
Surgical stabilization of multiple rib fractures in an Asian population: a systematic review and meta-analysis
Highlight box
Key findings
• Surgical stabilization of multiple rib fractures resulted in shorter duration of mechanical ventilation (DMV), intensive care unit length of stay (ICU LOS) and hospital length of stay (HLOS), lower risk for atelectasis and pneumonia, and lower pain scores after 4 weeks;
• There were no significant differences between treatment groups for risk of mortality.
What is known and what is new?
• Surgical stabilization of flail chest rib fractures was proven to be effective in previous meta-analyses. However, there is no consensus on the effectiveness of surgical stabilization among patients with multiple non-flail rib fractures, especially in Asians;
• This study provides up-to-date evidence on the treatment of multiple non-flail rib fractures among Asians.
What is the implication, and what should change now?
• Surgical stabilization results in better clinical outcomes than non-operative treatment in a cohort of Asian patients with multiple non-flail rib fractures. Therefore, surgical stabilization may be considered as an effective and safe treatment for patients with multiple non-flail rib fractures.
Introduction
Background
Chest trauma accounts for 25% of all trauma-induced mortality (1). Rib fractures are commonly encountered in blunt chest trauma and are associated with significant mortality and morbidity. The global annual prevalence of sternal and rib fractures was estimated to be 1.98 million in 2019. The number of cases is much higher in males (1.24 million) than in females (741 thousand) (2). The severity of the injury may be accompanied by complications such as pneumothorax, hemothorax, pulmonary contusion, pneumonia, other critical organ damage, and posttraumatic mortality (3). Studies have suggested that the number of rib fractures is correlated with an increased risk for pulmonary complications and mortality (4,5).
Li et al. [2020] (6) defined a flail chest as having more than three consecutive rib fractures on one side of the chest with at least two fracture lines per rib. This is considered an inherently unstable fracture pattern with high morbidity and mortality. Patients with multiple rib fractures but who do not meet the strict definition of “flail” may still have significant chest wall instability. For the purposes of this study, we followed the Chest Wall Injury Society (CWIS) guidelines for significant non-flail chest wall injury in patients with multiple rib fractures having three or more consecutive ribs that have a bicortical fracture displacements (7).
Management and treatment of rib fractures include supportive treatment to alleviate pain including systemic and local analgesics, procedures such as tube thoracostomy if pneumothorax or hemothorax present, airway clearance maneuvers, mechanical ventilation, and/or surgical treatment. Unstable rib fractures may impair respiration in many ways. Chest wall instability can reduce motion during respiration even causing paradoxical inspiratory collapse. This can cause severe pain and intercostal muscle spasms impeding both ventilation and cough effectiveness. Further, a study has shown that unstable rib fractures lead to higher incidence of retained hemothorax which will further impair respiration (8). This is often compounded by pulmonary contusions and thus chest wall instability hobbles the natural compensatory mechanisms and respiratory failure often ensures. For this reason, many surgeons find that surgical stabilization of rib fractures (SSRF) is the key to treating unstable rib fracture patterns such as flail chest. Chest wall stabilization is usually performed with surgical plate and screw fixation, and has especially been shown effective in patients with flail chest (9). There are various commercially produced plate-and-screw systems and designs available, and other types of fixation options exist including rib clips (or “struts”) and intramedullary rods. Other methods have been described using instruments not designed specifically for SSRF including Kirschner wires in a variety of techniques (10,11).
Rationale and knowledge gap
In recent years, the efficacy of SSRF has been investigated mostly for flail chest rib fracture patterns. Studies on patients with non-flail rib fractures patterns are limited and often performed in the Western population. Pieracci et al. [2020] (7) conducted a multicenter, prospective randomized controlled trial (RCT) of SSRF vs. conservative management for patients with non-flail fracture patterns and found highly favorable results, similar to the studies published on SSRF for flail, but this was primarily a non-Asian population study. However, in China, a retrospective study by Zhang et al. [2019] (3) examined the efficacy of SSRF for severe non-flail rib fracture patients. The study highlighted rib fixation as an effective treatment modality and provided a better quality of life (QoL) after surgery for non-flail rib fracture patients. Similarly, studies on flail chest rib fractures have shown that SSRF is effective and convenient, with improved morbidity outcomes (12-16). Investigations conducted in Japan displayed similar results, which revealed that SSRF is effective and beneficial regardless of the presence of flail chest (17,18). A systematic review and meta-analysis performed by Liang et al. in 2019 supported SSRF rather than nonoperative treatment for multiple rib fractures (19). The results indicated a shorter duration of mechanical ventilation (DMV) and decreased hospital and intensive care unit (ICU) lengths of stay for the operative group. In a prospective study by Granhed et al. in 2014, SSRF for flail chest or multiple rib fracture patients was reported to be cost-effective compared to patients who were treated nonoperatively (20). In contrast, a recent study from The Netherlands compared rib fixation to nonoperative treatment in multiple rib fracture with nonflail component. They observed an increase in hospital length of stay (HLOS) of 4.9 days and a decrease in QoL among patients who had rib fixation compared to non-operative treatment. The authors did not recommend rib fixation as the standard of care for multiple rib fractures (21).
