Right, middle, and lower bronchial sleeve lobectomy by video-assisted thoracic surgery
Introduction
Surgical treatment remains the most effective approach to extending the long-term survival of patients with lung cancer (1). However, for tumors that have already invaded the orifice of upper lobe bronchus and/or main bronchus, lobectomy alone can not completely remove the tumors, whereas pneumonectomy will severely damage the lung functions. On the contrary, bronchial sleeve lobectomy is featured by not only the maximal resection of tumors but also the maximal reservation of the normal lung tissues and lung functions and the remarkably decreased complications. Thus, it has shown good effectiveness in treating central-type lung cancer (2). The bronchial sleeve lobectomy extends the indications of lung cancer surgeries (3); When applied under thoracoscope, it can reduce the damage to the chest organs/tissues and the post-operative pain and therefore is particularly superior (4).
Clinical data
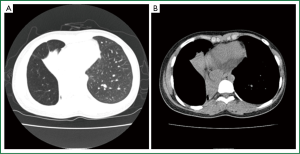
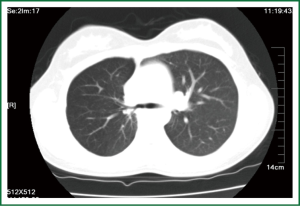
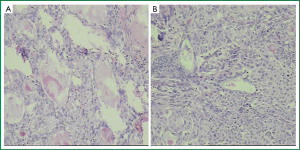
An 18 years old female patient was admitted on May 18, 2013 due to “heart palpitations on exertion with shortness of breath, occasionally accompanied with dry cough”. Chest computed tomography (CT) at admission showed right middle lobe atelectasis (Figure 1). Bronchoscopy displayed a mass at the orifice of right middle-lower bronchus. Pathology indicated the presence of “bronchial mucoepidermoid carcinoma” (Figure 2A). After the pre-operative preparation was well performed, he received right, middle, and lower bronchial sleeve lobectomy and lymph node dissection by video-assisted thoracic surgery (VATS) under general anesthesia (Video 1). During the surgery, obstructive atelectasis was seen in the right, middle and lower lung and excessive expansion seen in the right upper lung. Also, some paratracheal and subcarinal lymph nodes were found to be swollen. After the surgery, the tracheal stump was sent for pathologic examination, which showed no residual cancer. The post-operative pathology showed bronchial mucoepidermoid carcinoma (Figure 2B), whereas no metastasis was seen in lymph node stations 2, 4, 7, 8, 11, and 12. Anti-inflammatory and symptomatic treatment was provided after the surgery. The patient recovered well from the surgery and was discharged on the tenth post-operative day. One month later, the Chest CT scan showed right upper lobar inflation (Figure 3).
Pre-operative preparation
The patient underwent blood tests, urine analysis, ECG, and pulmonary function tests before the surgery to comprehensively evaluate the general conditions and his tolerance to the surgery. Informed consent was obtained before the surgery.
Surgical procedures
The patient was under general anesthesia with double-lumen endotracheal intubation. One lung ventilation of the healthy side was done when the patient was asked to take a supine position on the healthy side. A 1-cm incision was made at the sixth intercostal space on the right anterior axillary line as the observation port; A 5-cm incision was made at the fourth intercostal space on the anterior axillary line as the main operation port; And a 1-cm incision was made near the sixth intercostal space on the posterior axillary line as the auxiliary operation port. After the insertion of instruments, the mediastinal pleura of portopulmonary was dissected and the right inferior pulmonary ligament was disconnected. However, the hyperinflation of the lower right lung hampered the operation. Thus, the right, middle, and lower bronchi were dissected firstly and then transected, so as to relieve the hyperinflation of the lower right lung. The arteries and veins in the right, middle, and lower lungs were divided and then transected. The swollen lymph nodes in the hilum of lung were removed. End-to-end anastomosis of the right upper lobe bronchus to the main bronchus was performed using the prolene 3-0 suture. After the anastomosis, sterile water was injected into the thoracic cavity to find out if there was any gas leakage. A right lower chest tube was placed. Bronchoscopic sputum suction was performed. The condition of the anastomotic stoma was checked; Since it was patent, the incisions were then sutured.
Post-operative management
The post-operative management of patients who have undergone full thoracoscopic bronchial sleeve lobectomy is basically the same as those who have received conventional thoracoscopic lobectomy. It mainly includes adequate postoperative analgesia, prophylactic use of antibiotics, and resolving sputum. Effective expectoration and early ambulation should also be encouraged. A second chest X-ray showed good recruitment of the residual lung. The drain was electively removed when drainage was less than 100 mL/day.
Discussion
Currently the bronchial sleeve lobectomy is still based on the traditional open surgery. However, the open surgery-related trauma can severely affect the post-operative quality of life. Even worse, its damage to the respiratory muscles on the chest wall can increase the perioperative mortality. However, in some patients with central lung cancer, bronchial sleeve lobectomy can achieve an effectiveness similar as the pneumonectomy, and meanwhile can achieve the maximal reservation of the post-operative lung functions, improve the quality of life, and extend the survival (5). The min-invasive bronchial or vascular sleeve lobectomy by VATS can minimize the above problems. However, the full thoracoscopic surgery can be challenging for the operators. The bronchial sleeve lobectomy should only be performed by thoracic surgeons who have been well trained in laparoscopic techniques in carefully selected patients to ensure the safety.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ohta M, Sawabata N, Maeda H, et al. Efficacy and safety of tracheobronchoplasty after induction therapy for locally advanced lung cancer. J Thorac Cardiovasc Surg 2003;125:96-100. [PubMed]
- Maurizi G, D’Andrilli A, Anile M, et al. Sleeve lobectomy compared with pneumonectomy after induction therapy for non-small-cell lung cancer. J Thorac Oncol 2013;8:637-43. [PubMed]
- Okada M, Yamagishi H, Satake S, et al. Survival related to lymph node involvement in lung cancer after sleeve lobectomy compared with pneumonectomy. J Thorac Cardiovasc Surg 2000;119:814-9. [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [PubMed]
- Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32:20-8. [PubMed]