understand the clinical implications of this condition.
Introduction
Placental transmogrification of the lung (PTL) is a rare lung disease that mostly appears as a cystic lesion. As suggested by its name, it is characterized by the formation of placental villi-like papillary structures in the lung parenchyma (1,2). Despite its morphological similarities to placental villi upon histopathologic examinations, this lesion does not contain any biological components of the placenta. Microscopically, these placental villi-like papillary structures are located in the lung interstitium that are lined by proliferating pneumocytes. The cores of these papillary structures are edematous or fibrotic interstitium consisting of proliferating blood vessels, lymphoid cells, smooth muscle, fat, and interstitial cells containing abundant clear cytoplasm (3). Although there are several hypotheses about the pathogenesis of PTL, its exact origin and pathogenesis remain unknown (4,5).
To date, there have only been several case reports describing the computed tomography (CT) findings of PTL. Radiologically, PTL can present as unilateral giant bullous disease or cystic lesion, and rarely as a solitary pulmonary nodule (6-8).
Thus, the purpose of this study was to report detailed CT findings of PTL in correlation with histopathologic findings from six patients treated in our institution. This manuscript is written following STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-733/rc).
Methods
Patient selection
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of Samsung Medical Center (No. 2021-12-034). The requirement for written consent was waived because of the retrospective nature of the study. We searched medical records using the term “placental transmogrification” from 2004 to 2021 and found six patients who were diagnosed with PTL via curative lung resection surgery or lung biopsy at Samsung Medical Center, a tertiary referral hospital located in Seoul, South Korea. Clinical data of these patients were retrospectively reviewed in terms of the following variables: age, sex, smoking history, the presence of the symptom, and treatment performed. Of the six cases, the imaging and pathologic features of two cases have previously been published in case reports (1,6).
Image acquisition
CT studies were performed using various helical CT scanners (mostly 16- to 64-MDCT scanners) obtained from several vendors. The scanning parameters were as follows: 120 kVp and 170–200 mA under automatic exposure control; beam width, 10–20 mm; and rotation time, 0.3–0.4 seconds. Image data were reconstructed using standard soft-tissue algorithms. Data were reformatted with a section thickness of 2.5–3.0 mm for transverse images. Both enhanced and unenhanced CT scans were obtained for four subjects. Iobitridol (300 mgI/mL; Xenetics, Guerbet) at a dose of 1.5 mL/kg of body weight was injected at an infusion rate of 3 mL/s using a power injector (MCT Plus, Medrad). The interval time between the initiation of contrast injection and scanning was 45 seconds. Reconstructed images were then sent directly to a Picture Archiving and Communication System (PACS, Centricity 3.0, GE Healthcare). Images were viewed on monitors with both mediastinal [width, 400 Hounsfield units (HU); level, 20 HU) and lung (width, 1,500 HU; level, −700 HU) window settings.
Image interpretation
The CT findings were reviewed by two radiologists with 2 and 15 years of thoracic CT interpretation experience. Decisions about CT findings were reached by consensus. The reviewed image features included the type and location of the lesion; the size, extent, and wall thickness of cystic lesions; the presence of consolidation; adjacent vascular dilatation; pulmonary nodules and their size; and interlobular septal thickening. The observed types of interlobular septal thickening were divided into smooth and nodular types. The attenuation of nodules and consolidation was also evaluated. The definitions of the lesions including cyst, bulla, bullous emphysema, consolidation, nodule, and interlobular septal thickening followed those contained in the glossary of terms for thoracic imaging compiled by Fleischner Society (9). Vascular dilatation and interlobular septal thickening were compared to those of the normal vasculature and interstitium in the contralateral uninvolved lung at the same level.
Statistical analysis
Statistical analysis was performed using SPSS (version 25.0). The presentation of continuous variables included the mean and range, while categorical variables were expressed as counts and percentages (%).
Results
Clinical findings of PTL
The clinical features of the six cases of PTL are summarized in Table 1. All six patients were asymptomatic. For all patients, PTL was detected as an incidental finding on their chest X-ray or chest CT performed as part of routine health checkups. The median age at the time of diagnosis was 42 years (range, 27–65 years). Five patients were men and one patient was a woman. Two patients were current smokers, two patients were ex-smokers, and two patients were never smokers. Out of the total number of patients, tissue confirmation was carried out through biopsy in three cases, one of which used CT-guided percutaneous core needle biopsy whereas the other two used transbronchial lung biopsy. Pathologic reports were suggestive of PTL. Three patients underwent surgical resection due to suspicion of lung cancer. All patients recovered without recurrence or complications.