Given the conflicting evidence presented on the efficacy of surgical fixation of rib fractures, including unstable non-flail fracture patterns, it is imperative to better recognize the clinical aspects of operative treatment for a specific subgroup, such as the Asian population. To date, most of the systematic review and meta-analysis studies on rib fracture surgery have been derived from Western countries. The primary studies adopted are based on Western populations. Asia, which accounts for most of the world’s population, has lacked corresponding systematic research. Furthermore, the practice of SSRF is not that common in Asia compared to many Western nations mainly because of a lack of consensus on its effectiveness, especially in non-flail chest patients. On the other hand, clinical practice guidelines and consensus statements from Asian countries put higher weight on evidence derived from populations whose characteristics are similar to them. This is because health systems, practice patterns and procedures, as well as cultural and constitutional differences exist between Asian and Western countries. Therefore, a comprehensive understanding of the outcomes and benefits of SSRF vs. nonoperative treatment fixation particularly among Asian populations is essential for health care providers in formulating specific modalities for treatment.
Objective
This meta-analysis aims to synthesize the current evidence for the clinical effectiveness and safety of SSRF in Asian patients with multiple non-flail rib fractures. The null hypothesis is that there is no significant difference in clinical effectiveness and safety between operative and non-operative treatment of multiple non-flail rib fractures. The alternative hypothesis is that SSRF would be as safe as or more effective than nonoperative treatment.
Since RCTs are lacking, this systematic review and meta-analysis was based mostly on observational studies. The Meta-analysis of Observational Studies in Epidemiology (MOOSE) criteria were used to synthesize evidence on the effect of SSRF in skeletally mature Asian patients with multiple non-flail multiple rib fractures on the following outcomes: DMV, respiratory complications, need for tracheostomy, postprocedural pain score, mortality, intensive care unit length of stay (ICU LOS), HLOS, and QoL. We present this article in accordance with the MOOSE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1117/rc).
Methods
Literature search
This systematic search of electronic databases [MEDLINE, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), and Cochrane Database of Systematic Reviews] was performed in July 2022 by a medical writer (Abella SP). The search strategy was conducted using the keywords multiple rib fracture and surgical fixation. The search term used was as follows: (multiple AND rib fractur*) OR (“non flail” OR “not flail” OR “non-flail” OR “nonflail” OR “without flail”). A broad search strategy was utilized so that publications that did not use the terms multiple rib fracture or surgical fixation were still captured and assessed for inclusion. Reference lists of obtained articles were also searched for relevant studies.
Identification and selection of studies
The search was conducted to identify trials and observational studies comparing the outcomes of SSRF vs. nonoperative treatment of multiple rib fractures in skeletally mature Asian populations with non-flail rib fractures. Study data from primary surgical centers as well as database analyses were included in the review.
The following patient-intervention-comparator-outcome-time-source (PICOTS) framework was used to formulate the search strategies in identifying studies. Patients: the patients were skeletally mature Asian patients diagnosed with multiple severe, non-flail rib fractures. Studies with interventions that included both flail and non-flail rib injuries were included. Some studies evaluated only non-flail patients and mixed cohort (n=5) participants with or without flail chest. Therefore, not all patients included in this analysis had non-flail rib fractures patterns. We defined multiple non-flail rib fractures as three or more consecutive rib fractures, each having a single bicortical fracture line and possible clear displacements. However, other authors defined it as greater than or equal to three rib fractures without further detail. In contrast, a flail chest, which has fractures or broken ends in two or more locations per rib, may result in independent movement of that segment of chest wall during breathing. Intervention: SSRF was the intervention of focus in the study. All kinds of fixation devices as well as surgical approaches were considered. Comparators: the comparator group was conservative management or any kind of nonoperative care. Outcomes: the DMV was the primary outcome. Respiratory complications, need for tracheostomy, postprocedural pain score, mortality, ICU LOS, HLOS, and QoL were considered secondary outcomes. In the included studies, they reported pneumonia, pleural effusion, hemothorax, atelectasis, pneumothorax, and pleural empyema as part of respiratory complications. Time: no length of follow-up was excluded in posttreatment evaluation. Study type: RCTs, retrospective and prospective observational clinical trials, cohort studies, case-control studies, registry studies, economic studies (budget impact and cost-effective analyses), and case series (comparative only) published until June 30, 2022 were considered for inclusion. Posters and conference abstracts with no full texts were excluded. No relevant unpublished study or preprint articles were found. Additionally, no relevant studies written in non-English language were found. If the same authors published more than one study based on the same sample of patients, only the study of the most recent publication was selected.
Study selection procedure and data extraction
Parallel and blinded screening of titles and abstracts and selection of full-text articles were performed by two authors (Salonga R and Abella SP). Any disagreements were settled by discussion and subsequent consensus with all authors. Figure 1 illustrates the study selection process as a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA ) flow diagram.
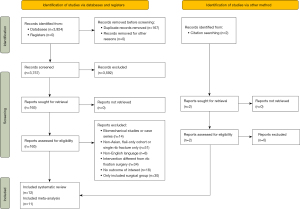
The journal citation, study objectives, study design and data source, intervention, study population, sample size, follow-up duration, primary and secondary outcome measures, and author’s conclusions were prespecified data extracted from the included studies and coded into a Microsoft Excel spreadsheet. The primary and secondary outcomes were identified as important data based on the clinical judgment of the primary author. Data collection was performed in parallel and blinded by two authors (Salonga R and Abella SP). Inconsistencies between the two authors were less than <5% of all data points and were resolved through consensus with all authors. Authors of the included studies were contacted through email if information from any study needed clarification.
Risk of bias (quality) assessment
The quality of evidence of the included studies related to safety and clinical effectiveness was assessed with the principles and methodology of the Evidence-Based Practice Guidelines (22). Study appraisal was performed blindly by two authors based on study design, methodology, and level of evidence. Any discordance was settled by consensus with all authors. All included studies were given levels I–III based on design and then ranked as either low-, good, or high-quality evidence using the Evidence Level and Quality Guide from John Hopkins Nursing Evidence-Based Practice (23). Evidence levels are classified as Level I (experimental study, RCT, systematic review of RCTs, with or without meta-analysis), Level II (quasiexperimental study, systematic review of a combination of RCTs and quasiexperimental, or quasiexperimental studies only, with or without meta-analysis), or Level III (nonexperimental study, systematic review of a combination of RCTs, quasiexperimental and nonexperimental studies, or nonexperimental studies only, with or without meta-analysis, qualitative study or systematic review with or without a meta-synthesis). Quality was classified as high (consistent, generalizable results; sufficient sample size for the study design; adequate control; definitive conclusions), good (reasonably consistent results; sufficient sample size for the study design; some control, fairly definitive conclusions), or low (little evidence with inconsistent results; insufficient sample size for the study design). Studies with no or minimal control for confounding were also classified as low. Reporting bias was not a concern since there were no missing results in the included studies.
Data synthesis
A meta-analysis was performed for an outcome that was reported in at least two different studies. A narrative summarization and qualitative synthesis were performed for some studies that were not appropriate for meta-analysis or effect estimation since mean values with standard deviations (SDs) cannot be extrapolated.
Statistical analysis
The inverse variance random effects model (REM) with DerSimonian Laird was applied for continuous outcome measures. The mean and SD were derived from means with P values and medians with range or interquartile ranges of individual studies.
For dichotomous outcomes, pooled risk ratios (RRs) were estimated using the Mantel-Haenszel REM. Inverse variance REMs were used for the pooled summary statistics for each outcome in the SSRF and nonoperative groups. Confidence intervals (CIs) of 95% were reported for all effect sizes. For estimation of statistical heterogeneity (α=0.05), the χ2 test was used and quantified using I2 statistics with a P value of 0.10. Sensitivity and subgroup analyses were not performed due to the limited number of studies included. Data management and analysis were performed using RevMan 5.0. Funnel plots were not created since there were fewer than 10 studies per outcome.
Results
Characteristics of the included studies
A total of 12 studies were included in the systematic review, and 11 were included in the meta-analysis. The studies described the outcomes of 2,440 patients, of which 1,015 and 1,425 were treated operatively and non-operatively, respectively. The mean age of the patients ranged from 38 to 60 years. Follow-up (months) ranged from 1 to 24 months. Five studies did not mention the follow-up period (18,24-27). All included studies focused on SSRF and compared the outcomes with the nonoperative group. A non-flail rib was defined as having three or more consecutive rib fractures in 4 studies (3,6,28,29), more than or equal to two rib fractures in 3 studies (14,18,24), and more than or equal to four rib fractures in 2 studies (30,31). Three studies did not define non-flail rib fracture injury (25-27).
Out of the 1,015 surgical patients, 73% (740/1,015) were identified as having a non-flail fracture pattern, and for 14% (143/1,015) it was unknown. In the nonoperative group, the proportions of identified non-flail fracture patterns and unknown patients were 58% (831/1,425) and 17% (239/1,425), respectively, as reported in Table 1. This meta-analysis included one single-center RCT, one case series and ten cohort studies. Studies were published between 2011 and 2020. The majority of the studies were conducted in China (n=8), two were conducted in Japan, one was conducted in Taiwan, China, and one was conducted in India.
Table 1
| Study | Year | Study design | Country/region | No. of patients | Mean age (years) | Follow-up (months) | Definition of non-flail rib (No. of ribs) | Surgical cohort |
Non-surgical cohort | Outcome† | Level and quality of evidence | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Of which: non-flail | N | Of which: non-flail | |||||||||||
| Khandelwal et al. | 2011 | Cohort study | India | 61 | 47.38 | NR | 2–3 | 32 | 94% (30/32) | 29 | NR | B, H | III, good | |
| Wada et al. | 2015 | Cohort study | Japan | 420 | NR | NR | NR | 84 | 12% (10/84) | 336 | 14% (48/336) | D, E, F | III, good | |
| Wu et al. | 2015 | Single-center RCT | China | 164 | 51 | 2 | ≥3 | 75 | 59% (44/75) | 89 | 61% (54/89) | A, B, C, D, E, F, G | I, good | |
| Qiu et al. | 2016 | Cohort study | China | 124 | 38 | 6 | ≥2 | 65 | 100% | 59 | 100% | B, C, D, F, H | III, good | |
| Tarng et al. | 2016 | Case series | Taiwan, China | 65 | 56 | 24 | >4 | 12 | 25% (3/12) | 53 | NR | A, D, E, F, G | III, low | |
| Uchida et al. | 2017 | Cohort study | Japan | 20 | 60 | NR | >2 | 10 | 40% (4/10) | 10 | NR | A, C, D, E, G | III, low | |
| Liu et al. | 2018 | Cohort study | China | 110 | NR | NR | NR | 59 | 83% (49/59) | 51 | 37% (19/51) | C, F, G | III, good | |
| Jiang et al. | 2019 | Cohort study | China | 167 | 55 | 3 | ≥4 | 75 | NR | 92 | NR | A, C, D, F | III, good | |
| Xiong et al. | 2019 | Cohort study | China | 123 | 47 | NR | NR | 68 | NR | 55 | NR | B, C, F, F | III, good | |
| Zhang et al. | 2019 | Cohort study | China | 78 | 50 | 6 | ≥3 | 39 | 100% | 39 | 100% | B, D, E | III, good | |
| Li et al. | 2020 | Cohort study | China | 98 | 55 | 12 | ≥3 | 66 | 100% | 32 | 100% | B, D, F, H | II, good | |
| Xiao et al. | 2020 | Cohort study | China | 1,010 | 50 | 1 | ≥3 | 430 | 100% | 580 | 100% | A, C, D, F, G | III, good | |
†, the contribution of each study is shown with letters A–H indicative of each outcome type. A, duration of mechanical ventilation; B, pain scores; C, respiratory complications; D, mortality; E, tracheotomy; F, length of hospital stay; G, length of ICU stay; H, functional outcomes. NR, not reported; ICU, intensive care unit.