Table 1
| Variable | N (%) or median [range] |
|---|---|
| Age, years | 42 [27–65] |
| Sex | |
| Male | 5 (83.3) |
| Female | 1 (16.6) |
| Smoking history | |
| Current smoker | 2 (33.3) |
| Ex-smoker | 2 (33.3) |
| Never smoker | 2 (33.3) |
| Symptoms | |
| Yes | 0 (0.0) |
| No | 6 (100.0) |
| Surgical treatment | |
| Yes | 3 (50.0) |
| No | 3 (50.0) |
CT findings of PTL
All the subjects had lesions in a unilateral lung. Among these, four subjects had cystic lesions on CT scans. One subject had both a nodule and a cystic lesion, while another subject had a solitary pulmonary nodule.
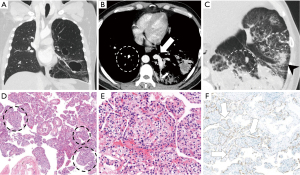
In the four subjects with cystic lesions, the cyst sizes varied from small, subcentimeter-sized thin-walled cysts to large cysts exceeding 10 cm. Three subjects had both small cysts and large cysts simultaneously, which led to air-trapping, hyperinflation of the affected lung, and mediastinal shifting to the contralateral side (Figure 1).
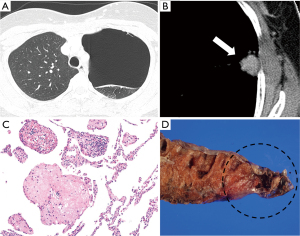
In the subject with both nodules and cysts, the cystic lesion appeared as a large bulla with an extent of 11 cm in the largest diameter. The nodule was well-defined, and it had the diameter of 1.9 cm. The nodule appears to be well-enhanced and measures 73 HU in post-contrast CT image, which is an increase of 15 HU compared to the pre-contrast image (Figure 2). Finally, the last case showed only a solitary pulmonary nodule with a well-defined lobulated margin. The mass appeared as soft tissue attenuation, and no post-contrast images were taken (Figure 3).
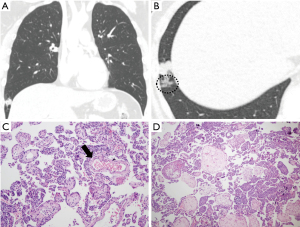
We also observed that all six cases exhibited nodular interlobular septal thickening and clustered interstitial nodules. Even the solitary pulmonary nodular pattern had perilesional interstitial nodules around the main nodule (Figure 3). The tiny nodules had a beaded appearance along the bronchovascular bundle and interlobular septum, as can be seen in Figure 1. In four of the six cases, these nodules merged into dense nodular consolidation (Figure 4). Further, three cases presented dilated pulmonary vasculature of the affected lung, including pulmonary arteries and veins (Figure 1). The radiological features of the six patients with PTL are summarized in Table 2. The clinical and radiological features of each patient are summarized in Table 3.
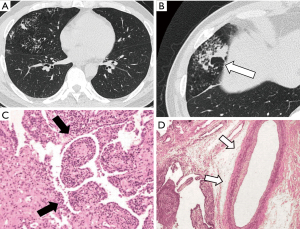
Table 2
| Image findings | N (%) |
|---|---|
| Location | |
| Right | 2 (33.3) |
| Left | 4 (66.6) |
| Both | 0 (0.0) |
| Cystic lesion | |
| Yes | 5 (83.3) |
| No | 1 (16.6) |
| Nodule | |
| Yes | 2 (33.3) |
| No | 4 (66.6) |
| Consolidation | |
| Yes | 4 (66.6) |
| No | 2 (33.3) |
| Dilated vasculature | |
| Yes | 3 (50.0) |
| No | 3 (50.0) |
| Nodular interlobular septal thickening and clustered interstitial nodules | |
| Yes | 6 (100.0) |
| No | 0 (0.0) |
Table 3
| Case No. | Age (years) | Sex | Symptoms | Site | Treatment | Cystic lesion | Nodule | Dilated vasculature | Nodular interlobular septal thickening and interstitial nodules |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 46 | Male | No | RML | RML lobectomy | Yes | No | No | Yes |
| 2 | 32 | Female | No | LUL | LUL lobectomy | Yes | Yes | Yes | Yes |
| 3 | 46 | Male | No | Left | Yes | No | Yes | Yes | |
| 4 | 27 | Male | No | Left | Yes | No | Yes | Yes | |
| 5 | 65 | Male | No | LLL, LUL | LUL lobectomy | Yes | No | No | Yes |
| 6 | 38 | Male | No | RLL | No | Yes | No | Yes |
PTL, placental transmogrification of the lung; RML, right middle lobe; LUL, left upper lobe; LLL, left lower lobe; RLL, right lower lobe.