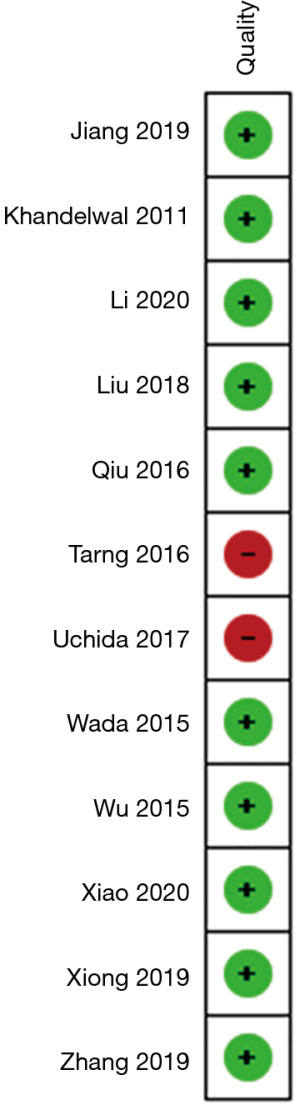
The studies were analyzed and classified according to the John Hopkins Nursing Evidence-based Practice Level and Quality guidelines (23) (Figure 2). Ten of the 12 studies were graded to be of good quality, with most having level III evidence (see Table 1).
Meta-analysis
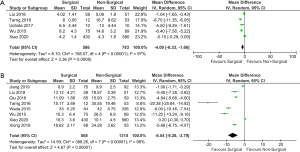
DMV
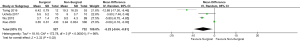
A total of 1,259 patients were included in the four studies that reported DMV in this meta-analysis. Forty-two percent (n=527) were treated with SSRF (18,28,29,31). Two of these studies reported significantly lower DMV among patients who received surgical fixation (28,31). The overall pooled mean difference (MD) demonstrated significantly lower DMV in the operative group [MD: –5.23 (95% CI: –9.64 to –0.81), P=0.02]. High heterogeneity was observed (I2=98%) (Figure 3).
QoL: posttreatment pain score
The posttreatment pain score was reported as part of QoL. The pooled analysis for the pain endpoint included two studies at four weeks posttreatment and showed a significant difference [standard mean difference (SMD): –2.24 (95% CI: –3.18 to –1.31), P<0.00001]. This suggests a lower pain score for patients who were surgically fixated compared to nonoperative treatment. High heterogeneity (I2=85%) was reported (Figure 4). Due to insufficient data, a meta-analysis for pain at other follow-up time points could not be performed (3,28).

Three other studies reported on pain (6,14,23). However, these were not included due to differences in assessment reporting period and unreported mean or SD. Li et al. [2020] (6) reported no significant differences (P>0.05) in visual analog pain scale indices (8 vs. 8). However, during the follow-up period, patients who underwent SSRF experienced a shorter duration of pain than those who had nonoperative management (1.0 vs. 1.9 months). Qiu et al. [2016] (14) assessed pain using a visual analog pain scale 2 months after intervention and observed less pain in the surgical fixation group than in the nonoperative group (1.45±0.65 and 4.50±1.05, P=0.003). A study from Khandelwal et al. [2011] (24) reported lower numerical pain scores in the SSRF group than in the nonoperative group on days 15 (2.31 vs. 5.96) and 30 (1.12 vs. 4.50) but higher scores on day 5 (9.15 vs. 6.25) posttreatment.
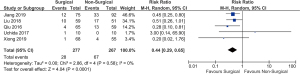
Pneumonia
Four studies that measured the risk of pneumonia were included in this meta-analysis (18,28-30). Three showed a significantly lower risk of pneumonia among surgically fixated patients (18,28,30). The pooled analysis of the four studies demonstrated a significantly reduced risk of developing pneumonia in SSRF patients compared to nonoperative group, with a RR 0.46 (95% CI: 0.23 to 0.95, P=0.04). High heterogeneity was also observed (I2=79%) (Figure 5). An analysis of the pneumonia follow-up period was not conducted due to insufficient data.
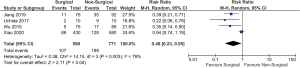
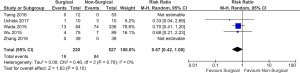
Atelectasis
Five studies that reported the risk of atelectasis were included in this meta-analysis (14,18,25,27,30). One study described lower events of atelectasis in nonoperatively treated patients (18), whereas four reported lower events of atelectasis in patients following SSRF (14,25,27,30). The overall pooled analysis found a statistically significant reduction in atelectasis in operatively treated patients with a RR of [RR: 0.44 (95% CI: 0.29 to 0.65), P<0.0001]. No heterogeneity (I2=0%) was reported (Figure 6).
ICU LOS
Five studies assessed ICU LOS in this meta-analysis (18,25,28,29,31). Four of these studies demonstrated that operatively treated patients had a substantially lower mean duration of ICU stay (18,25,28,31). The pooled estimation found a significantly [MD: –4.00 (95% CI: –6.33 to –1.66), P=0.0008] shorter ICU LOS in favor of surgical fixation compared with nonoperative treatment. High heterogeneity (I2=97%) was reported (Figure 7).
HLOS
Eight studies reported on HLOS (14,25-31). Seven of these studies showed a significantly lower mean duration of hospital stay (14,25-28,30,31). The overall pooled estimates showed that SSRF resulted in a significant reduction in hospital stay compared to the nonoperative group with a MD of –6.54 (95% CI: –9.28 to –3.79, P<0.00001). Significantly high heterogeneity (I2=98%) was observed (Figure 7).
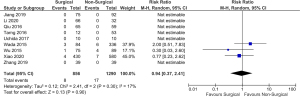
Need for tracheostomy
The need for tracheostomy was reported in five studies (3,18,26,28,31). The pooled analysis revealed that surgical fixation was associated with a nonsignificant [RR: 0.67 (95% CI: 0.42 to 1.08), P=0.10] reduction in the need for tracheostomy compared to nonoperatively treated patients. No heterogeneity (I2=0%) was observed for this analysis (Figure 8).
Risk of mortality
Nine studies reported mortality events (3,6,14,18,26,28-31). The pooled estimate suggested no statistically significant difference in mortality between the SSRF and nonoperative groups [RR: 0.94 (95% CI: 0.37 to 2.41), P=0.90]. Low heterogeneity (I2=17%) was found for this analysis (Figure 9).
Narrative review of other outcomes not included in the meta-analysis
Posttreatment complications and malformations
In the study by Xiong et al. [2019] (27), the number of patients with sternal malformation in the SSRF group was smaller than that in the nonoperative group. However, this difference was not statistically significant (P=0.295). Other studies by Li et al. [2020] (6), Uchida et al. [2017] (18), and Tarng et al. [2016] (31) were consistent in reporting that all surgical operations were uneventful, and no surgical complications were recorded.
QoL
Six studies reported outcomes related to QoL. The results showed better functional QoL in the surgical fixation cohort. Li et al. [2020] (6) reported a shorter duration to perform moderate to severe physical labor (5.4 vs. 5.8 months), shorter time to restore daily selfcare (0.9 vs. 1.2 months), lower duration of chest discomfort (1.1 vs. 2.9 months), less time to perform mental labor (1.9 vs. 2.8 months) and overall improvement in QoL in surgically fixated patients compared to the nonoperative group. Lung function indicators were also reported and measured prior to discharge in the SSRF and nonoperative group. The vital capacity (VC) and forced expiratory volume in one second (FEV1) in the surgical group showed significant improvement over the nonoperative group (P<0.05). No significant differences (P>0.05) in indicators of pulmonary function [VC: 31.0% vs. 26.5%; FEV1: 29.9% vs. 26.7%; peak expiratory flow (PEF): 15.2% vs. 12.0%] were found between the surgical and nonoperative groups at the time of admission. Uchida et al. [2017] (18) showed that surgically fixated patients could be promptly weaned from mechanical ventilation and could be extubated within 24 hours after surgery. Furthermore, the respiratory functions of both patients with flail chest and those with multiple rib fractures improved significantly from 25 breaths/min preoperatively vs. 15 breaths/min postoperatively (P=0.005) and a tidal volume of 400 mL preoperatively vs. 480 mL postoperatively (P=0.008). Qiu et al. [2016] reported that after 2 months of follow-up, operatively treated patients were able to return to normal activity sooner than the nonoperative group (28.18±9.21 vs. 42.42±10.12 days, P=0.028) (14). Zhang et al. [2019] (3) reported a significantly higher level of physical activity in the SSRF group (69.23% vs. 48.72%, P<0.05). After 6 months, there was a higher rate of preinjury work in the SSRF group than in the nonoperative group (94.87% vs. 64.10%). Similarly, there was a higher QoL score in the surgery group at both 3 months and 6 months post-operative follow-up in comparison to the nonoperative group (P<0.05). Another study by Jiang et al. [2019] (30) reported a significantly lower number of SSRF patients who experienced post physical activity chest tightness (14.7%) and thoracic deformity (10.7%) at the 3-month post-operative follow-up than the nonoperative group (39.1%, 37% and 41.3%, respectively; all P<0.05). Khandelwal et al. [2011] (24) reported that the operative group had a shorter duration of return to normal activities (26.2 vs. 54.21 days).
Discussion
Key findings
In this study, SSRF of patients with mainly non-flail multiple rib fracture resulted in a statistically significant shorter DMV, lower pain scores, reduced risk of atelectasis and pneumonia and reduced ICU LOS and HLOS compared to nonoperative treatment. However, there were no significant differences between treatment groups in the risk of mortality.