Pathologic findings of PTL
At low magnification, numerous nodular structures were visible, which resembled villi of the placenta. Immunohistochemistry analysis revealed that the lining of these nodules exhibited TTF-1 expression, a marker commonly associated with respiratory epithelial cells. The inner structure was proliferated lung interstitium (Figure 1).
Histiocytes and macrophages with a clear cytoplasm were present within the lining of the pneumocyst. In some cases, capillaries grew into the proliferated interstitium, with adipose tissue suggestive of fatty changes around them. In the area that was identified as a large bulla on the CT scan, the airway was stretched and appeared similar to emphysema. As a result, in one case, emphysema was initially diagnosed in the first biopsy, while in repeat biopsy, it was confirmed to be PTL (Figure 2).
Discussion
PTL is a rare pathological condition that affects the lungs. It is characterized by the presence of papillary structures in the lung parenchyma that resemble the chorionic villi of the placenta. It typically appears as a bullous and cystic lesion involving unilateral lung.
In the existing literature, there are currently fewer than 40 papers about PTL. Kim et al. (6) suggested that the image findings of PTL can be classified into three patterns: The most common pattern is the bullous emphysema pattern, followed by the thin-walled cystic lesion and nodule pattern. The third and rarest pattern is the solitary nodule pattern. In our study, we observed all three patterns of PTL, and our study is the first study to include all three patterns.
Previous papers have also reported cases with other radiologic findings, with specific examples including consolidative lesion with bronchiectasis (10) and progressive unilateral interstitial lung disease with micronodules and cysts (11). Cases with pneumothorax have also been reported (12,13).
In addition to the typical findings of cystic lesion and nodule, we observed two findings commonly found in many cases: the inclusion of nodular interlobular septal thickening and clustered interstitial nodules and vascular dilatation of the affected lung. Nodular interlobular septal thickening and clustered interstitial nodules were found in all six patients in our study. Similarly, a previously published case report mentioned the presence of cystic and micronodular interstitial lung disease (11).
There are various hypotheses regarding the pathogenesis of PTL, but its etiology remains unclear. Fidler et al. (2) proposed that PTL could arise from bullous emphysema, while Theile et al. (14) suggested that it may be linked to lymphatic or vascular abnormalities, and Xu et al. (4) theorized that PTL is associated with pulmonary hamartoma, assuming that the villous structure is an invagination of fibroadipose tissue. Recently, Cavazza et al. (3) suggested that interstitial clear cell proliferation is a primary pathologic event in PTL where the emphysema-like cystic change is simply a secondary phenomenon. There were also a few papers that analyzed the immunohistochemistry findings of PTL. Interstitial clear cells were positive for CD-10 and, focally, for vimentin in one study (3) and focal positivity for vimentin in another study (2). In both studies, the ultrastructural examination did not identify any distinctive line of cellular differentiation.
Our hypothesis proposes that the interstitial proliferation of countless nodules resembling placental villi in pathologic specimen may account for the interstitial nodules visualized on CT scans, which can aggregate and manifest as consolidation. We postulate that the thickening of the interstitium may lead to ischemia, which triggers vascular remodeling and proliferation, eventually resulting in the dilation of larger vessels observed on CT scans.
Because PTL can appear as a large bullous cystic lesion and/or solitary pulmonary nodule on CT, its differential diagnoses may include bullous emphysema, and especially idiopathic giant bullous emphysema (also known as vanishing lung syndrome); congenital pulmonary airway malformation (CPAM) with accompanied bronchopneumonia; and hamartoma or lung cancer if it is presented as a solitary pulmonary nodule (1,6). If extensive consolidation is present, PTL may be mistaken for pneumonia (15), but it can be differentiated from infectious conditions by the absence or minimal presence of symptoms as well as the lack of changes over time.