Strengths and limitations
The strength of this meta-analysis is that almost all the studies were consistent in the direction of observed benefit in favor of the SSRF group. Meanwhile, it has several limitations. First, the studies are heterogeneous, which we anticipate when pooling observational studies. The heterogeneity may be attributed to differences in patient characteristics, sample size, study quality, assessment of outcomes, and characteristics of intervention. This observed heterogeneity resulted in varying magnitudes of effect size among studies. However, the studies are consistent in having effect measures that favor the SSRF group. This makes us confident in the results of our meta-analysis, which indicate that SSRF might be of benefit in the treatment algorithm of patients with multiple non-flail rib fractures. Given the nature of the interventions being compared and the condition being studied, it is unlikely that RCTs will be conducted to draw a conclusion. Hence, the inclusion of observational studies in this meta-analysis may lead to a more robust conclusion. This is supported by Choi and associates in their Bayesian meta-analysis, which included both observational studies and RCTs. Conventional meta-analyses commonly exclude observational studies since these have lower level of evidence than RCTs. However, this compromises the number of patients that contribute data to the overall evidence especially when majority of the available studies are observational in design (32). The recommendations presented in the literature for the use of real-world evidence in meta-analyses were exercised in the conduct of this study. The range of I2 values observed in the current study was consistent with other meta-analyses (0–97% and 0–95%, respectively). Another limitation is that baseline health condition or severity of other injuries or trauma are not reported in detail among studies. This is a possible confounding factor since patients who had worse or more severe health conditions can be intentionally assigned to receive nonoperative treatment due to being unstable for surgery. Also, mortality from thoracic trauma can be largely influenced by intra- (and extra-) thoracic concomitant injuries such as injury to the pericardial region. Additionally, a higher percentage of patients with flail chest were in the nonoperative group. This could result in less favorable outcomes in the nonoperative group as compared to their less injured counterparts in the operative group. Finally, the small sample size in some of the studies, wide CIs, and the non-randomized selection of subjects may be threats to the generalizability of our findings.
Comparison with similar research
The findings from this study agree with the results of previous publications. However, very few studies, especially systematic reviews and meta-analyses, have focused on non-flail rib fractures in the Asian population. In a retrospective study, Zhang et al. [2019] (3) evaluated the efficacy of surgical fixation for patients with severe non-flail rib fractures and showed significantly lower pain scores. Similarly, Pieracci et al. [2020] (7) conducted a prospective controlled clinical trial and found that surgical fixation of non-flail rib fractures significantly reduced the 2-week numeric pain score and improved the respiratory disability-related quality of life (RD-QoL).
Several systematic reviews and meta-analyses further support the results of the current study despite only having patients with flail chest. Beks et al. [2019] (33) presented current evidence on the outcome after surgical rib fixation in both flail and non-flail patients and found that surgical fixation significantly reduced mortality, ICU LOS, DMV, pneumonia, and tracheostomies. However, there were not enough data for non-flail patients to proceed with meta-analysis. A meta-analysis focusing on patients with a non-flail fracture pattern found that SSRF may result in a significant reduction of pneumonia, mortality, and HLOS as compared to nonoperative treatment. This study did, however, not specifically address a population type (34). To compare surgical fixation with nonoperative measures, Choi et al. [2021] (32) initiated a systematic review and Bayesian meta-analysis and revealed that SSRF was associated with reduced pulmonary complications and mortality compared with nonsurgical methods. Sawyer et al. [2022] (10) showed that SSRF significantly reduced ICU LOS, DMV, mortality, and risk of pneumonia. Furthermore, surgical fixation was best suited for flail chest patients, especially when performed within 72 hours of injury. Last, a recently concluded systematic review and meta-analysis by Craxford et al. [2022] (35) accentuates the current study’s results with a significantly reduced risk of pneumonia, DMV, and ICU LOS. A second systematic literature review and meta-analysis by Shiroff et al. [2022] (36) was published while this manuscript was being prepared. Their analysis of SSRF in patients with a majority of non-flail rib fractures was not specific to the Asian population; however, it concluded a shorter DMV, lower 2-week pain intensity and lower risk of atelectasis, respiratory complications and mortality compared to nonoperative treatment.
In a literature review performed by Raza et al. [2022] (37), consistent with our observations, it was observed that several cohort studies demonstrated better pain scores and QoL following SSRF as compared to nonoperative treatment. However, the authors mentioned that SSRF may not specifically benefit those with very high or very low pain scores.
More recently, a prospective multicenter RCT was conducted in Australia by Marasco et al. [2022] to compare rib fixation versus nonoperative treatment for non-flail fracture. They reported no differences in pain scores and QoL scores at 3 months after treatment. However, the return-to-work rates were better in the rib fixation group at 3 and 6 months after treatment. Their study population, however, is limited to non-ventilator-dependent patients (38). The result also may be affected by the following reasons: first, as the author mentioned, the randomization allocation in this study was impacted by a significant proportion of crossovers in both directions. In addition, the fixation proportion of rib fractures is only 50%. This may partially affect the pain control effect of the surgery.
Explanations of findings
Multiple non-flail rib fractures have been traditionally managed conservatively despite promising results in the medical literature. SSRF as compared to nonoperative management in the Asian population is associated with decreased DMV and rates of pneumonia, as well as lower HLOS, reduction in pain scores and need for tracheostomy, better range of motion in the thorax and fewer limitations in physical function (10,14,39,40).
Only four studies in this analysis reported that treatment groups also included patients with flail chest, which accounts for less than 20% of the cases in our study. This makes the findings representative of Asian patients with multiple non-flail rib fractures.
Implications and actions needed
Surgical fixation is effective in a cohort of Asian patients, with the majority having non-flail rib fractures. This finding is significant for understanding the clinical aspects of surgical rib fixation, which is not a common treatment option in Asia due to the lack of consensus on its effectiveness. Rib fractures are often encountered in blunt chest trauma and are associated with significant mortality and morbidity. Given our findings, SSRF should be considered as an effective and safe treatment for patients with multiple, severe rib fractures. Future studies should conduct clinical trials to validate our findings.
Conclusions
In conclusion, SSRF may be an effective treatment modality among Asian cohorts with multiple rib fractures characterized by mainly non-flail fracture patterns. This meta-analysis demonstrates shorter DMV, ICU LOS and HLOS, as well as a lower risk for atelectasis and pneumonia, and pain scores after 4 weeks following SSRF as compared to nonoperative treatment. The risk of mortality was similar between groups. The results must be interpreted with caution as high quality prospective studies are required.
Acknowledgments
We are grateful for the administrative and technical support provided by Anne Rossi and Yinghui Liu who work under Johnson & Johnson (JnJ), and helped initiate and complete this study. The abstract of this study has been previously presented (poster presentation) in The International Society for Pharmacoeconomics and Outcomes Research (ISPOR 2023).
Funding: This study was funded by
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1117/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1117/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1117/coif). All authors report that this study was funded by Johnson & Johnson (JnJ) for the conduct of literature search and statistical analysis, and payments were made to ClinChoice Inc. RS and SPA report that they are working with ClinChoice Inc. as contractor to JnJ at the time of the study. PG receives honoraria from Zimmer Biomet and DePuy Synthes for conducting training sessions (which includes discussing the risks and benefits of rib fixation) two to three times a year. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lafferty PM, Anavian J, Will RE, et al. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am 2011;93:97-110. [Crossref] [PubMed]
- Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev 2021;2:e580-92. [Crossref] [PubMed]
- Zhang JP, Sun L, Li WQ, et al. Surgical treatment ofpatients with severe non-flail chest rib fractures. World J Clin Cases 2019;7:3718-27. [Crossref] [PubMed]
- Martin TJ, Eltorai AS, Dunn R, et al. Clinical management of rib fractures and methods for prevention of pulmonary complications: A review. Injury 2019;50:1159-65. [Crossref] [PubMed]
- Senekjian L, Nirula R. Rib Fracture Fixation: Indications and Outcomes. Crit Care Clin 2017;33:153-65. [Crossref] [PubMed]
- Li Y, Gao E, Yang Y, et al. Comparison of minimally invasive surgery for non-flail chest rib fractures: a prospective cohort study. J Thorac Dis 2020;12:3706-14. [Crossref] [PubMed]
- Pieracci FM, Leasia K, Bauman Z, et al. A multicenter, prospective, controlled clinical trial of surgical stabilization of rib fractures in patients with severe, nonflail fracture patterns (Chest Wall Injury Society NONFLAIL). J Trauma Acute Care Surg 2020;88:249-57. [Crossref] [PubMed]
- Majercik S, Vijayakumar S, Olsen G, et al. Surgical stabilization of severe rib fractures decreases incidence of retained hemothorax and empyema. Am J Surg 2015;210:1112-6; discussion 1116-7. [Crossref] [PubMed]
- Talbot BS, Gange CP Jr, Chaturvedi A, et al. Traumatic Rib Injury: Patterns, Imaging Pitfalls, Complications, and Treatment. Radiographics 2017;37:628-51. [Crossref] [PubMed]
- Sawyer E, Wullschleger M, Muller N, et al. Surgical Rib Fixation of Multiple Rib Fractures and Flail Chest: A Systematic Review and Meta-analysis. J Surg Res 2022;276:221-34. [Crossref] [PubMed]
- Bemelman M, Poeze M, Blokhuis TJ, et al. Historic overview of treatment techniques for rib fractures and flail chest. Eur J Trauma Emerg Surg 2010;36:407-15. [Crossref] [PubMed]
- Jian X, Lei W, Yuyang P, et al. A new instrument for surgical stabilization of multiple rib fractures. J Int Med Res 2020;48:300060519877076. [Crossref] [PubMed]
- Liu T, Liu P, Chen J, et al. A Randomized Controlled Trial of Surgical Rib Fixation in Polytrauma Patients With Flail Chest. J Surg Res 2019;242:223-30. [Crossref] [PubMed]
- Qiu M, Shi Z, Xiao J, et al. Potential Benefits of Rib Fracture Fixation in Patients with Flail Chest and Multiple Non-flail Rib Fractures. Indian J Surg 2016;78:458-63. [Crossref] [PubMed]
- Xu JQ, Qiu PL, Yu RG, et al. Better short-term efficacy of treating severe flail chest with internal fixation surgery compared with conservative treatments. Eur J Med Res 2015;20:55. [Crossref] [PubMed]