The results of our study suggest that, when there is a large bullous cystic lesion confined to one lung, either with or without a pulmonary nodule, PTL can be considered one of the differential diagnoses.
There are limitations to our study, including a retrospective design and a small sample size of pathologically confirmed PTL, which is partially attributable to the rarity of this disease. To validate our results, there is a need for further studies with a larger sample size and multi-center comparison.
Conclusions
PTL typically manifests as a cystic lesion that is limited to a single lung, and it can also appear as a pulmonary nodule with or without an associated cystic lesion. The presence of nodular interlobular septal thickening and clustered interstitial nodules which may merge into dense nodular consolidation, and dilated pulmonary vasculature could serve as additional radiologic diagnostic indicators for PTL.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-733/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-733/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-733/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-733/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of Samsung Medical Center (No. 2021-12-034). The requirement for written consent was waived because of the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Park ES, Han J, Koh WJ, et al. Placental Transmogrification of the Lung: A Brief Case Report. Korean J Pathol 2008;42:308-10.
- Fidler ME, Koomen M, Sebek B, et al. Placental transmogrification of the lung, a histologic variant of giant bullous emphysema. Clinicopathological study of three further cases. Am J Surg Pathol 1995;19:563-70. [Crossref] [PubMed]
- Cavazza A, Lantuejoul S, Sartori G, et al. Placental transmogrification of the lung: clinicopathologic, immunohistochemical and molecular study of two cases, with particular emphasis on the interstitial clear cells. Hum Pathol 2004;35:517-21. [Crossref] [PubMed]
- Xu R, Murray M, Jagirdar J, et al. Placental transmogrification of the lung is a histologic pattern frequently associated with pulmonary fibrochondromatous hamartoma. Arch Pathol Lab Med 2002;126:562-6. [Crossref] [PubMed]
- Hochholzer L, Moran CA, Koss MN. Pulmonary lipomatosis: a variant of placental transmogrification. Mod Pathol 1997;10:846-9. [PubMed]
- Kim JW, Park IH, Kwon W, et al. Placental transmogrification of the lung. Korean J Radiol 2013;14:977-80. [Crossref] [PubMed]
- Ferretti GR, Kocier M, Moro-Sibilot D, et al. Placental transmogrification of the lung: CT-pathologic correlation of a rare pulmonary nodule. AJR Am J Roentgenol 2004;183:99-101. [Crossref] [PubMed]
- Horsley WS, Gal AA, Mansour KA. Unilateral giant bullous emphysema with placental transmogrification of the lung. Ann Thorac Surg 1997;64:226-8. [Crossref] [PubMed]
- Hansell DM, Bankier AA, MacMahon H, et al. Fleischner Society: glossary of terms for thoracic imaging. Radiology 2008;246:697-722. [Crossref] [PubMed]
- Kang MK, Kang DK, Hwang YH, et al. Placental transmogrification of the lung presenting as a consolidative lesion with bronchiectasis. Thorac Cancer 2019;10:1644-7. [Crossref] [PubMed]
- Lohbrunner A, Bitton L, Remy J, et al. Lung placental transmogrification presenting as progressive unilateral interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis 2017;34:188-90. [PubMed]
- Hamad AM, Nosseir MM, Alorainy SM. Unilateral Giant Bullae: Pulmonary Placental Transmogrification Should Be Kept in Mind: Case Reports. J Chest Surg 2021;54:416-8. [Crossref] [PubMed]
- Dunning K, Chen S, Aksade A, et al. Placental transmogrification of the lung presenting as tension pneumothorax: case report with review of literature. J Thorac Cardiovasc Surg 2008;136:778-80, 780.e1-8.
- Theile A, Wex P, Müller KM. Placentoid malformation of the lung as differential diagnosis of localized emphysema. Pneumologie 1997;51:550-4. [PubMed]
- Horiuchi K, Asakura T, Sakaguchi S, et al. Placental transmogrification of the lung masquerading as difficult-to-treat pneumonia. QJM 2020;113:213-4. [PubMed]