- Zhang X, Guo Z, Zhao C, et al. Management of patients with flail chest by surgical fixation using claw-type titanium plate. J Cardiothorac Surg 2015;10:145. [Crossref] [PubMed]
- Shibahashi K, Sugiyama K, Okura Y, et al. Effect of surgical rib fixation for rib fracture on mortality: A multicenter, propensity score matching analysis. J Trauma Acute Care Surg 2019;87:599-605. [Crossref] [PubMed]
- Uchida K, Nishimura T, Takesada H, et al. Evaluation of efficacy and indications of surgical fixation for multiple rib fractures: a propensity-score matched analysis. Eur J Trauma Emerg Surg 2017;43:541-7. [Crossref] [PubMed]
- Liang YS, Yu KC, Wong CS, et al. Does Surgery Reduce the Risk of Complications Among Patients with Multiple Rib Fractures? A Meta-analysis. Clin Orthop Relat Res 2019;477:193-205. [Crossref] [PubMed]
- Granhed HP, Pazooki D. A feasibility study of 60 consecutive patients operated for unstable thoracic cage. J Trauma Manag Outcomes 2014;8:20. [Crossref] [PubMed]
- Hoepelman RJ, Beeres FJP, Beks RB, et al. Non-operative vs. operative treatment for multiple rib fractures after blunt thoracic trauma: a multicenter prospective cohort study. Eur J Trauma Emerg Surg 2023;49:461-71. [Crossref] [PubMed]
- Newhouse R, Dearholt S, Poe S, et al. Evidence-based practice: a practical approach to implementation. J Nurs Adm 2005;35:35-40. [Crossref] [PubMed]
- Johns Hopkins nursing evidence-based practice Johns Hopkins nursing evidence-based practice Sandra L Dearholt and Deborah Dang Sigma Theta Tau International £24.70 256pp 9781935476764 1935476769 Formula: see text. Nurs Manag (Harrow) 2012;19:8. [Crossref] [PubMed]
- Khandelwal G, Mathur RK, Shukla S, et al. A prospective single center study to assess the impact of surgical stabilization in patients with rib fracture. Int J Surg 2011;9:478-81. [Crossref] [PubMed]
- Liu Y, Xu S, Yu Q, et al. Surgical versus conservative therapy for multiple rib fractures: a retrospective analysis. Ann Transl Med 2018;6:439. [Crossref] [PubMed]
- Wada T, Yasunaga H, Inokuchi R, et al. Effectiveness of surgical rib fixation on prolonged mechanical ventilation in patients with traumatic rib fractures: A propensity score-matched analysis. J Crit Care 2015;30:1227-31. [Crossref] [PubMed]
- Xiong M, Hu W, Lou Q, et al. Efficacy of nickel-titanium memory alloy in the treatment of multiple rib fracture combined with sternal fracture. Exp Ther Med 2019;18:537-42. [Crossref] [PubMed]
- Wu WM, Yang Y, Gao ZL, et al. Which is better to multiple rib fractures, surgical treatment or conservative treatment? Int J Clin Exp Med 2015;8:7930-6.
- Xiao X, Zhang S, Yang J, et al. Surgical fixation of rib fractures decreases intensive care length of stay in flail chest patients. Ann Transl Med 2020;8:216. [Crossref] [PubMed]
- Jiang Y, Wang X, Teng L, et al. Comparison of the Effectiveness of Surgical Versus Nonsurgical Treatment for Multiple Rib Fractures Accompanied with Pulmonary Contusion. Ann Thorac Cardiovasc Surg 2019;25:185-91. [Crossref] [PubMed]
- Tarng YW, Liu YY, Huang FD, et al. The surgical stabilization of multiple rib fractures using titanium elastic nail in blunt chest trauma with acute respiratory failure. Surg Endosc 2016;30:388-95. [Crossref] [PubMed]
- Choi J, Gomez GI, Kaghazchi A, et al. Surgical Stabilization of Rib Fracture to Mitigate Pulmonary Complication and Mortality: A Systematic Review and Bayesian Meta-Analysis. J Am Coll Surg 2021;232:211-219.e2. [Crossref] [PubMed]
- Beks RB, Peek J, de Jong MB, et al. Fixation of flail chest or multiple rib fractures: current evidence and how to proceed. A systematic review and meta-analysis. Eur J Trauma Emerg Surg 2019;45:631-44. [Crossref] [PubMed]
- Wijffels MME, Prins JTH, Perpetua Alvino EJ, et al. Operative versus nonoperative treatment of multiple simple rib fractures: A systematic review and meta-analysis. Injury 2020;51:2368-78. [Crossref] [PubMed]
- Craxford S, Owyang D, Marson B, et al. Surgical management of rib fractures after blunt trauma: a systematic review and meta-analysis of randomised controlled trials. Ann R Coll Surg Engl 2022;104:249-56. [Crossref] [PubMed]
- Shiroff AM, Wolf S, Wu A, Vanderkarr M, et al. Surgical Fixation of Severe Rib Fractures: A Systematic Literature Review and Meta-Analysis. Arch Orthop 2022;3:33-46.
- Raza S, Eckhaus J. Does surgical fixation improve pain and quality of life in patients with non-flail rib fractures? A best evidence topic review. Interact Cardiovasc Thorac Surg 2022;35:ivac214. [Crossref] [PubMed]
- Marasco SF, Balogh ZJ, Wullschleger ME, et al. Rib fixation in non-ventilator-dependent chest wall injuries: A prospective randomized trial. J Trauma Acute Care Surg 2022;92:1047-53. [Crossref] [PubMed]
- Fagevik Olsén M, Slobo M, Klarin L, et al. Physical function and pain after surgical or conservative management of multiple rib fractures - a follow-up study. Scand J Trauma Resusc Emerg Med 2016;24:128. [Crossref] [PubMed]
- Lodhia JV, Konstantinidis K, Papagiannopoulos K. Surgical management of multiple rib fractures/flail chest. J Thorac Dis 2019;11:1668-75. [Crossref] [PubMed]


